This week, our In Focus section, written by HMA Principal Denise Soffel, reviews New York’s Medicaid Redesign Team Structural Roadmap: Roles and Responsibilities in a Value Based Payment World, released by the state’s Department of Health on March 19, 2018.
New York is committed to the transformation of its health care delivery system. Its Delivery System Reform Incentive Payment (DSRIP) program envisions a significant shift to community-based care, a more integrated delivery system, and a shift to value-based payment. A new document, released in draft form for public comment, lays out an ambitious objective: “New York seeks to make health care a team sport. The State seeks to forever banish the traditional silos that made care navigation for patients difficult and in some cases impossible.” (p. 13)
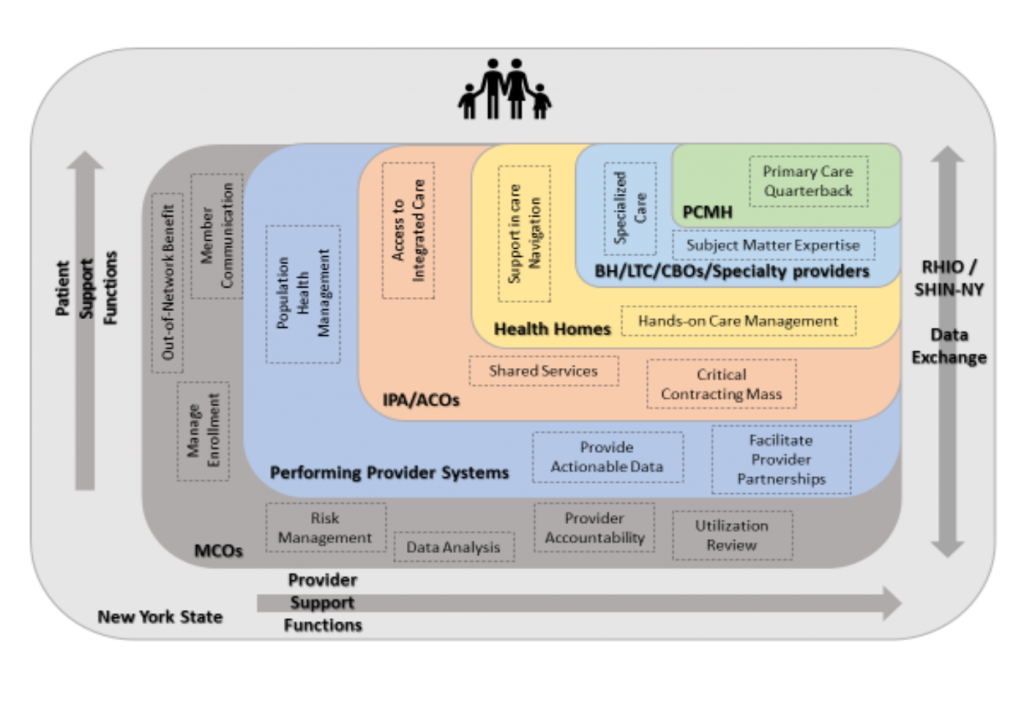
The draft document provides a structural roadmap of roles and responsibilities of various entities in a value-based payment environment. The document identifies a “middle layer” of actors that operate between the state as payer and the actual providers of care. This layer includes managed care plans, managed long-term care (MLTC) plans, health homes, performing provider systems (PPSs) currently participating in the DSRIP program, ACOs and IPAs, as well as patient-centered medical homes. These actors are seen as critical to ensuring cost-effective, high-quality care. The Structural Roadmap intends to define the various roles that middle level entities play in a value-based delivery system, where integrated networks replace disconnected service silos.
Missing from the Structural Roadmap is any discussion of social determinants of health and the role of community-based organizations in addressing those needs. The importance of addressing social determinants has been a central theme of New York’s health reform efforts, and the absence of a discussion about community-based organizations and their contribution to supporting population health efforts is a surprising omission.
The draft includes a chart that describes the functions of each of the layers that run between the state and the on-the-ground providers of care. Functions are categorized as either patient support or provider support.
| Layer | Patient Support Functions | Provider Support Functions |
| MCOs | Manage Enrollment, Out-of-Network Benefits, Member Communication | Risk Management, Data Analysis, Provider Accountability, Utilization Review |
| Performing Provider Systems | Population Health Management | Provider Actionable Data, Facilitate provider Partnerships |
| IPAs/ACOs | Access to Integrated Care | Shared Services, Critical Contracting Mass |
| Health Homes | Support in Care Navigation | Hands-on Care Management |
| BH/LTC/Specialty providers | Specialized Care | Subject Matter Expertise |
| PCMH | Primary Care Quarterback | |
Medicaid Managed Care Organizations
The Structural Roadmap envisions a smaller role for mainstream managed care organizations (MCOs) in the future. New York has relied on MCOs to provide care within the Medicaid program since its initial waiver was approved in 1996. Initially MCOs had a leading role in providing care coordination and case management to their members; in addition to capitation payments, they have received quality incentive bonus payments based on extensive performance metrics. Health homes now have primary responsibility for care management, based on a belief that they are better able to meet the needs of the highest-cost, highest-need Medicaid beneficiaries, who require a more intensive, comprehensive approach to care management than plans are able to provide. The Structural Roadmap identifies policies that will encourage MCOs to work more closely with their health home partners, including moving payment for health home services into the capitation rate and developing a Health Home Quality Performance and Management program, which will give MCOs health-home-specific performance data.
According to the Structural Roadmap, MCOs will remain involved in enrollment and member services, network development, and quality and utilization management. MCOs “will begin to delegate some risk, network development, and care management activities to increasingly sophisticated networks of providers that have been purposefully designed to better manage population health under VBP arrangements.” (p.2)
Since the DSRIP program began, much of the responsibility for identifying and responding to community health needs has shifted from MCOs to the 25 PPSs across the state, which have developed local networks of partners working collaboratively to “reform service delivery, address community health needs and reduce avoidable hospitalizations.” (p. 7) MCOs are expected to partner with PPSs to support value-based purchasing (VBP) arrangements, especially with data-sharing related to patient management, tracking, and quality improvement.
Managed Long Term Care
As described in the Structural Roadmap, MLTC plans will continue to have a significant role in providing care management to Medicaid beneficiaries requiring long term services and supports. They will also be involved in developing VBP initiatives by establishing relationships with and between providers and facilitating data sharing. The Structural Roadmap envisions MLTC plans playing a leading role in encouraging LTC providers to move to VBP arrangements and sharing best practices in care delivery, contracting, and quality measures.
Health Homes
Health Homes will be required to take full responsibility for care management for high-need beneficiaries. Given that MCOs can selectively contract with health homes, the health homes face competitive pressure to prioritize the quality of the care management services they provide through improved supervision and management of the care management agencies providing care on the ground. Health home care managers are responsible for closing all gaps in care needs of their members, assuring that members get the services they need, and that the services are coordinated effectively. Health homes also need to improve partnerships with MCOs in order to conduct successful outreach, aligning real time data and predictive risk modeling to better prioritize and target outreach activities. Health homes will be required to support MCO value-based purchasing goals by moving to value-based arrangements with progressive risk over time. In fact, health homes are required to enter into VBP arrangements with upside-only risk (at a minimum) by January 2019. It is unclear how care management needs for Medicaid beneficiaries who are not health home-eligible or who choose not to enroll in a health home will be met.
Performing Provider Systems
PPSs are beginning the fourth year of the five-year DSRIP program. They are expected by now to have developed deep population health management activities, including data management, patient tracking, practice redesign, community engagement, provider connectivity, and service integration (although the capacity of the PPSs varies across the state). PPSs are now in the process of developing a sustainability plan that describes how they will support on-going VBP implementation once DSRIP has ended. (Note that should a PPS decide not to continue post-DSRIP, it must describe how it will transfer its infrastructure to others in the community so as not to lose population health functional capacity). PPSs have the responsibility to develop a plan for working with MCOs, as well as with provider entities such as accountable care organizations, independent practice associations, and patient-centered medical homes, to maintain a population health facilitator function. It remains unclear whether all 25 PPSs will be able or willing to continue operations without ongoing funding once DSRIP ends in March 2020.
The state expects MCO and PPS partnerships will deepen to support providers as VBP rolls out. There will be an emphasis on data sharing as PPSs develop better real-time patient management, tracking, and quality improvement capabilities. These partnerships will also aid MCOs in improving quality and efficiency scores that affect payment.
Accountable Care Organizations and Independent Practice Associations
Providers are increasingly forming arrangements to facilitate providing accountable, value-based care, providing better population health management, and lowering cost. These organizations, which are occurring both horizontally and vertically, provide an asset to VBP contracting by allowing providers to take on risk contracting. MCOs are already working with these organizations; those relationships are likely to accelerate as behavioral health, specialty care, and long term care services become integrated into provider organizations.
Behavioral Health Care Collaboratives
Behavioral Health Care Collaboratives (BHCCs) are newly-established entities that establish provider networks that span various behavioral health silos, including mental health and alcohol and substance-use services. BHCCs are designed to integrate care across the entire spectrum of physical and behavioral health services. BHCCs are intended to help prepare providers for VBP by facilitating shared infrastructure and administrative capacity, as well as collective quality management. They should also encourage VBP payers, whether MCOs or providers, to partner with the BHCCs. BHCCs are receiving funding to build data-collection and data-analytic capacity, facilitating their participation in VBP.
Patient Centered Medical Home/Advanced Primary Care
New York began providing financial incentives to primary care practices that achieved National Committee for Quality Assurance (NCQA) recognition starting in 2010. Medicaid will begin a process this year that will reduce, and eventually eliminate, PCMH incentive payments for practices that opt not to participate in VBP arrangements with (at least) upside-only risk. Longer term, the state intends to limit PCMH incentive payments to practices that meet quality and efficiency targets.
SHIN-NY Support for DSRIP and VBP
New York has invested significantly in the development of the Statewide Health Information Network for New. It is meant to provide the health information exchange infrastructure necessary to support health care transformation initiatives. Eight Qualified Entities (QE) across the state are meant to support the exchange of electronic health record information. The state has been working with the QEs to help PPSs with data management and information exchange. QEs are supporting providers, PPSs and MCOs by making clinical data available for care management and quality measurement. QEs are also helping with consent management, which can be a major barrier to effectively implementing VBP. “Focusing on high-quality and easily available EHR information will support real-time, actionable, high-performing population health management.” (p. 12)
Care Delivery Layers
The following infographic is meant to display activities within the layer responsible for each activity, categorized as patient support (vertically) or provider support (horizontally)
The state is seeking public comment on the Structural Roadmap by April 2. Comments should be sent to [email protected].