This week our In Focus reviews the Rhode Island Medicaid managed care request for qualifications (RFQ), released on November 12, 2021, by the Executive Office of Health and Human Services (EOHHS). Contracts are worth approximately $1.4 billion annually and cover over 300,000 individuals.
Background
Medicaid managed care organizations (MCOs) will provide acute, primary care, specialty care, pharmacy, and behavioral health services to RIteCare, Rhody Health Partners, and the adult Medicaid expansion population.
Enrollment in managed care is mandatory for all populations across the three programs. EOHHS also has the right to amend the contract to include new populations, services, or programs, including the RIte Smiles (dental) and Rhode Island Medicare-Medicaid Plan (MMP) programs.
RFQ Goals
MCOs will be expected to work closely with accountable entities (AEs) as a part of the Rhode Island Health System Transformation Project (HSTP) component of the Section 1115 Demonstration waiver. The HSTP provides the financial and structural support for growth and development of AEs. Current AEs include health centers, hospitals, and primary care providers. All members that are attributed to an AE are also enrolled in an MCO. AEs serve approximately 68 percent of managed care enrollees. EOHHS proposes a system of care where the MCO and AE partner together to provide care programs to support members that are:
- Person-centered and holistic
- Collaborative
- Community-based
- Equitable
- Population health-focused
- For better outcomes, lower cost
Through this procurement, EOHHS also seeks to align coverage for members who transition from Medicaid to Exchange coverage and from Exchange coverage to Medicaid. This would be done through similar sets of providers to ensure continuity, having a single point of contact, and greater assistance from carriers in maintaining coverage throughout eligibility changes.
As a result of feedback from the request for information (RFI) released in March, EOHHS found the following fundamental principles and policy goals:

The Department of Administration (DOA), on behalf of EOHHS, received responses from 19 potential bidders, organizations, associations, and community leaders.
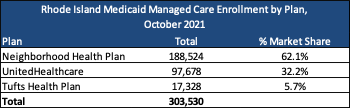
Current Market
As of October 2021, there were 303,530 members across the Medicaid managed care program. RIteCare served 176,115 individuals, Rhody Health Partners 27,828, and expansion 99,933. There are also an additional 346 members in Rhody Health Partners covered under PACE. Current incumbents are Neighborhood Health Plan (NHP), Tufts Health Plan, and UnitedHealthcare. NHP accounts for nearly two-thirds (62.1 percent) of all enrollees in the market.
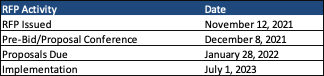
Timeline
Proposals are due January 28, 2022. Any MCO that plan to submit a proposal must attend the mandatory pre-bid/proposal conference on December 8, 2021. Contracts will run from July 1, 2023, until June 30, 2028, with up to three additional option years.
Evaluation
MCOs must pass all the mandatory requirements and receive a minimum of 750 points out of a possible 1,000 points, or 75 percent, on the technical proposal. The components of the technical proposal include the following: