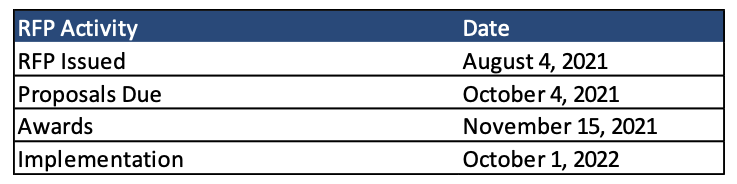
This week, our In Focus section reviews the Arizona Health Care Cost Containment System (AHCCCS) Competitive Contract Expansion (CCE) request for proposals (RFP), released on August 4, 2021. The procurement will expand the current AHCCCS Complete Care (ACC) Medicaid contracts to include responsibilities as an ACC Contractor (health plan) with a Regional Behavioral Health Agreement (ACC-RBHA). At least one incumbent Medicaid ACC Contractor will be selected in each of the state’s three Geographic Service Areas (GSAs). The responsibilities will include management of:
- An integrated Medicaid physical and behavioral health services benefit for individuals with serious mental illness (SMI),
- Non-Medicaid behavioral health services for children and adults, and
- A crisis system and services (ACC-RBHAs will jointly select and oversee a single statewide crisis phone vendor to operate a single, easy-to-use crisis phone line and crisis response system).
Implementation is slated to begin October 1, 2022.
Current ACC plans are:
- Health Choice Arizona (subsidiary of Blue Cross Blue Shield of Arizona)
- Banner University Family Care
- Arizona Complete Health (subsidiary of Centene)
- Care 1st Health Plan (subsidiary of Centene)
- Mercy Care Plan,
- Molina Complete Care
- UnitedHealthcare Community Plan
ACC plans provide physical health and behavioral health services to Medicaid members, including adults with General Mental Health/Substance Use (GMH/SU) needs and children, including those with Special Health Care Needs (SHCN).
Plans must already serve the GSA in order to win the expanded contracted in that GSA. For example, only plans that already serve the North GSA will be eligible to bid for the CCE in the North GSA. ACC plans will not be awarded more than two of the three GSAs.
Winning plans will need to implement Whole Personal Care Initiative (WPCI) strategies, including addressing Social Determinants of Health (SDOH) and utilizing the Statewide Closed-Loop Referral System (CLRS). Plans will actively promote provider network utilization of the CLRS to properly refer members to Community Based Organizations (CBOs) providing services addressing social risk factors of health.
Additionally, plans will use health information technology in electronic health records (EHRs), e-prescribing, and a Health Information Exchange (HIE) infrastructure. They will be required to contract with the state designated Health Information Exchange (HIE) organization, Health Current, a non-profit organization which provides a secure network for the exchange of clinical health information.
Background
The procurement will replace the state’s current Regional Behavioral Health Authorities (RBHAs) with ACC-RBHAs. AHCCCS currently contracts with three RBHAs –Arizona Complete Health (Centene), Mercy Care Plan, and Health Choice Arizona (Blue Cross Blue Shield of Arizona)– for behavioral health benefits for individuals with SMI. Other changes include in October 2021, the Arizona Behavioral Health Corporation began administering the AHCCCS Housing Program for individuals with mental health issues who are experiencing homelessness.
Below is each plan’s Medicaid SMI enrollment:
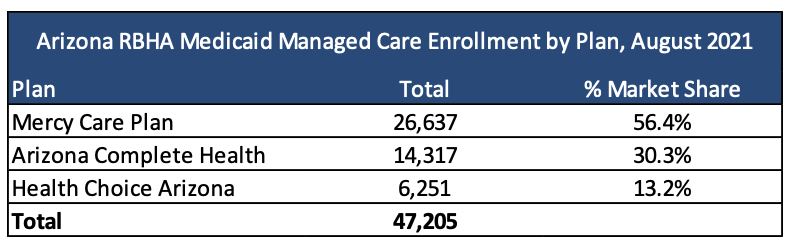
There will also be non-Medicaid grant funded program lives.
Timeline
Proposals are due October 4, 2021, with awards expected to be announced November 15, 2021.
For questions and additional RFP information, please contact HMA Senior Consultant Suzanne Rabideau.