This week, our In Focus reviews a case study called, “Spotlight on Health Center Payment Reform: Washington State’s FQHC Alternative Payment Methodology,” authored and prepared for the National Association of Community Health Centers by Health Management Associates’ Principal Art Jones and Senior Consultant Liz Arjun. The study, published in May 2018, looks at Washington’s fourth federally qualified health center (FQHC) Alternative Payment Model (APM4), implemented in July 2017.
Background
Washington adopted its initial FQHC APM in 2000 by inflating the FQHC Prospective Payment System (PPS) by a rate higher than the rate used nationally through a State Plan Amendment. As health care reform has continued to move away from fee-for-service, Washington State health centers became interested in developing FQHC APMs in partnership with their state Primary Care Association (PCA) and Medicaid agency that delink payment from the face-to-face visits through a primary care capitation approach with quality performance metrics.
APM4
Washington launched APM4 on July 1, 2017, with the state’s 16 of 27 FQHCs participating. The goal of the new model was to allow clinics to improve access to primary care by using the full care team and to provide alternative access beyond face-to-face visits with billable clinicians. This model enables primary care providers to manage a larger member panel without increasing their work load. This in turn increases the per practitioner revenue for his/her panel. The quality component assures that the transition from a fee-for-service to a capitated approach does not reduce access to primary care services. The APM4 model applies to Medicaid managed care enrollees only. In addition, it enhances their performance on other pay-for-quality and shared savings arrangements already in place with the health plans for the same population. The previous version, known as APM3, relied on face-to-face encounter fee-for-service payments without incentives for quality or efficiency.
Changes to the APM:
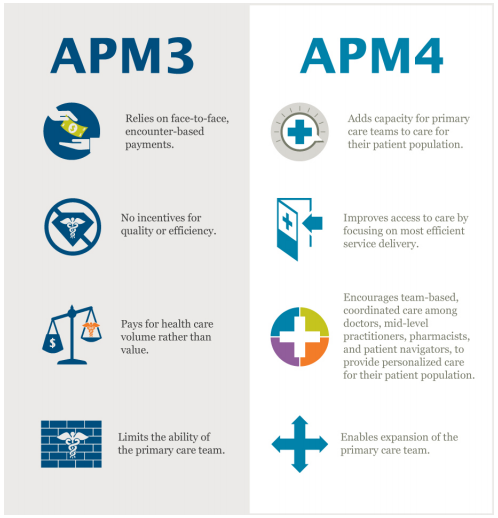
Source: Washington State Health Care Authority
Dental services, specialty mental health services, and services aimed at treating substance use disorder are carved out of APM4 reimbursement and will continue to be paid on a fee-for-service basis.
Rates
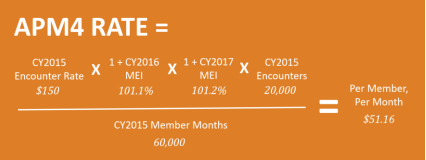
APM4 calculates an individual per member, per year (PMPY) budget neutral amount for each FQHC and pays that amount in a per member, per month (PMPM) amount. The PMPM is calculated by multiplying the FQHC’s encounter rate under APM3 times the total number of billable encounters to enrollees in Medicaid managed care and dividing that by total Medicaid managed care months. It trends the PMPM rate by the Medicare Economic Index (MEI) annually. The baseline PMPM rate is then carried forward in future years as long as quality targets are met. Quality targets are set for each FQHC individually based on improvement from their historical performance.
Example:
Quality Measures
APM4 uses a subset of the Washington State Common Metrics. Failure to meet these quality performance measures results in a prospective reduction of the PMPM payments. The PMPM rate will never go below encounter-based equivalent payment amounts. After being adjusted downward for failure to meet quality targets, clinics can earn back the full benefit of the baseline PMPM rate in the future (as trended by the MEI) upon meeting quality improvement targets.
- Comprehensive diabetes care – poor HbA1c control (>9%)
- Comprehensive diabetes care – blood pressure control (<140/90)
- Controlling high blood pressure (<140/90)
- Antidepressant medication management
- Effective acute phase treatment
- Effective continuation phase treatment (6 months)
- Childhood immunization status – combo 10
- Well-child visits in the 3rd, 4th, 5th and 6th years of life
- Medication management for people with asthma: medication compliance 50%
- (Ages 5-11)
- (Ages 12-18)
Program Monitoring
Although it is too early to gauge the success of the model, health centers are committed to working together with the Health Care Authority to address any future challenges. A small working group meets regularly to focus on:
- Quality performance measure reporting process and data validation sustainability
- The approach to reconciliation
- The change in scope process
- The health plan credentialing process
APM4 hopes to achieve improved access to primary care for individuals through a consumer-centric approach, not obtainable under a fee-for-service model.