This week's roundup:
- In Focus: Executive Order Addressing Homelessness: The Federal Shift Toward Institutionalization
- California Individual Marketplace Plans Propose Rate Hike of 10.3 Percent in 2026
- Florida Medicaid Spending Could Exceed Fiscal 2026 Budget by $511 Million
- Iowa to Implement Medicaid Work Requirements in January 2026
- Louisiana Establishes Medicaid Doula Coverage Effective August 1
- North Carolina Delays Medicaid Standard Plan Reprocurement by Two Years Amid $319 Million Budget Shortfall
- Vermont Releases Medicaid NEMT RFP
- CMS Launches Additional Verification Process to Confirm Citizenship, Immigration Status for Medicaid
- Elevance, NACHC to Integrate Food as Medicine Program in Community Health Centers
- CareSource Invests in Radley Health to Provide Workforce Peer Support Services for Patients with SMI
In Focus
Executive Order Addressing Homelessness: The Federal Shift Toward Institutionalization
President Trump signed an executive order (EO), Ending Crime and Disorder on America’s Streets, on July 24, 2025, signaling a significant shift in federal homelessness policy and the requirements for organizations that use federal dollars to address homelessness in their communities. The order emphasizes public safety and prioritizes institutionalization and mandatory treatment over housing first approaches.
The administration asserts that “the overwhelming majority of these individuals are addicted to drugs, have a mental health condition, or both” and calls for transitioning homeless individuals into long-term institutional settings through civil commitment for “humane treatment.” Below, Health Management Associates (HMA) outlines key elements of the EO, including provisions, key stakeholder considerations, and potential strategies to maintain care continuity amid federal changes.
Key Elements of the Executive Order
End of Housing First: The EO discontinues support for the Housing First model, directing federal agencies to prioritize mandatory treatment. The Department of Housing and Urban Development (HUD) Secretary is directed to take steps requiring treatment participation as a condition of HUD program participation.
Support for Civil Commitment Infrastructure: The federal government will assist state and local governments with technical guidance, grants, and other resources to implement civil commitment, institutional treatment, and step-down treatment standards. The Attorney General and US Department of Health and Human Services (HHS) Secretary are instructed to pursue reversal of legal precedents that restrict civil commitments for individuals with mental illness who pose risks or are unable to care for themselves.
Restructuring Federal Programs: The EO directs HHS, HUD, and the Departments of Justice (DOJ) and Transportation (DOT) to review discretionary grants and restructure programs to ensure compliance with the new guidelines, as outlined below.
- HHS Substance Abuse and Mental Health Services Administration (SAMHSA) grants will no longer support harm reduction or safe consumption efforts and has issued a “Dear Colleague” letter clarifying which services will be funded; for example, naloxone distribution can be funded, but clean syringe distribution cannot.
- HUD will exclusively, where permissible, fund programs for women and children and revise regulations to exclude registered sex offenders.
- Some emergency law enforcement funds may be allocated for encampment removals.
Expanded Roles: The EO directs HHS to leverage the use of federally qualified health centers (FQHCs) and Certified Community Behavioral Health Clinics (CCBHCs) to reduce homelessness and ensure federal funds support crisis intervention and comprehensive behavioral health services. In addition, the Attorney General is directed to prioritize funding for the expansion of drug and mental health courts.
Notably, federal grants will prioritize jurisdictions and states that enforce laws against open drug use, urban camping, urban loitering, and urban squatting. Grant recipients must also share certain health-related data with law enforcement, as permitted by law.
Considerations for Stakeholders
States, local governments, and county jurisdictions must assess housing and homeless programs that use federal funding streams. They must consider the implications of their current program activities and, where possible, realign programs with new requirements. They may gain access to new funding for treatment beds, drug and mental health courts, crisis response, and law enforcement support but risk losing funding for those programs that use harm reduction or housing first models. Local governments could face increased jail overcrowding and legal challenges related to civil commitments and data sharing. Early examination of current programs, particularly HUD and crisis programs, as well as early planning, will be essential.
Providers may need to restructure services to comply with the new mandates, including collaboration with crisis/removal entities and law enforcement and expanded reporting. Emergency department and inpatient facilities may see increased demand, especially from uninsured individuals.
State behavioral health authorities and other stakeholders can benefit from forming advisory councils to develop ethical frameworks for civil commitments, as well as consider providing training for providers and law enforcement and propose revisions to state statutes and regulations
Homeless individuals are likely to experience increased policing, institutionalization, and loss of access to non-mandated services and housing.
What Happens Next
Federal agencies are now responsible for implementing the EO, revising grant programs, issuing guidance, and shifting funding priorities toward enforcement and institutional treatment. These changes will redefine compliance for local governments and service providers.
Health and housing organizations must quickly assess the implications of this policy shift. Strategic collaboration across sectors, including behavioral health, housing, law enforcement and judicial systems, will be essential to maintain care continuity and protect individual rights.
Connect with Us
HMA’s housing and homelessness and behavioral health experts are closely monitoring the evolving federal policy landscape and legal developments. We are tracking federal funding shifts, priorities, and opportunities across HHS, HUD, DOJ, and DOT, helping stakeholders align their programs with new priorities to enhance eligibility and impact.
For details about federal agency implementation of the EO and downstream effects, contact our featured experts: Tia Cintron, MHA, Managing Director, Housing and Health Solutions Practice Group, and Monica Johnson, MA, LPC, Managing Director, Behavioral Health Practice Group.
HMA Roundup
California
California Individual Marketplace Plans Propose Rate Hike of 10.3 Percent in 2026. Covered California, the state’s Affordable Care Act Marketplace, announced on August 14, 2025, that preliminary individual rates will rise by an average 10.3 percent. The proposed increase is largely attributed to the end of the federal enhanced premium tax credits and increase health care and pharmacy costs after December 31, 2025.
Florida
Florida Medicaid Spending Could Exceed Fiscal 2026 Budget by $511 Million. Florida Phoenix reported on August 15, 2025, that Florida could exceed its fiscal 2025-26 Medicaid appropriations by approximately $510.7 million, according to projections by economists at the Social Services Estimating Conference. Medicaid managed care plans are projected to receive $7.8 billion by the end of the fiscal year, $285.4 million more than projected. The projections for fiscal year 2026-27 show that Florida could exceed its base Medicaid budget by $2.1 billion, with payments to managed care plans accounting for $1.75 billion of the estimated shortfall. The projections show lower than anticipated enrollment numbers for the current fiscal year, with 67,000 fewer people receiving benefits than originally thought when legislators were developing the budget.
Iowa
Iowa to Implement Medicaid Work Requirements in January 2026. Radio Iowa reported on August 19, 2025, that Iowa will implement Medicaid work requirements starting January 1, 2026, ahead of the federal 2027 mandate. Able-bodied adults under 65 in the Iowa Health and Wellness Plan will need to prove they work at least 80 hours per month to keep coverage, though exemptions will apply for people with disabilities, serious health conditions, or parents of young children. State officials estimate around 100,000 Iowans could be affected.
Louisiana
Louisiana Establishes Medicaid Doula Coverage Effective August 1. WBRZ reported on August 17, 2025, that Louisiana Medicaid began covering doula services for eligible individuals on August 1, following Governor Jeff Landry’s signature of House Bill 454. The coverage, which aims to reduce the state’s maternal mortality rate, includes five prenatal visits, three postpartum visits, and support during labor and delivery.
North Carolina
North Carolina Delays Medicaid Standard Plan Reprocurement by Two Years Amid $319 Million Budget Shortfall. The North Carolina Department of Health and Human Services released on August 11, 2025, a letter stating that it will delay the re-procurement of its Medicaid Standard Plan and Tailored Plan contracts by two years due to insufficient administrative funding and uncertainty stemming from federal and state budget cuts. The delay comes alongside a $319 million Medicaid rebase shortfall for State Fiscal Year 2025–26 which will trigger broad rate reductions of 3 percent across all providers and 8–10 percent for certain institutional and behavioral health services starting October 1. It will also end optional GLP-1 coverage for weight loss and terminate the Healthy Opportunities Pilot and the Integrated Care for Kids Pilot.
Vermont
Vermont Releases Medicaid NEMT RFP. The Department of Vermont Health Access (DVHA), Agency of Human Services released on August 14, 2025, a request for proposals (RFP) for Medicaid Non-Emergency Medical Transportation (NEMT). DVHA currently oversees and monitors the NEMT benefit, contracting with the Vermont Public Transportation Association (VPTA) as the NEMT provider, who further subcontracts with a network of public transportation providers. Vermont is seeking to reprocure this contract with one or more NEMT brokers. Proposals are due October 1, 2025. Implementation is expected to be as soon as January 1, 2026. and no later than July 1, 2026. Contracts will run for three years, with up to two optional years.
National
CMS Launches Additional Verification Process to Confirm Citizenship, Immigration Status for Medicaid. The Centers for Medicare & Medicaid Services (CMS) announced on August 19, 2025, that it is launching a new verification process to check that Medicaid and Children’s Health Insurance Program (CHIP) enrollees meet the necessary citizenship or immigration requirements to receive benefits. CMS will start providing states with monthly enrollment reports that identify individuals whose status could not be confirmed through federal databases, and states will be responsible for reviewing the cases and verifying documentation status of identified enrollees. When necessary, states will have to request additional documentation and take action when identified individuals do not meet requirements. CMS will monitor progress monthly.
Industry News
Elevance, NACHC to Integrate Food as Medicine Program in Community Health Centers. Fierce Healthcare reported on August 18, 2025, that Elevance Health will be partnering with the National Association of Community Health Centers (NACHC) to integrate the plan’s food as medicine program into community health centers. The partnership will give eligible Medicaid members access to nutritional services, including tailored interventions, coaching, and referrals. It aims to improve patient engagement, reduce chronic disease, and strengthen preventative healthcare. Additionally, NACHC will receive a six-month grant from Elevance to develop a scalable food as medicine model.
CareSource Invests in Radley Health to Provide Workforce Peer Support Services for Patients with SMI. CareSource announced on August 14, 2025, that it has invested in Ohio-based Radley Health (RadleyCare). RadleyCare provides peer workforce development services to individuals with serious mental illness (SMI). CareSource will partner with RadleyCare to identify gaps and enhance peer support services to improve community-based behavioral health care in Ohio.
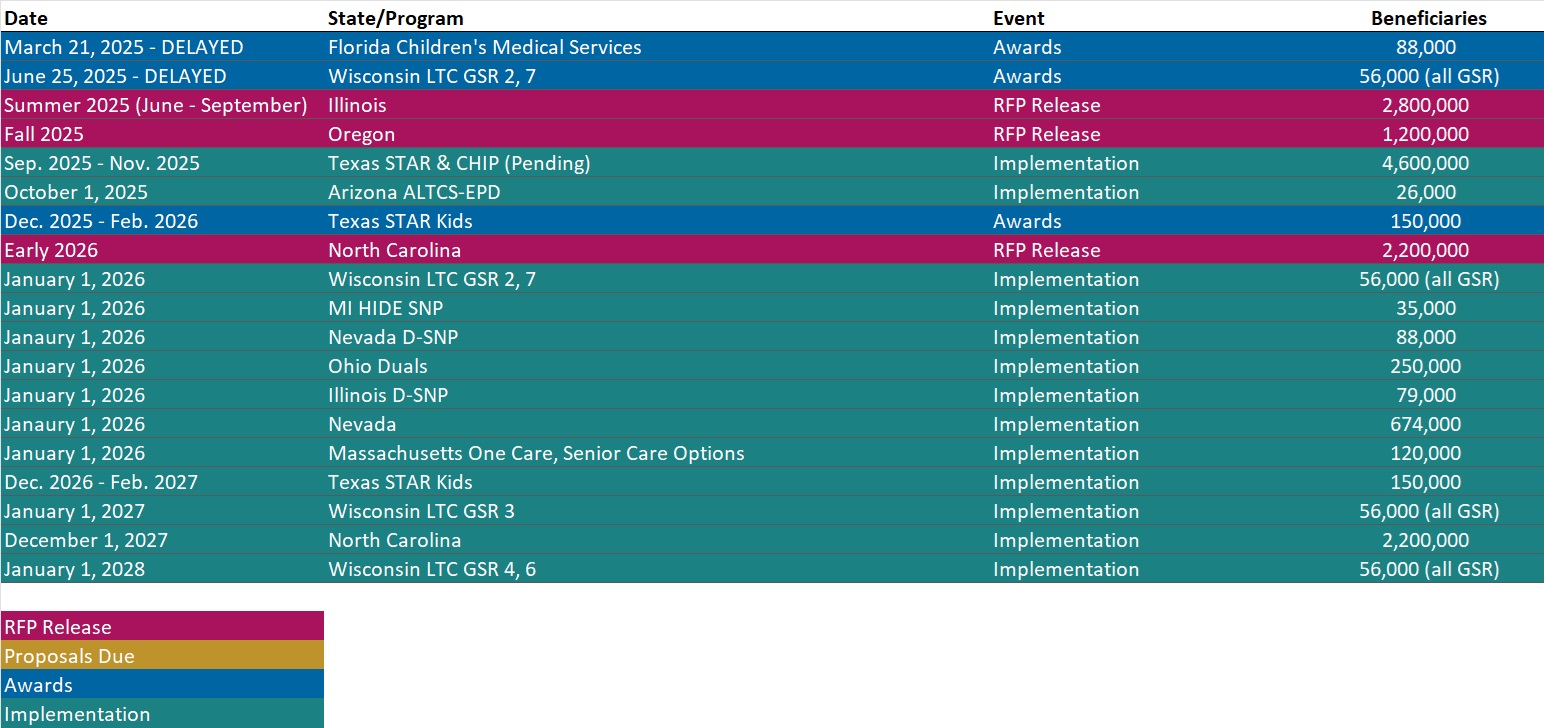
RFP Calendar
Actuaries Corner
Physicians Are Working More but Reimbursement Isn’t Keeping Pace. Physicians are working harder now than in past years, but they’re getting less for that work, according to new research from Kaufman Hall. Editor’s Note: According to a report from Kaufman Hall, the amount of work that goes into providing a physician service has increased by 11 percent over the past two years. This is an issue as Kaufman Hall also found that patient revenue per each work relative value unit dropped 7 percent over the same time period, leading provider compensation per work relative value unit fell 2 percent. A recent CMS rule includes a Medicare base rate hike of 2.5 percent for doctors next year. But, its impact on reimbursement will vary wildly based on a physician’s specialty and site of practice.
Discover other developments in the Wakely Wire here.
HMA News & Events
HMA Conference
Coffee Conversations and Collaborations. New session content and speakers added to the HMA National Conference.
Wakely Webinar
From Insight to Impact: Measuring What Matters in Care Management. Tuesday, August 26, 2025, 2 PM ET. With care management programs and point solutions continuing to expand across Medicare, Medicaid, and Commercial lines of business, the need for rigorous, data-driven evaluation has never been more urgent. Join us for a practical session on how payers and partners can design and execute credible studies to measure both the financial and member experience impact of their investments. We’ll cover where to start (hint: it begins with your data), introduce analytical frameworks for assessing direct and indirect outcomes, and share lessons from a recent case study—blinded for objectivity. Whether you’re considering how to pursue new opportunities, understanding the landscape, building your first evaluation or refining an existing one, this session offers strategic and tactical guidance for turning good intentions into actionable insights.
NEW THIS WEEK ON HMA INFORMATION SERVICES
(Exclusive Access for HMAIS Subscribers):
HMAIS Medicaid Market Overviews, Reports, and Data
- Updated State Medicaid Agency Contracts (SMACs) Inventory
- Updated HMA Federal Health Policy Snapshot
- New Medicaid enrollment, RFP documents, and other market intelligence resources for dozens of states
- Updated New Mexico Overview
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services.
If you’re interested in becoming an HMAIS subscriber, contact Andrea Maresca at [email protected].