Communities across the country are seeing elevated numbers of adolescents in the Emergency Department due to suicide attempts, self-harm, anxiety, depression, substance use disorder (SUD), and overdose. While this youth mental health crisis predates COVID, it has been greatly exacerbated by the pandemic. According to the Centers for Disease Control and Prevention (CDC), in 2019, 13% of adolescents reported having a major depressive episode, a 60% increase from 2007, and suicide rates rose nearly 60% for youth ages 10 to 24 by 2018[1]. Then it got worse. Last December, the U.S. surgeon general issued a public health advisory about the adolescent mental health crisis as emergency room visits due to suicide attempts rose 51% for adolescent girls in early 2021, compared to the same period in 2019. For boys, the increase was 4%[2].
The surgeon general recommends a “whole-of-society effort,” including a focus on mental health education and prevention, early identification, and access to high-quality mental healthcare.[3] School-based intervention is ideal because only 20% of students in need of more intensive services typically receive needed care when referred to external providers.[4]
The Bipartisan Safer Communities Act has committed $1.7 billion for mental health support in schools and communities via an array of methods including grant programs. The following programs are currently available for a wide array of eligible entities, including states, cities/counties, Local Education Agencies (LEAs), Indian tribes or tribal organizations, health facilities, and nonprofit entities:
- Project AWARE (Advancing Wellness and Resiliency in Education). This grant program provides up to $1.8 million per year for up to 4 years to develop a sustainable infrastructure for school-based mental health programs and services. Grant recipients are expected to build collaborative partnerships with the State Education Agency (SEA), LEA), Tribal Education Agency (TEA), the State Mental Health Agency (SMHA), community-based providers of behavioral health care services, school personnel, community organizations, families, and school-aged youth. Grant recipients will leverage their partnerships to implement mental health-related promotion, awareness, prevention, intervention, and resilience activities to ensure that students have access to and are connected to appropriate and effective behavioral health services. Applications are due October 13th.
- Resiliency in Communities After Stress and Trauma (ReCAST). This program provides up to $1,000,000 a year for up to 4 years to promote resilience, trauma-informed approaches, and equity in communities that have recently faced civil unrest, community violence, and/or collective trauma within the past 24 months; and to assist high-risk youth and families through the implementation of evidence-based violence prevention, and community youth engagement programs. SAMHSA expects ReCAST to be guided by a community-based coalition of residents, non-profit organizations, and other entities (e.g., health and human service providers, schools, institutions of higher education, faith-based organizations, businesses, state and local government, law enforcement, and employment, housing, and transportation services agencies). Applications are due October 17th.
In addition to these two grants, there will be an expansion of the Certified Community Behavioral Health Center (CCBHC) Demonstration for States that is expected to be released later this month. The Excellence in Mental Health Act[5] established a federal definition and criteria for CCBHCs. These centers are a provider type that delivers a comprehensive range of mental health and SUD services to vulnerable individuals. They meet people where they are, which can include school-based services, and act as a critical partner in ensuring people have access to quality, affordable, and accessible mental health care.
School-based Mental Health Services
School-based mental health services, delivered within a Multi-Tiered System of Supports (MTSS) framework, can be supported by the aforementioned funding opportunities. The MTSS framework is currently used in public schools to target services and supports to students. As shown below, MTSS addresses universal prevention and progressively targeted support for students and families. It also aligns well with partnerships with community providers to establish an authentic community response that addresses the continuum of mental health needs.
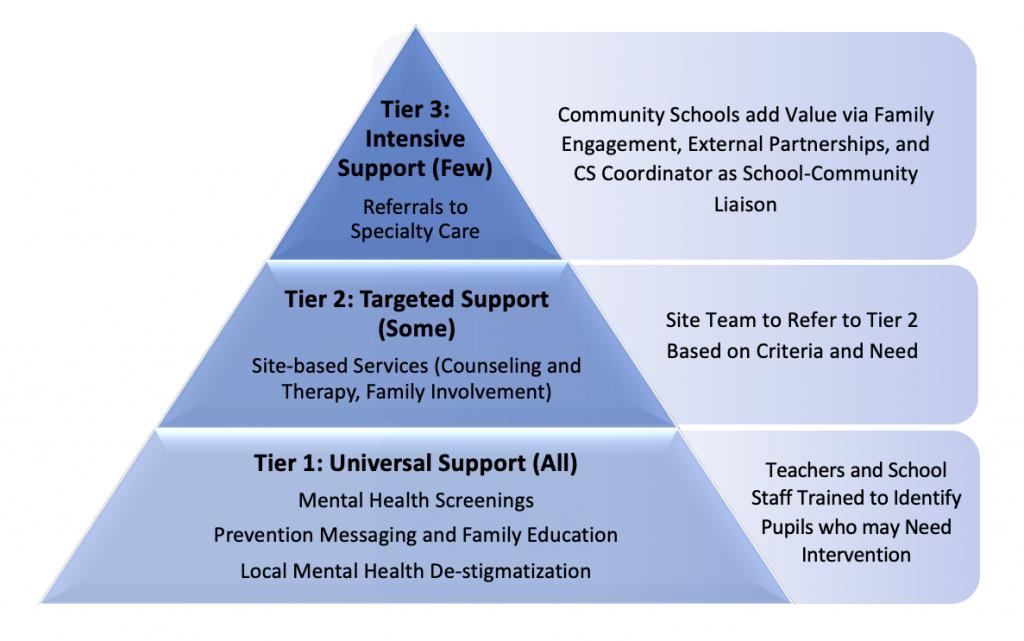
The key to a successfully implemented MTSS framework is a strong partnership between the school staff, parents/guardians, children, and community partners. This partnership works well when anchored to an evidence-based socio-emotional curriculum that is reinforced across all Tiers and familiar to all parties.
Suicide and Self Harm Prevention
Dialectical Behavioral Therapy (DBT) was recently identified by the New York Times as “the Best Tool We Have’ for Self-Harming and Suicidal Teens,” because it is one of the only interventions found to reduce self-harm and suicidal ideation, its effects are maintained at one-year follow-up[6], and it successfully engages young people[7].
Curriculum developers Drs. Lizz Dexter-Mazza and James Mazza worked with Marsha Linehan, the DBT treatment developer, to adapt DBT Skills into a universal school-based social emotional learning curriculum, called DBT-STEPS-A. This approach is designed to help schools intervene and support well-being and resiliency before kids are suicidal or self-harming. It trains existing school personnel to integrate skill-building into the school program, universally or as a stand-alone option for youth in 6-12th grade (an elementary version is in development). As such, it is a viable approach, despite the current shortage of mental health care professionals in school-based settings.
In addition, DBT provides a shared language and strategies across all three MTSS tiers so that everyone (students, school staff, teachers, providers, and parents/guardians) can benefit. Because DBT is also commonly provided in inpatient, outpatient, and residential behavioral health programs, the value of extending this approach into school settings is further magnified for youth who transition from the highest levels of care.
A DBT STEPS-A program taught at the universal level provides the broadest application within school-based settings, supports uptake that leads to peer-to-peer coaching and support, along with shifting the school environment and culture to promote mental wellbeing and reinforce the skills via a shared language and common strategies. In Tier 2, students are supported to practice skills and decision-making strategies in smaller group or individual psychotherapy sessions as needed. The third tier is more intensive support for students experiencing ongoing emotional and behavioral difficulties for whom Tier 2–level support is not sufficient. It is designed to supplement individual psychotherapy for those in need of a higher level of care. Parent/guardian skills-training seminars are recommended, so they can learn about the skills their child is acquiring and how best to support them while they are practicing. Engaging parents/guardians proactively helps to increase adaption of the skills across both home and school contexts.
A matched sample of adolescents who received the DBT STEPS-A curriculum demonstrated lower scores on the BASC-2 Emotion Symptom Index and on the BASC-2 Internalizing Problems, indicating fewer mental health difficulties, compared to peers who did not receive the curriculum (Cohen’s F squared equal to 0.65 and 0.83, respectively[8].
The DBT curriculum is accessible via a $50 manual. All handouts for kids are available in English and Spanish and can be printed from a web-based link for free. An array of trainings are available to support rapid school-based service delivery.
To learn more about current and upcoming funding for enhanced school and community-based mental health care or DBT-STEPS-A, contact:
Heidi Arthur, Principal [email protected]
Michael Butler, Principal [email protected]
You can also contact DBT in Schools, LLC for information about DBT-STEPS-A [email protected].
[1] National Vital Statistics reports – Centers for Disease Control and … (n.d.). Retrieved from https://www.cdc.gov/nchs/data/nvsr/nvsr69/nvsr-69-11-508.pdf
[2] Richtel, M. (2021, December 7). Surgeon general warns of Youth Mental Health Crisis. The New York Times. Retrieved from https://www.nytimes.com/2021/12/07/science/pandemic-adolescents-depression-anxiety.html
[3] Protecting youth mental health – hhs.gov. (n.d.). Retrieved from https://www.hhs.gov/sites/default/files/surgeon-general-youth-mental-health-advisory.pdf
[4] Sheryl H. Kataoka, M.D., M.S.H.S., Lily Zhang, M.S., and Kenneth B. Wells, M.D., M.P.H. (2002). Unmet Need for Mental Health Care Among U.S. Children: Variation by Ethnicity and Insurance Status. The American Journal of Psychiatry: https://doi.org/10.1176/appi.ajp.159.9.1548
[5] Excellence in Mental Health Act. (2013, February 7). http://www.congress.gov/
[6] McCauley E, Berk MS, Asarnow JR, et al. Efficacy of Dialectical Behavior Therapy for Adolescents at High Risk for Suicide: A Randomized Clinical Trial. JAMA Psychiatry. 2018;75(8):777–785. doi:10.1001/jamapsychiatry.2018.1109 https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2685324#:~:text=Given%20its%20effectiveness%20with%20adults,suicidal%20youths%20with%20promising%20results.&text=A%20recent%20RCT%20with%20self,1%2Dyear%20follow%2Dup.
[7] Rathus, Jill H. ( 2014). DBT skills manual for adolescents. New York :The Guilford Press,
[8] Elizabeth T. Dexter-Mazza, James J. Mazza, Alec L. Miller, Kelly Graling, Elizabeth Courtney-Seidler, and Dawn Cattuchi (2022). Application of DBT in a School-Based Setting. Pending publication

