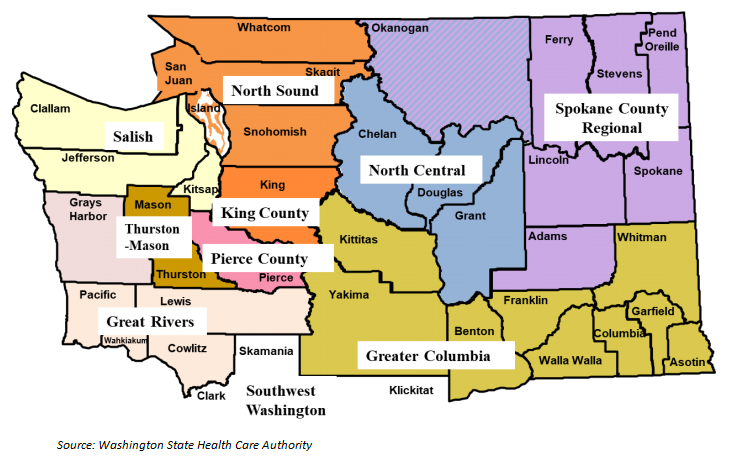
This week’s In Focus section reviews Washington’s 2019/2020 Integrated Managed Care (IMC) request for proposals (RFP) issued by the Washington State Health Care Authority (HCA) on February 15, 2018 to provide 1.6 million Medicaid enrollees with both physical and behavioral health services. The procurement will expand Washington’s Apple Health – IMC program (formerly known as Fully Integrated Managed Care (FIMC)) to eight additional Regional Service Areas (RSAs) and add an additional managed care organization to the Southwest RSA. It will also add one county to the Southwest RSA and one county to the North Central RSA.
Services and Populations Covered
Selected Medicaid Managed Care Organizations (MCOs) will provide the full continuum of physical and behavioral health, including primary care, pharmacy, mental health, and SUD treatment, to Medicaid enrollees. Most Medicaid enrollees will be enrolled in the IMC program, including current Apple Health managed care beneficiaries. Apple Health covers most populations, including individuals who are aged, blind, and disabled (ABD) and HCBS waiver beneficiaries. Those who are not eligible for managed care will receive Behavioral Health Services Only (BHSO) through the IMC contracts and will continue to receive their medical services through the state’s fee-for-service system. These include dual eligibles, individuals residing in an IMD (Institution for Mental Disease), medically needy spenddown enrollees, and pregnant women who are not citizens of the U.S.
Incumbent Behavioral Health Organizations (BHOs) will either cease operations or convert to a Behavioral Health Administrative Service Organization (BH-ASO) in regions where IMC is implemented. MCOs will be required to subcontract with BH-ASOs under the contract.
Foster care beneficiaries will remain enrolled in the current statewide foster care plan for physical health. Beginning on October 1, 2018, all behavioral health services will also be provided through that MCO. American Indian/Alaska Native (AI/AN) individuals may voluntarily opt into IMC. If they are not eligible for IMC, they can select BHSO with one of the IMC-contracted MCOs.
RFP Requirements
HCA is accepting bids only from MCOs with current Apple Health Medicaid Managed Care contracts.
Contract Awards
HCA anticipates awarding multiple contracts per RSA:
| Region | Number of MCOs |
| Greater Columbia | 5 |
| King | 5 |
| North Sound | 5 |
| Pierce | 4 |
| Spokane | 4 |
| Thurston-Mason | 3 |
| Great Rivers | 3 |
| Salish | 3 |
Additionally, HCA will select a third MCO to operate in the Southwest RSA. This region is already in the IMC program. Molina Healthcare and Community Health Plan of Washington are currently serving the Southwest RSA. In the Southwest region, the service area will also be expanded to include Klickitat County and in the North Central region, the service area will be expanded to include Okanogan County.
For regions choosing to implement IMC in 2019, contracts are set to begin on or about January 1, 2019 and end December 31, 2020. For regions choosing to implement IMC in 2020, contracts are set to begin on or about January 1, 2020 and to end on December 31, 2020. HCA can extend the contracts for up to two (2) additional one (1)-year periods.
Evaluation Criteria
MCOs will be evaluated based on combined scores on statewide and regionally-specific questions. Under some service areas, specific issues are identified in addition to general requirements. For example, a rural county may ask how a bidder will ensure clients have access to specific services. Counties with high homelessness rates can ask the bidder how they can develop affordable housing. Mandatory requirements, including medical and behavioral health networks, will be evaluated on a pass/fail basis.
| Evaluation Criteria | Maximum Points |
| RFP Compliance | N/A |
| Mandatory Management Review Letter of Submittal and Certification and Assurances | N/A |
| Statewide Evaluation Questions | 650 |
| (Management and Administration) | (105) |
| (Behavioral Health Network and Access) | (210) |
| (Quality and Utilization Management) | (105) |
| (Care Coordination) | (230) |
| 2019 Regional Questions | |
| Greater Columbia | 250 |
| King | 250 |
| North Sound | 250 |
| Pierce | 250 |
| Spokane | 250 |
| Provider Network | Pass/Fail |
RFP Timeline
MCOs are required to submit a mandatory letter of intent to propose by March 1. Proposals are due on April 12, with “Apparently Successful Bidders” selected on May 22, 2018. Contracts run for one year, with renewal options for two (2) one (1)-year periods.
| RFP Activity | Date |
| RFP Issued | February 15, 2018 |
| Mandatory LOI Due | March 1, 2018 |
| Proposals Due | April 12, 2018 |
| Awards | May 22, 2018 |
| 2019 Implementation | January 1, 2019 |
| 2020 Implementation | January 1, 2020 |
Current Medicaid Managed Care Market
Washington’s total managed care enrollment is 1.6 million. Molina Healthcare is the largest MCO, with over 45 percent of the market share.
| MCO | 2017 Enrollment | Market Share |
| Molina Health Care | 730,752 | 45.4% |
| Community Health Plan of WA | 278,038 | 17.3% |
| UnitedHealth/Optum Total | 234,774 | 14.6% |
| Coordinated Care Corp./Centene | 203,107 | 12.6% |
| Anthem/Amerigroup | 145,303 | 9.0% |
| Various Tribal/County Orgs | 16,057 | 1.0% |
| Total Managed Care | 1,608,031 |
Waivers
Washington’s Section 1115 Waiver, Medicaid Transformation Project (MTP), was approved by the Centers for Medicare & Medicaid Services (CMS) on January 9, 2017. The five-year waiver, worth $1.5 billion, integrates physical and behavioral health purchasing and service delivery, converts 90 percent of Medicaid provider payments to reward outcomes instead of volume, supports providers to adopt new payment and care models, implements population health strategies, and addresses key determinants of health.
Link to RFP/Bidders’ Library
RFP #2567 Integrated Managed Care (IMC) can be found in the Request for Proposals section.