This week, our In Focus reviews requests for proposals (RFPs) for Minnesota’s Medicaid managed care programs: 1. Families and Children Medical Assistance and MinnesotaCare; 2. Minnesota Senior Care Plus (MSC+)/Minnesota Senior Health Options (MSHO). The two RFPs were released by the Minnesota Department of Human Services on February 25, 2019, with implementation scheduled to begin on January 1, 2020 for all programs.
Families and Children Medical Assistance and MinnesotaCare
Minnesota’s Medical Assistance program provides Medicaid services for low income individuals, while MinnesotaCare provides health care services to individuals at 138 percent to 200 percent of the federal poverty level, funded by a provider tax, Basic Health Program funding, and enrollee premiums/cost sharing. The Families and Children Medical Assistance and MinnesotaCare RFP will provide services in 80 Minnesota counties, excluding seven metro areas: Anoka, Carver, Dakota, Hennepin, Ramsey, Scott, and Washington. A separate procurement will be released for these counties at a later date. For Families and Children, the state will choose at least two managed care organizations (MCOs) to provide services in counties identified as metro areas – Chisago, Olmsted, Rice, Sherburne, Stearns and Wright. The State will determine the number of MCOs in the remaining counties. For MinnesotaCare, at least two MCOs will be selected for all 80 counties in the RFP. HMA estimates that the contracts are worth approximately $2.1 billion.
Eligibility
The following individuals will be eligible for services:
- Medical Assistance/Pregnant women
- Medical Assistance/Children under 21
- Medical Assistance/Adults with children
- Medical Assistance/Adults without children
- MinnesotaCare enrollees
Additionally, adults who are seriously and persistently mentally ill (SPMI) and eligible to receive Medical Assistance-covered mental health targeted case management services; children who are severely emotionally disturbed (SED) and eligible to receive Medical Assistance-covered mental health targeted case management services; and children receiving Medical Assistance through adoption assistance can voluntarily enroll.
Projected Enrollment
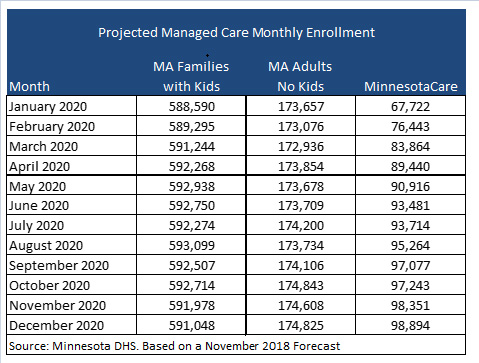
Minnesota predicts that when the new contracts start in January 2020, 588,590 will be eligible for Families and Children and 67,722 will be eligible for MinnesotaCare.
Senior Health Options and Senior Care Plus
Minnesota’s Senior Health Options program provides Medicare-Medical Assistance (Medicare and Medicaid) integrated care to dually eligible individuals, while the Minnesota Senior Care Plus program provides Medical Assistance health care and long-term care services. The RFP applies to all 87 counties. Plans that provide MSHO will also be required to provide MSC+ in the same county. HMA estimates that the contracts are worth $2.4 billion.
Eligibility
The following individuals are eligible for MSHO:
- 65 years of age or older
- Eligible for Medical Assistance and Medicare Parts A and B
- Eligible to enroll in MSC+ (unless they are eligible for MSHO, but are not required to enroll in MSC+ due to a Spenddown)
The following individuals are eligible for MSC+:
- 65 years of age or older
- Eligible for Medical Assistance without a medical spenddown
- The following populations may also be eligible:
- Nursing Facility and Community Residents
- Hospice
- End Stage Renal Disease (ESRD)
Adults aged 65 or older who have serious and persistent mental illness (SPMI) and who are eligible to receive Medical Assistance mental health targeted case management services can voluntarily enroll in MSHO and MSC+.
Projected Enrollment
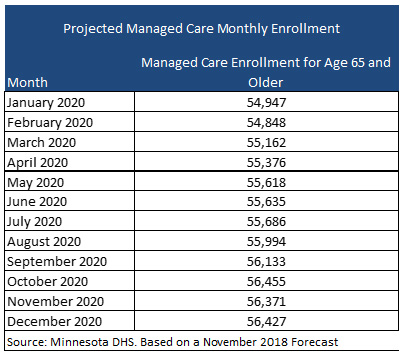
Minnesota projects that the managed care enrollment for people ages 65 and older will be 54,947 when the new contracts start in January 2020.
Evaluation
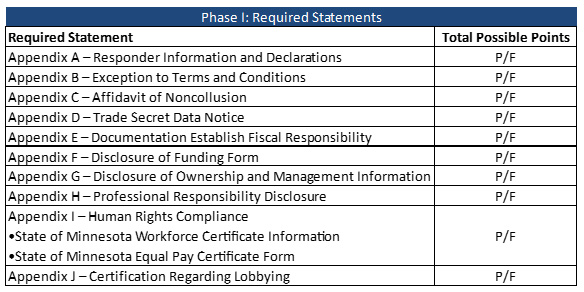
Plans will be evaluated in three phases. In Phase I, the Required Statements will be scored on a pass/fail basis. If any statement fails, the plan will not move on to Phase II. In Phase II, the Technical Requirements are evaluated. Components will be scored and then multiplied by a point factor rating. MA Families and Children/MinnesotaCare plans must receive a total score of 50 or higher to move to Phase III. MSHO/MSC+ plans must score 75 or more to move on.
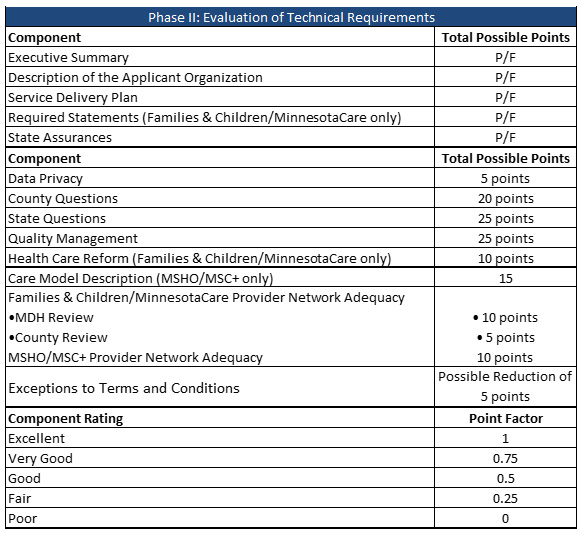
In Phase III, the state will select the successful responders. The evaluation team will review the scoring in making its recommendations, as well as other factors including:
- Can serve most or all of the counties in the geographic area
- Ability to accept all enrollment for the county
- Completeness of the response and ability to meet all requirements contained in this RFP, which includes providing all health care services and tasks required in the current model contract
- Number of potential responders and availability of providers in the responder’s service areas
- Access to, and availability of covered services that meets community needs, such as public health goals
- Consideration of transitions of members between programs
RFP Timeline
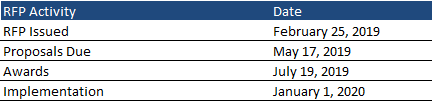
Contracts for both procurements are expected to run from January 1, 2020, through December 31, 2020, with up to five optional years. Proposals are due May 17, 2019, and awards will be announced July 19, 2019.
Current Market
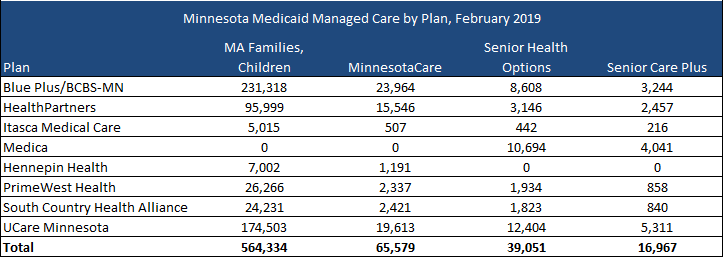
As of February 2019, Minnesota had approximately 906,000 Medicaid managed care members. The MA Families and Children program had 564,334, MinnesotaCare 65,579, Senior Health Options 39,051, and Senior Care Plus 16,967. Blue Plus has the largest market share for Families and Children/MinnesotaCare, while UCare Minnesota had the largest market share for Minnesota Senior Health Options/Senior Care Plus.