This week, our In Focus section reviews the Medicaid managed care procurement landscape for 2017, including those requests for proposals (RFPs) and other procurement vehicles that were awarded, are currently out to bid, or are expected to be released before the end of the calendar year. By year’s end, we anticipate there will have been at least 16 procurements awarded or issued this year across 13 states, covering more than 13 million Medicaid or CHIP members, and accounting for more than $76 billion in annual spending when fully implemented.
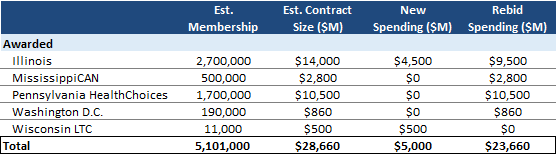
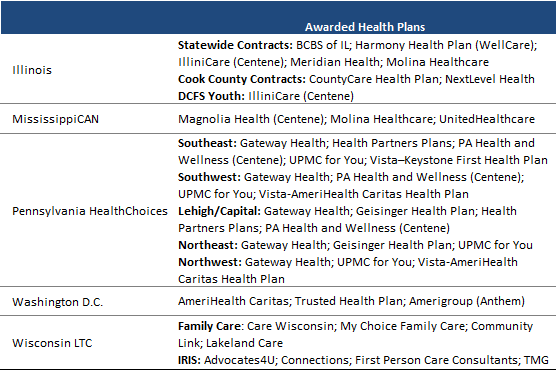
Medicaid Managed Care Awards in 2017
So far in 2017, there have been five Medicaid managed care awards, the most significant being the Illinois rebid and statewide expansion (2.7 million members, $14 billion annual spend), and the Pennsylvania HealthChoices rebid (1.7 million members, $10.5 billion annual spend). Pennsylvania contract awards have been announced, but are still pending the outcome of the protest process.
Medicaid Procurements Currently Underway
There are seven procurements currently in various stages of the process, with Massachusetts (850,000 members, $7.1 billion annual spend) set to announce awards any day now. Delaware’s procurement (200,000 members, $1.7 billion annual spend) allowed for the option to award, but did not require it; the state may elect to use the responses to the request for qualifications to inform a later procurement. Texas CHIP (rural service areas only – 85,000 members, $250 million annual spend) is also expected to be announced before the end of the year, while Florida (combined 3.1 million members, $15 billion annual spend) and New Mexico awards (700,000 members, $4.5 billion annual spend) are expected in the first half 2018. Virginia’s Medallion 4.0 procurement (700,000 members, $3.5 billion annual spend) did not target an award date; however, contracts are scheduled to be implemented August 1, 2018.
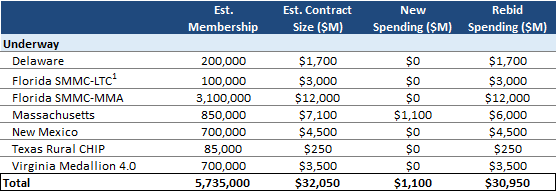
1 FL LTC membership excluded from total as already counted in MMA
Medicaid Procurements Expected by End of 2017
There are a further four states expected to release meaningful Medicaid managed care procurements before the end of the year. The largest of the four being Arizona’s Acute Care program rebid (1.6 million members), followed by the Texas STAR+PLUS rebid (530,000 members), which includes long-term services and supports (LTSS). Not included in this list is the potential Alabama Integrated Care Network procurement for individuals with LTSS needs, which has been delayed pending a revised timeline.
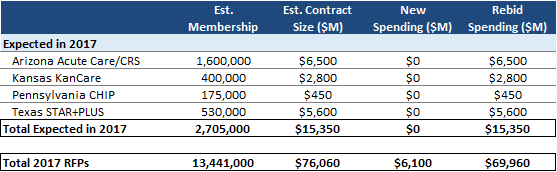
2017’s procurement activity, both in contract awards and procurements issued, is estimated to impact 13.4 million beneficiaries, more than 20 percent of the roughly 55 million Medicaid managed care beneficiaries nationwide. Procurement activity in 2017 will result in the rebid of roughly $70 billion in current annual Medicaid managed care spending, and will result in an estimated $6.1 billion in new managed care spending when fully implemented.
Look Ahead to 2018 Medicaid Managed Care Activity
Both New Hampshire (~160,000 members) and North Carolina (1.8 million members) have concretely indicated plans to release Medicaid managed care procurements in the first half of 2018, New Hampshire’s to rebid the existing program, while North Carolina will represent one of the most significant new Medicaid managed care opportunities in years. Texas is also very likely to release a reprocurement for the STAR program (2.9 million members) and potentially the CHIP program (425,000 members) in 2018, as the state indicated its intentions to align all Medicaid managed care program start dates to September 1, 2019. North Carolina and Texas STAR alone would account for nearly 5 million Medicaid managed care beneficiaries out to bid.
Beyond these opportunities, there are a number of states that could potentially see procurement activity in 2018 based on contract timing and other factors. These potential opportunities include:
- Louisiana (1.46 million members) – Louisiana is in the process of reviewing current MCO contracts; a decision on whether to extend beyond 2018 contract term is expected in coming weeks.
- Puerto Rico (1.6 million members) – Puerto Rico’s MiSalud managed care contracts technically expire in 2018, but are likely to be extended through May of 2019. Based on this timeframe, a 2018 procurement is highly likely.
- Washington (1.6 million members) – Washington is in the process of transitioning to Fully Integrated Managed Care statewide, with a goal of full implementation by 2020. So far, two regions – North Central (66,000 members) and Southwest (110,000 members) – have been procured, with the rest of the state to be procured on a regional basis in the coming years.