As reported by the New York Times (An Army of Virus Tracers Takes Shape in Massachusetts, April 17), Massachusetts has hired 1,000 public health contact tracers to speed containment of COVID-19 during its surge in infections. Contact tracers are reaching out to those who have tested positive, providing information, and talking them through their recent movements and connections, using cell phones and triangulation data. They then, in turn, reach out to inform and educate those contacts.
The article noted that “the idea of training a corps of contact tracers is emerging in many places at the same time, as leaders think ahead to the point when social-distancing constraints will be lifted.” Contact tracing has helped South Korea and Singapore contain the spread of the virus, although their efforts are informed by digital surveillance unavailable in the U.S. Massachusetts Governor Charlie Baker is quoted as saying, “It’s hard to see how we create a sense of safety if we don’t have a program like this in place…digital tracing may be integrated into the state’s program later, but human outreach is critical to reaching people without an easy way to isolate themselves.”
Additionally, a recent NPR report (How Do You Do Contact Tracing? Poor Countries Have Plenty Of Advice) reinforces the critical role of contact tracing as a standard practice to manage communicable diseases and “break epidemics” all around the world. The reporter shared a projection that 300,000 people will be needed for the contact tracing required to break the COVID-19 epidemic.
Local community based organizations are poised to provide this kind of outreach and engagement.
Today’s New York Times reports that Bloomberg Philanthropies has engaged a group called Vital Strategies to hire and train 4,000-5,000 people to serve as contact tracers. At HMA, we have supported numerous community-based organizations to complement public health initiatives such as the COVID-19 response.
Among these, HMA has supported several local communities and health networks to plan implementation of the Pathways Community HUB (HUB) model to activate and coordinate local community health workers. In this model, existing local human service organizations are coordinated to establish an organized network of community health workers (CHWs) who reach out to those at greatest risk, identify their risk factors, and ensure that they connect to medical, social, and behavioral health services. The HUB contracts with payers and funders of all types using a pay for performance methodology based on outcomes. Eleven certified HUBs are currently operational around the country, and many others are presently under development in Washington, Oregon, Michigan, Ohio, Pennsylvania, and New York.
Contact tracers are connecting with people who have been exposed to the virus, talking them through what they need to know about staying safe and helping others avoid contracting the virus, as well as supporting them to access needed services. In the same way, CHWs in a HUB network reach out to community members to identify and mitigate risks that lead to poor health outcomes.
The Pathways Community HUB Institute (PCHI) supports HUBs and payers. It has developed a COVID-19 learning module for CHWs, and supported CHWs to obtain consents and connect patients to telehealth services. It assists HUBs with data collection to inform planning and convenes a national network of HUB leaders to share ideas and problem-solve.
In response to COVID-19, health plans in Ohio are already paying HUBs for completed CHW visits conducted by phone. HUBs are also a go-to resource for local municipal planning to organize CHWs who can deliver groceries, medicine, and formula while also educating the public and assessing and tracking local gaps in the crisis response to both medical and social needs.
One HUB in Muskegon, Michigan is organizing shelter for the homeless who need a place to recuperate safely. A HUB in Summit County, Ohio is helping ill parents who require childcare arrangements and supporting local efforts to address the increased threat for those at risk of family violence. Others are reaching out to people whose addiction recovery may be vulnerable to social isolation and to people with disabilities and older adults whose risks from the virus require more targeted attention.
The recent news stories underscore the value of contact tracing in response to the pandemic and as a remedy for skyrocketing unemployment rates. HUBs are working to maintain employment for skilled CHWs able to support at-risk populations in a variety of ways, and they are also well positioned to administer and facilitate broader contact tracing efforts.
For more information, contact:
- Heidi Arthur at [email protected]
- Sarah Redding at [email protected]
*************************************************************************************
More Information
How the Pathways Community HUB Model Works
The HUB receives patient referrals directly from providers and other CBOs. CHWs are also always conducting outreach and identifying new individuals they can connect to care. The HUB ensures that families are only assigned one CHW by managing referrals within the network and across other care coordination programs and services within the region. They can act as extenders for MCO care management, offer outreach and connections to Health Home care management, and support providers of all types.
Payments to the CBOs are based on mitigated risk factors (confirmed outcomes) achieved by the CHW for each member of the family. This methodology incentivizes CHWs to find the highest risk patient clusters and rapidly connect them to services necessary to address their full array of health needs and social determinants. The 21 standard “risks” are called Pathways and have been refined over 20-plus years to comprehensively establish a whole person approach.
HUBs address individual AND community level risk factors in a pay for performance, quality improvement framework. HUB data is used to identify and address local gaps (e.g. establish new transportation support, priority access to housing for pregnant women, local aid for specific needs).
HUB data shared with the delivery system, and vice versa, will inform contracting, target outreach efforts, and build the case for other needed services, from other funding partners – effectively bridging the health and human service sector.
HUBs convene Community Advisory Councils to facilitate this vital population health effort across its funder and delivery system partners.
Funding Sources and Flow
- HUBs support contracting and administration functions for CBOs. They streamline engagement with regional payers and other funders (state, local, federal, foundations, others) and manage data collection and quality management for the network.
- The Pathways Community HUB Model utilizes a risk-based “pay for performance” funding model – Care Coordinating Agencies (CCAs) are paid based on positive outcomes achieved (Pathways completed).
- Once established, HUB operating costs are partially supported by MCO payments, plus blended and braided funding from regional, state, federal, foundation and other potential sources.
- Medicaid Managed Care and other funders provide payments for outcomes achieved (Pathways) with high-risk members.
- Grant funding is sought to address social determinants, fund HUB operations, and provide payment outcomes to at-risk clients for whom contract funds are not available.
- In Ohio, HUB funds are legislated within the annual state budget.
- In New York State, the model aligns with planned State MRT investments to create regional Social Determinants of Health Networks to serve as single point of contracting for SDOH services; establish a regional referral network with multiple community based organizations and health systems; and utilize a shared IT platform to coordinate a regional referral network; as well as assess Medicaid members for key state-selected SDH social risk factors.
- $1.2 million budgeted for fiscal year ’21 and $4.95 million in fiscal year ’22.
Outcomes
The peer reviewed Journal of Maternal and Child Health published research indicating that the model achieved a cost savings of $5.59 for every $1 spent on high-risk maternal patients. Centene’s Buckeye Health Plan published research indicating a 236% return on investment from one HUB in Ohio, due to reduced neonatal intensive care admissions and shortened lengths of stay.
In Michigan, a Center for Medicare and Medicaid Innovation (CMMI) award in 2012 established the model in 19 counties served by three HUBs. For 7,435 clients enrolled in one HUB, complete medical referrals were achieved for 2,545 individuals, and 97 behavioral health connections to care were successfully achieved. Confirmed medical home connections were accomplished for 568. Housing was achieved for 224, employment was found for 122, health insurance was secured for 269, and over 8,003 successful connections were made to address SDOH needs.
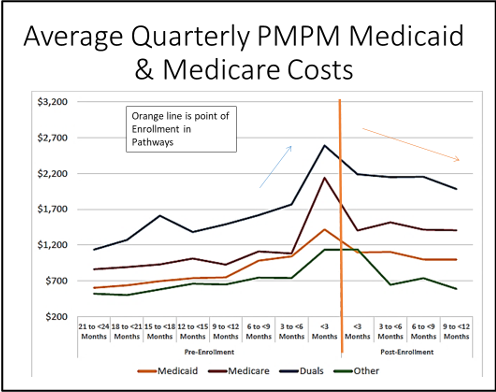
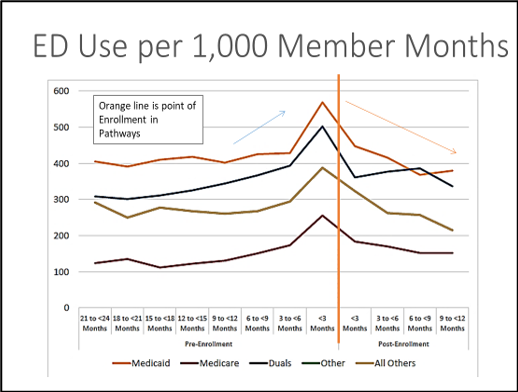
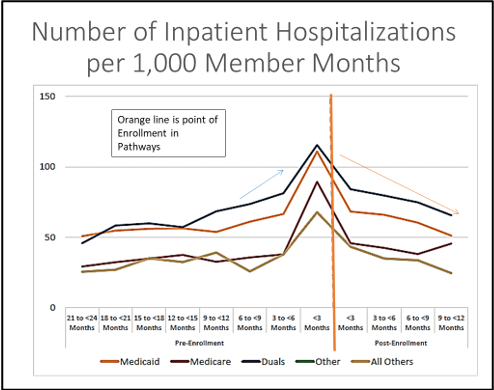
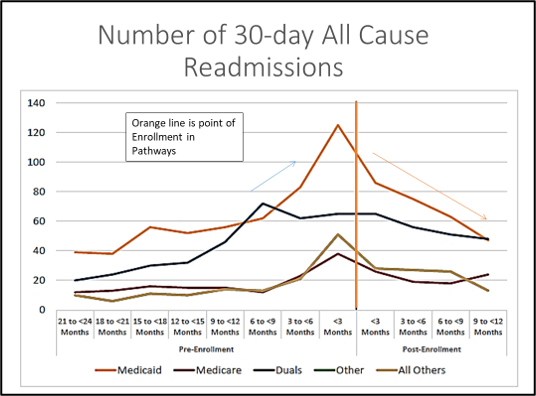
The model was found to reduce average quarterly PMPM Medicaid & Medicare Costs, inpatient hospitalizations, ED use and 30-day all cause readmissions. The orange line in the graphs below represents the point of enrollment in Pathways.