This week, our In Focus section highlights an article, Digitally Driven Integrated Primary Care and Behavioral Health: How Technology Can Expand Access to Effective Treatment, published in the Current Psychiatry Report, was co-authored by HMA Principals Lori Raney, MD and David Bergman, MPA, as well as John Torous, MD, and Michael Hasselberg, M.S., Ph.D. Together, they addressed how technology solutions can be utilized for more widespread implementation of effective integrated primary care and behavior health.
The article deconstructs the four core principals of effective integrated care, team-based care, evidence-based care, measurement-based care, and population-based care, to identify the critical tasks. Several of the tasks related to these core principles are adaptable to technology.
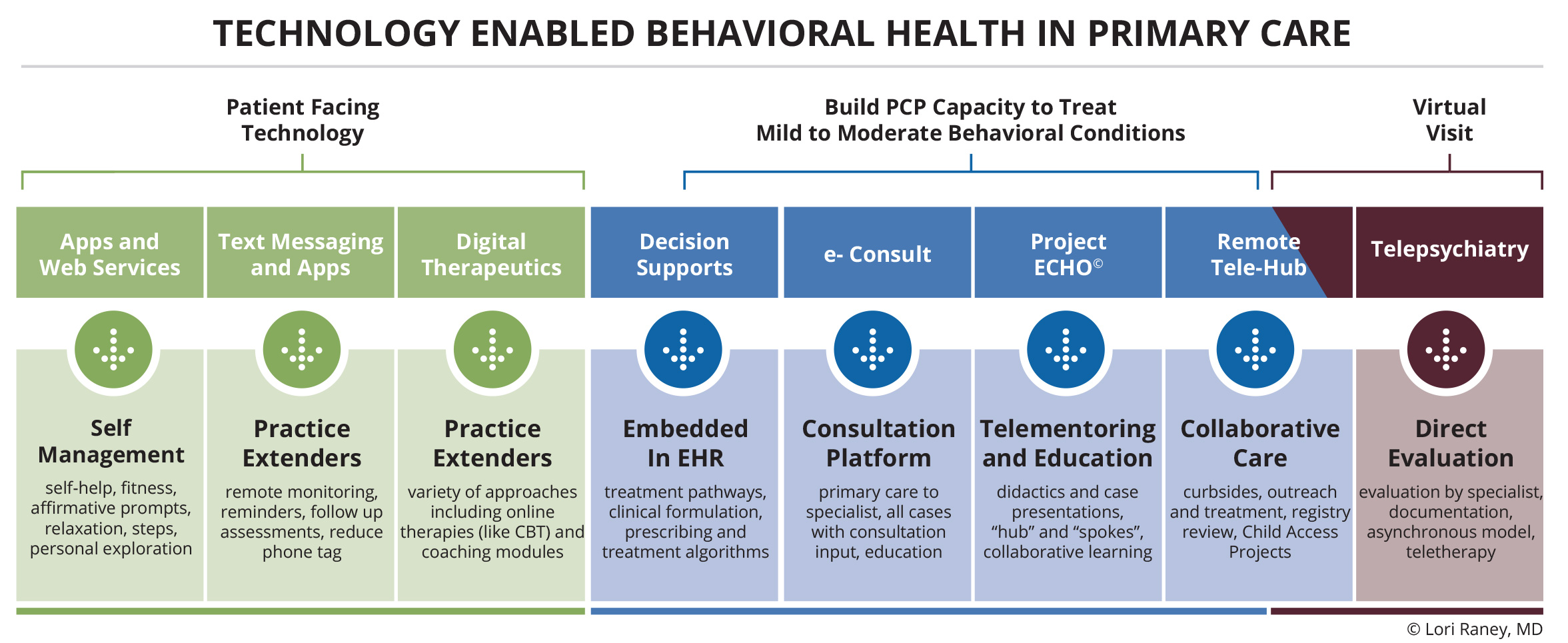
There are many different technologies available including: patient-facing tools, technologies that help to build the knowledge and skills of primary care providers (PCPs), and virtual care. Patient-facing tools allow self-management of symptoms and serve as “practice extenders” for the team. When digital approaches help build the knowledge and skills of PCPs, it can increase their capacity to treat mild to moderate mental illness in the primary care setting. Virtual care can provide telepsychiatry and other behavioral health specialty services remotely.
Building the capacity for PCPs to treat behavioral health conditions in primary care settings is done in many ways. Clinical decision supports enhance health-related decisions using the right channels, like electronic health records. Electronic consultation or eConsults can provide enhanced communications between PCPs and specialists regarding treatment in the referral process. Psychiatric Project ECHO (Extensions of Community Healthcare Outcomes) allows PCPs telementoring and collaborative learning for the treatment of behavioral health conditions. Remote tele-hubs can provide behavioral healthcare for sites that would not otherwise have access due to lack of workforce, patient populations or resources. While virtual visits do not solve the workforce shortage problem, they can help with the geographical maldistribution of behavioral health providers.
The major obstacles to widespread implementation of traditional integration of primary care and behavioral health models can be attributed to workforce shortages, competencies to deliver evidence-based approaches, and inadequate reimbursement. Digital solutions—alone and in combination—are showing some promise in integrating care, and technology developers will need to understand the current evidence base for effective integration efforts. With this understanding, key tasks that could be adapted with technology can be used to develop new and revised solutions. The use of these technologies is a growing area of research and development that warrants further investigation, particularly as multiple approaches are increasingly being used together. This article explores the evidence base and breaks down the key tasks that along with human support could help extend behavioral health expertise to larger populations in need.
Read more in the Current Psychiatry Report: http://rdcu.be/wlmr