Just one week after we reviewed the Senate’s version of the budget reconciliation bill, H.R. 1, President Trump has now signed the legislation into law. The final iteration of H.R. 1 includes sweeping changes to Medicaid, the Affordable Care Act (ACA) Marketplaces, and Medicare—several of which diverge significantly from the version that the House passed May 22, 2025.
This update outlines many of the most consequential healthcare provisions, with a focus on Medicaid financing, eligibility, and operational impacts. It also highlights how stakeholders can act now to prepare for what happens next.
From Proposal to Policy: What Changed
The Senate’s amended version of H.R. 1, approved on July 1 and passed by the House on July 3, 2025, reshaped several key provisions in the earlier version of the House bill. Although the bill retains its core focus on tax policy and entitlement reforms, it further constrains state Medicaid financing and eligibility and scales back Marketplace subsidies for certain populations.
According to preliminary analysis from the Congressional Budget Office, the final bill will reduce federal healthcare spending by approximately $1.15 trillion over the next decade but also will increase the number of uninsured individuals by 11.8 million by 2034 because of changes to both Medicaid and Marketplace programs.
Medicaid Eligibility: A New Era of Policy and Operational Complexity
Mandatory Community Engagement Requirements
By December 31, 2026, states must implement community engagement (work) requirements for certain Medicaid enrollees. These requirements cannot be waived under Section 1115, though states may request “good faith” exemptions through 2028.
States must notify enrollees through multiple channels and develop the infrastructure needed to track compliance. Managed care organizations and other entities that have financial relationships with Medicaid services are prohibited from determining compliance.
Tighter Eligibility and Redetermination Requirements
States must now conduct Medicaid eligibility redeterminations every six months for expansion populations. The bill also delays implementation of previously finalized rules that would have streamlined enrollment and imposes new verification requirements, including address checks. For immigrants, H.R. 1 narrows the definition of “qualified” individuals who are eligible for Medicaid and CHIP, removing coverage for refugees, asylees, and other humanitarian categories.
Cost Sharing for Expansion Adults
Starting in 2028, states must apply cost-sharing requirements to Medicaid expansion adults with incomes greater than 100 percent of the federal poverty level. Though primary care, mental health, and certain other services are exempt, the policy introduces new administrative burdens for states and many providers.
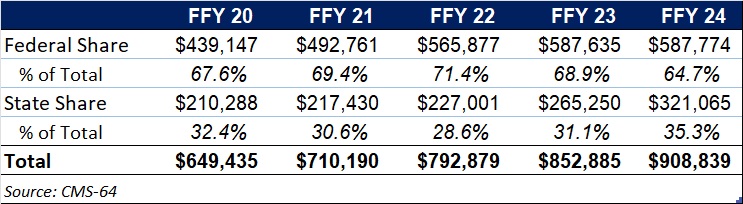
Medicaid Financing: A Structural Shift
Provider Tax Restrictions
H.R. 1 freezes existing provider tax programs and bars any new taxes. Also, Medicaid expansion states must phase down the maximum allowable tax rate from 6 percent to 3.5 percent by 2032. This change will significantly constrain states’ ability to use provider taxes to finance Medicaid and draw down federal matching funds.
Limits on State-Directed Payments
The bill caps state-directed payments at either 100 percent or 110 percent of Medicare rates, depending on the state’s expansion status. Grandfathered payment arrangements will be phased down by 10 percent annually beginning in 2028. These provisions will require states to reassess supplemental payment strategies and may affect provider participation and access to care.
Other Key Provisions
The Rural Health Transformation Program provides $50 billion over five years to support financially distressed rural providers. H.R. 1 requires that each state submit a plan, and the Centers for Medicare & Medicaid Services (CMS) administrator must approve or deny the plan by December 31, 2025, giving CMS and the US Department of Health and Human Services significant authority to shape the approval/denial processes, as well as critical details of the program and funding decisions.
For the Marketplace, the law eliminates ACA subsidy eligibility for certain lawfully present immigrants, ends conditional eligibility for ACA subsidies as well as passive re-enrollment, and eliminates the cap on ACA subsidy repayment at tax time. It also prohibits individuals who are not enrolled in Medicaid because of a failure to satisfy community engagement requirements from receiving any subsidies.
In addition, a new 1915(c) waiver option allows states to offer home and community-based services (HCBS) without requiring that they provide institutional level of care but only if waiting lists for existing services are not extended. Another provision excludes family planning and abortion service providers from receiving Medicaid funding if they received at least $800,000 in Medicaid reimbursements in 2023.
Finally, the law includes a one-year, 2.5 percent increase to the Medicare physician fee schedule conversion factor, which will be in effect for calendar year 2026 and expire thereafter.
What Stakeholders Should Do Now
States can begin planning for eligibility system changes, redetermination volume, and community engagement implementation, all of which require an understanding of the potential interactions of the federal Medicaid, Medicare, and ACA Marketplace policy changes. In addition, state officials should consider reassessing provider tax structures and supplemental payment strategies, where applicable. They need to engage early on rural health transformation funding opportunities and other provider supports.
Health plans can forecast enrollment and risk mix changes. They have opportunities to support states in compliance efforts to avoid federal funding recoupments. In addition, plans must prepare for new administrative requirements related to cost sharing and work requirements, among other policy changes on the horizon. Consumer communications should also be a focus area.
Providers and community-based organizations will need to prepare for greater uncompensated care needs and costs, which can lead to potential revenue loss, as well as new reporting and program integrity expectations. They also will play an integral role in assisting patients in maintaining coverage and navigating new requirements.
Vendors and health information exchanges have several opportunities to support the implementation of new requirements in H.R. 1 alongside the changing regulatory priorities. Examples include reviewing system capabilities to support new eligibility, verification, and reporting requirements and coordinating with states to ensure smooth implementation and program integrity.
Looking Ahead
The passage of H.R. 1 marks a turning point in federal health policy. Although the law’s fiscal goals are clear, its operational impacts will unfold over the coming months and years. States, plans, providers, and community organizations must now pivot from policy analysis to implementation readiness.
HMA will continue to monitor federal guidance, state responses, and stakeholder strategies. For more detailed analysis or support with scenario planning, contact our experts below.