HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: An HMA Toolkit and Webinar to Advance Health Equity & Access for Rural Dually Eligible Individuals

- Arkansas Releases RFI for Medicaid Managed Care Module of MMIS Replacement

- Florida Governor Announces Proposal to Regulate PBMs

- Medicaid Expansion News: Georgia, Kansas, Mississippi, North Carolina, South Dakota

- Georgia Releases RFI to Audit PBMs Contracted Through Medicaid Plans

- Louisiana Releases RFP for Permanent Supportive Housing Services Funded in Part by Medicaid

- Michigan Doulas Push for Higher Medicaid Reimbursement Rates

- Mississippi Seeks Bids for Medicaid FFS Non-emergency Transportation Services

- South Carolina to Continue Several Flexibilities After COVID-19 PHE Ends

- CMS Announces Medicare Accountable Care Partnerships Will Cover 13.2 Million Enrollees in 2023

- Health Network One Acquires Premier Eye Care

In Focus
An HMA Toolkit and Webinar to Advance Health Equity & Access for Rural Dually Eligible Individuals
In 2022, HMA convened stakeholder roundtables in three states – including New Mexico, North Dakota, and Tennessee to identify the challenges facing dually eligible individuals living in rural areas and to propose solutions to these challenges. Informed by this process, HMA developed the Health Equity & Access for Rural Dually Eligible Individuals (HEARD) Toolkit.
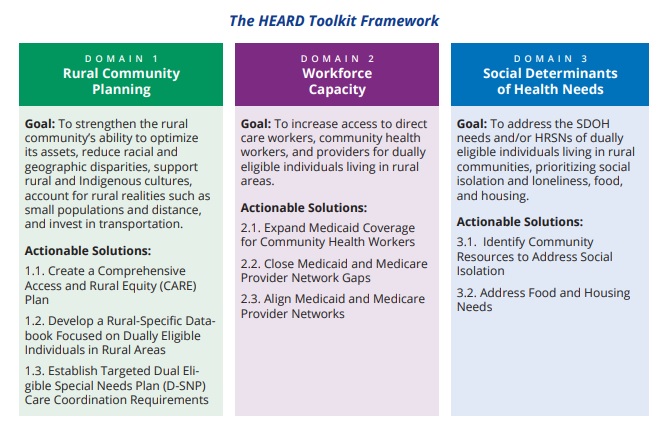
The toolkit is structured around three domains used to organize eight solutions. For each solution, HMA provides a description of the rural access challenge, the proposed solution, and the proposed tool. Each tool is powered by some type of lever available to the federal and state government. We anticipate that policymakers will build upon this toolkit through continued dialogue with rural communities. The toolkit’s framework, goals, and actionable solutions are summarized in the figure below.
HMA Principal Ellen Breslin, Consultant Samantha Di Paola, and Senior Consultant Susan McGeehan authored the toolkit, with research contributions from HMA Principals Rebecca Kellenberg and Andrea Maresca.
The toolkit is available here.
On February 2, 2023, 1pm ET, HMA will host a webinar on the HEARD toolkit. During this webinar, HMA experts and panelists including Craig Caplan (HRSA), Dennis Heaphy (DPC), Pam Parker (SNP Alliance), and Tallie Tolen (New Mexico Medicaid) will summarize and discuss the toolkit’s actionable solutions for improving rural dually eligible individuals’ health and social outcomes.
Click here to register.
HMA Roundup
Arkansas
Arkansas Releases RFI for Medicaid Managed Care Module of MMIS Replacement. The Arkansas Department of Human Services released on January 17, 2023, a request for information (RFI) for a potential Medicaid managed care module of the state’s planned replacement of its Medicaid management information system (MMIS). The solution must automate assignment and management of Medicaid beneficiaries across multiple managed care organizations, support the centralized management and oversight of the state’s financial management requirements, and provide integration with existing MMIS modules and systems. Responses are due on February 17. Read More
California
California Launches Stimulant Use Disorder Treatment Pilot Program. Managed Healthcare Executive reported on January 17, 2023, that California Medicaid launched a pilot program with Pear Therapeutics to treat stimulant use disorder through a contingency management program. The program will be initially launched in 24 counties in early 2023. Read More
Delaware
Delaware Requests 5-year Extension of Diamond State Health Plan Section 1115 Waiver. The Centers for Medicare & Medicaid Services announced on January 13, 2023, that Delaware requested a five-year extension of its Delaware Diamond State Health Plan Section 1115 waiver, in which Medicaid members are covered by managed care plans. The waiver also covers long-term services and supports, enhanced behavioral health services, adult dental services, and coverage for former foster care youth under age 26. The current waiver expires on December 31, 2023. The federal public comment period will be open until February 12. Read More
Florida
Florida Governor Announces Proposal to Regulate PBMs. Health News Florida reported on January 12, 2023, that Florida Governor Ron DeSantis outlined a proposal to regulate pharmacy benefit managers (PBMs). The plan would bar PBMs from requiring consumers to use mail programs for prescriptions and increase the information PBMs must provide the state regarding company affiliations. DeSantis also hopes to end surprise billing and prescription drug overpayments. Read More
Georgia
Georgia Democratic Lawmakers to Prioritize Medicaid Expansion During Legislative Session. WABE reported on January 13, 2023, that Democratic lawmakers in Georgia will prioritize Medicaid expansion during the current legislative session. Georgia Governor Brian Kemp did not include full expansion in his proposed fiscal 2024 budget, but he did include $52 million to fund the implementation of Georgia Pathways to Coverage, a limited Medicaid expansion program that includes work requirements. Read More
Georgia Releases RFI to Audit PBMs Contracted Through Medicaid Plans. The Georgia Department of Community Health released on January 12, 2023, a request for information (RFI) to audit pharmacy benefit managers (PBM) contracted through Medicaid managed care plans, which are referred to in the state as care management organizations (CMOs). The audit would cover outpatient prescription claims from July 1, 2020, through July 31, 2022. Responses are due on January 27. Read More
Georgia House Speaker Creates Committee to Coordinate Health Care Legislation. The Atlanta Journal-Constitution reported on January 11, 2023, that Georgia House Speaker Jon Burns (R-Newington) plans to create a special committee to oversee legislation worked on by multiple health-related House committees. The committee will focus on issues like health care access, insurance, surprise billing, and hospital certificates of need. Burns did not rule out Medicaid expansion when asked. Read More
Kansas
Kansas Governor Proposes Medicaid Expansion in Fiscal 2024 Budget. The Kansas Reflector reported on January 12, 2023, that Kansas Governor Laura Kelly is proposing Medicaid expansion in her fiscal 2024 budget. State House and Senate leaders both oppose expansion. Read More
Iowa
Iowa Faces Class Action Lawsuit Claiming it Failed to Provide Medicaid-Eligible Children With Mental Health Care. Ropes & Gray announced on January 17, 2023, the filing of a class action lawsuit claiming that Iowa is denying Medicaid-eligible children their right to mental health care, including intensive care coordination, in-home therapeutics services, and crisis response services. The suit was filed along with with co-counsel Disability Rights Iowa, Children’s Rights and National Health Law Program. Read More
Illinois
Illinois, Medicaid Plan Face Federal Investigation Over Medical Care for Foster Children. The Chicago Sun Times reported on January 13, 2023, that the Centers for Medicare & Medicaid Services is opening an investigation into claims that Medicaid health plan Centene failed to provide basic medical care to Illinois foster children under its contract with the state YouthCare program. Read More
Louisiana
Louisiana Releases RFP for Permanent Supportive Housing Services Funded in Part by Medicaid. The Louisiana Department of Health released on January 17, 2023, a request for proposals (RFP) for contractors to provide Permanent Supporting Housing (PSH) services in nine regions of the state. Many of the PSH households will be funded through the Medicaid program. The state intends to award seven to 10 three-year contracts, with a two-year extension option. Proposals are due by February 24, 2023. Read More
Maine
Maine Lawmakers Introduce Bill to Extend Medicaid Coverage to Adult Non-citizens. The Maine Wire reported on January 16, 2023, that Maine House Speaker Rachel Talbot Ross (D-Portland) and other lawmakers introduced a bill (LD 199) that would appropriate state funds to extend MaineCare Medicaid coverage to asylum seekers, refugees, and individuals who are in the country illegally. If passed, Maine would be the first state to offer Medicaid coverage to adult residents who are illegally in the country. Read More
Michigan
Michigan Doulas Push for Higher Medicaid Reimbursement Rates. The Detroit Free Press reported on January 16, 2023, that doulas in Michigan are pushing for higher Medicaid reimbursement rates since the state implemented a policy on January 1 that allows Medicaid to cover doula services. The current overall rate is $1,150, which includes a $700 base rate and up to six pre- or post-natal visits at $75 each. Read More
Mississippi
Mississippi Lawmakers to Consider Bills on Medicaid Expansion, Postpartum Coverage. The Associated Press reported on January 16, 2023, that Mississippi lawmakers will consider bills on whether to implement Medicaid expansion and extend postpartum Medicaid coverage from 60 days to 12 months. Lawmakers are also considering bills to help hospitals that are struggling financially by creating grant programs or tax credits. Read More
Mississippi Seeks Bids for Medicaid FFS Non-emergency Transportation Services. The Mississippi Division of Medicaid released on January 13, 2023, an invitation for bids for non-emergency transportation brokerage services for fee-for-service (FFS) Medicaid beneficiaries. Medical Transportation Management (MTM) is the current vendor. Proposals are due on March 23 and awards are anticipated no later than April 10. The contract will be implemented on June 8 and the operational phase will begin on October 1. Read More
Montana
Montana Representative Introduces Bill to Increase Medicaid Reimbursement Rates for Psychiatric Treatment Facilities With Children. Choteau Acantha reported on January 17, 2023, that Montana representative Jane Gillette (R-Gallatin County) introduced a bill (HB 147) that would increase the Medicaid reimbursement rate to 133 percent of the rate in effect on July 1, 2022, for psychiatric residential treatment facilities and therapeutic group homes treating children, which would match the rate paid to out-of-state providers. As of November 2022, 61 children were at in-state facilities and 67 were out-of-state. The bill is aimed at having more children treated in-state. Read More
Montana Considers Rule to Require Prior Authorizations for Abortions Covered by Medicaid. The Associated Press reported on January 12, 2023, that the Montana Department of Public Health and Human Services is considering a rule that would require prior authorization for abortions covered by Medicaid. Montana is one of 16 states in which Medicaid is required to cover the costs of medically necessary abortions based on state law or court order.
North Carolina
North Carolina Senate Leader Includes Medicaid Expansion Among Priorities. The Carolina Journal reported on January 11, 2023, that North Carolina Senate president pro tempore Phil Berger (R-Rockingham) hopes to pass Medicaid expansion legislation during the current session. In 2022, the state House and Senate each passed separate versions of expansion legislation, but could not agree on a single bill. Read More
South Carolina
South Carolina to Continue Several Flexibilities After COVID-19 PHE Ends. The South Carolina Department of Health and Human Services announced on January 18, 2023, that it will continue and make permanent after the public health emergency (PHE) ends the following temporary flexibilities initiated by federal regulators during the COVID-19 pandemic: COVID-19 testing without copays and the application of caries arresting medicament. Flexibilities that will remain for a year after the PHE ends include COVID-19 vaccination with a copay, suspension of an annual limit of 12 ambulatory care visits, and waiver of copays for all evaluation and management codes. Temporary flexibilities that will end when the PHE ends include early pharmacy refill denials being bypassed for fee-for-service members and the extension of the timeframe for submitting prior authorization documents to seven days.
South Dakota
South Dakota Seeks Additional Employees to Implement Medicaid Expansion by July 2023. KELOLAND reported on January 17, 2022, that the South Dakota Department of Social Services is requesting 68 additional full-time employees to implement Medicaid expansion for nearly 58,000 individuals. The state intends to submit Medicaid State Plan amendments for federal approval in March 2023 and implement expansion in July 2023. Read More
South Dakota Releases Medicaid Expansion Third-Party Administrator RFI. The South Dakota Department of Social Services released on January 9, 2023, a request for information (RFI) regarding implementation of a third-party administrator (TPA) for the state’s Medicaid expansion population. The TPA would handle prior authorization, provider claims processing and payment, customer service and support, and data analytics and reporting. Responses are due by February 23, 2023. Read More
Utah
Utah Submits Waiver Amendment to Provide LTSS, Integrated Behavioral Health Services. The Centers for Medicare & Medicaid Services announced on January 12, 2023, that Utah submitted requests to amend its Medicaid Reform Section 1115 waiver to allow individuals to provide long-term services and supports (LTSS) to patients with complex behavioral conditions. Another amendment would allow individuals to receive existing covered physical and behavioral services in an integrated model through a contracted local mental health authority, which will be selected through a request for proposals. The federal comment period will be open until February 12. Read More
Utah House Representative Files Bill to Extend Postpartum Medicaid Coverage from 60 Days to 12 Months. State of Reform reported on January 12, 2023, that Utah House Representative Rosemary Lesser (D-Ogden) filed a bill to extend postpartum Medicaid coverage from 60 days to 12 months. Lesser also plans to introduce legislation to expand income eligibility for Medicaid to 200 percent of the federal poverty level. Read More
Wyoming
Wyoming House Committee Advances Bill to Extend Medicaid Postpartum Coverage. The Sheridan Press/Wyoming News Exchange reported on January 16, 2023, that the Wyoming House Labor, Health and Social Services Committee advanced a bill to extend Medicaid postpartum coverage to 12 months from 60 days. The bill will now be debated by the full state House. Read More
National
CMS to Audit Schizophrenia Diagnoses, Post All Nursing Home Citations on Care Compare. The Centers for Medicare & Medicaid Services (CMS) announced on January 18, 2023, that it will conduct off-site audits of assessment and coding of individuals with a schizophrenia diagnosis to reduce inappropriate use of antipsychotic medications in nursing homes. CMS will also begin displaying all nursing home citations, even those being disputed, on its Care Compare website for consumers. Read More
53 Percent of State Medicaid Eligibility Determinations Were Processed in Under 24 Hours from April to June 2022. The Centers for Medicare & Medicaid Services (CMS) reported on January 17, 2023, that 53 percent of state Medicaid Modified Adjusted Gross Income (MAGI) eligibility determinations were processed in under 24 hours from April to June 2022. Oklahoma had the highest percentage processed in under 24 hours at 100 percent, while Nevada, North Carolina, and South Dakota had the lowest at zero percent. Read More
CMS Announces Medicare Accountable Care Partnerships Will Cover 13.2 Million Enrollees in 2023. The Centers for Medicare & Medicaid Services (CMS) announced on January 17, 2023, that Medicare accountable care initiatives will cover more than 13.2 million Medicare beneficiaries through more than 700,000 providers and organizations in 2023. The programs include the Medicare Shared Savings Program; the Accountable Care Organization Realizing Equity, Access, and Community Health Model; and the Kidney Care Choices Model. CMS has a goal of providing 100 percent of traditional Medicare beneficiaries with accountable care relationships by 2030. Read More
Medicare Drug Price Provisions of Inflation Reduction Act Take Effect. The New York Times reported on January 14, 2023, that a $35 monthly price cap on insulin for Medicare Part D beneficiaries took effect on January 1, 2023, as a result of the Inflation Reduction Act. Additionally, adult vaccines covered by Part D, including the shingles vaccine, are free of charge, and drug manufacturers have to pay rebates for drugs whose price increases faster than the inflation rate. Medicare has not yet determined which price increases will require rebates or the amounts of the rebates. Read More
CMS Releases Fiscal 2021 Drug Utilization Review Annual Reports. The Centers for Medicare & Medicaid Services (CMS) released on January 13, 2023, the fiscal 2021 drug utilization review annual reports for Medicaid fee-for-service and managed care organization programs. The reports indicate a 12 percent increase in enrollment in Medicaid managed care programs with a drug benefit from fiscal 2020 and a two percent decrease in enrollment in Medicaid FFS programs. Read More
Uninsured Rate Falls Half a Percentage Point from 2019 to 2021, HHS Reports. Fierce Healthcare reported on January 13, 2023, that Medicaid expansion and increased Exchange plan accessibility drove the national uninsured rate from 11.1 percent in 2019 to 10.5 percent in 2021, according to the U.S. Department of Health and Human Services (HHS). The largest declines in the uninsured rate were among individuals with incomes between 100 and 250 percent of poverty. Read More
CMS Allows Medicaid, CHIP to Reimburse Behavioral Specialists for Consulting with Primary Care Providers. Health Payer Intelligence reported on January 11, 2023, the Centers for Medicare & Medicaid Services (CMS) issued guidance allowing Medicaid and the Children’s Health Insurance Program (CHIP) to reimburse specialty behavioral health providers when they are consulted by a primary care provider. The reimbursed consultations can occur even without the presence of the beneficiary. Read More
Healthcare Labor Costs, Service Integration Among Top Priorities for Healthcare Organizations. Modern Healthcare reported on January 12, 2022, that contract labor spending is expected to stay elevated for the near future, driven by wage inflation and staffing shortages, but is coming down from peak levels, according to speakers at the J.P. Morgan Healthcare Conference. Other highlights of the conference: integrating healthcare services remains a priority; Medicare Advantage plans continue to push for membership growth; rate negotiations with providers are expected to remain tense; and competition in the health tech industry is growing. Read More
MedPAC Recommends Increase in Physician Payments, Cuts to Skilled Nursing Providers. MedPage Today reported on January 12, 2023, that the Medicare Payment Advisory Commission (MedPAC) recommended an increase in the 2023 Medicare physician base payment rate by 50 percent of the projected increase in the Medicare Economic Index. Separately, the commission recommended a three percent payment cut for skilled nursing providers in 2024. Read More
CMS Allows Medicaid, CHIP to Reimburse Behavioral Specialists for Consulting with Primary Care Providers. Health Payer Intelligence reported on January 11, 2023, the Centers for Medicare & Medicaid Services (CMS) issued guidance allowing Medicaid and the Children’s Health Insurance Program (CHIP) to reimburse specialty behavioral health providers when they are consulted by a primary care provider. The reimbursed consultations can occur even without the presence of the beneficiary. Read More
Medicaid HCBS Members Under Age 65 Have High Mortality Rate During Pandemic. Managed Healthcare Executive reported on January 11, 2023, that individuals under 65 years old receiving Medicaid home and community-based services (HCBS) had a mortality rate 7.4 times that of Medicaid beneficiaries in the community but not receiving HCBS during the first 10 months of the COVID-19 pandemic, according to a study by Health Affairs. Mortality rate was 26.6 times that of the general population. The study suggests a variety of factors may have contributed to the high mortality rates, including “individual risk factors, societal barriers, and indirect impacts”. Read More
Industry News
HMA in Health Affairs Forefront: Imminent VFC Decisions Are Critical for RSV Therapy Access. As respiratory syncytial virus (RSV), a seasonal pathogen in young children, is challenging the national health care system as part of an unprecedented “tripledemic” with COVID-19 and flu this winter, HMA authors weigh in on potential coverage pathways for new monoclonal antibody (mAb) preventive therapies for RSV and their implications for access. The Vaccines for Children (VFC) program is a proven vehicle for ensuring comprehensive coverage of immunizations based on recommendations from the Advisory Committee on Immunization Practices (ACIP). An ACIP workgroup is actively discussing potential recommendations for immunization with RSV mAbs. HMA authors Helen DuPlessis, MD, FAAP, Diana Rodin, and Matt Wimmer explore the implications of ACIP recommendations, Medicaid coverage pathways, and children’s access to the new therapies. Read More
Health Network One Acquires Premier Eye Care. Health Network One announced on January 12, 2023, the acquisition of Premier Eye Care, an optometry and ophthalmology provider network manager covering more than two million members. Health Network One operates specialty healthcare networks, including outpatient therapy, podiatry, and dermatology, for over 20 Medicaid, Medicare Advantage and commercial health plans. Read More
InTandem Capital Partners Announces Investment in HouseWorks. InTandem Capital Partners announced on January 12, 2023, an investment in home care provider HouseWorks. InTandem is a private equity firm focused on healthcare services. Read More
Sentara Healthcare Completes Acquisition of AvMed. Sentara Healthcare announced on January 12, 2023, that it has completed the acquisition of AvMed, a commercial, individual, and Medicare Advantage not-for-profit health plan based in Florida. Sentara acquired AvMed from SantaFe HealthCare. Read More
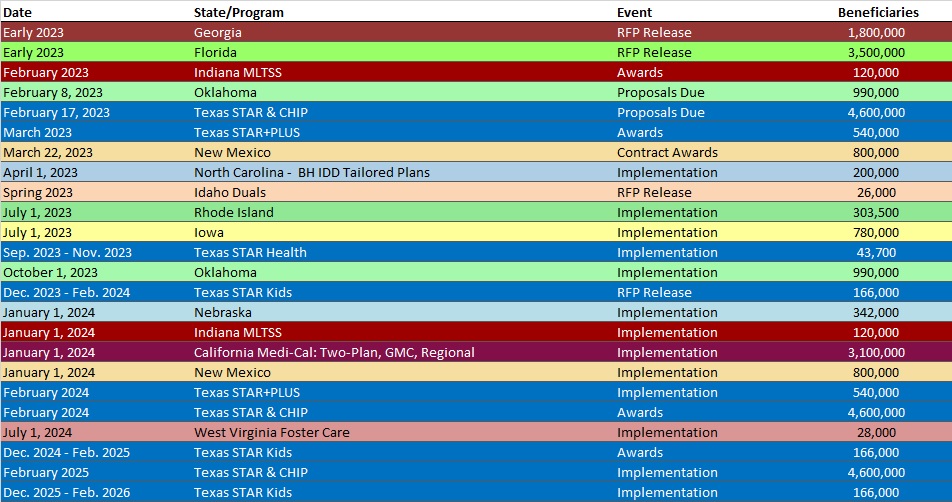
RFP Calendar
Company Announcements
HMA News & Events
WAKELY, AN HMA COMPANY, WHITE PAPERS
