HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Lee Fleisher of CMS to Deliver Keynote Address at HMA National Quality Conference

- Arkansas Legislature Faces Potential Hurdles for Funding Medicaid Expansion

- Arizona Governor Proposes $2.7 Million to Modernize Medicaid Enterprise System

- Georgia House Speaker Does Not Plan to Take Up Medicaid Expansion

- Massachusetts Governor Appoints Kate Walsh as Secretary of Health, Human Services

- Michigan Provides Pregnancy App for Eligible Medicaid Beneficiaries

- New Mexico Medicaid Director to Step Down

- New Mexico Has Yet to Announce Medicaid Managed Care Awards

- Oklahoma Awards Medicaid Dental Contracts to 2 Plans

- Rhode Island Legislators Introduce Medicaid Housing Supports Pilot Proposal

- Wisconsin Adds Medicaid Work Requirement Advisory Referendum to April Ballot

- Wyoming Appoints Lee Grossman as State Medicaid Agent, Senior Administrator

- Exchange Plan Enrollment Rises Nearly 13 Percent to 16.3 Million in 2023

- FCC Clears Medicaid Plans to Text, Robocall Beneficiaries for Eligibility Redeterminations

- Elevance Health to Acquire BCBS of LA

In Focus
Lee Fleisher of CMS to Deliver Keynote Address at HMA National Quality Conference
Lee Fleisher, MD, chief medical officer and director of CMS’ Center for Clinical Standards and Quality, will deliver the morning keynote address at HMA’s March 6 conference on “Healthcare Quality: A Deep Dive on What’s Next for Providers, Payers, and Policymakers” at the Fairmont Chicago, Millennium Park.
Fleisher will present A Vision for Healthcare Quality: How Policy Can Drive Improved Outcomes. Other featured speakers will include executives from the American College of Surgeons, ANCOR, Brave Health, CareJourney, CareOregon, Commonwealth Care Alliance, Council on Quality and Leadership, Denver Health, Healthy People, Institute on Public Policy for People with Disabilities, Intermountain Healthcare, Kaiser Permanente, NCQA, Reema Health, Social Interventions Research and Evaluation Network, UnitedHealth Group, and United Hospital Fund.
HMA’s first annual quality conference will provide organizations the opportunity to “Focus on Quality to Improve Patients’ Lives.” Attendees will hear from industry leaders and policymakers about evolving healthcare quality initiatives and participate in substantive workshops where they will learn about and discuss solutions that are using quality frameworks to create a more equitable health system.
Working sessions will provide expert-led discussions about how quality is driving federal and state policy, behavioral health integration, approaches to improving equity and measuring social determinants of health, integration of disability support services, stronger Medicaid core measures, strategies for Medicare Star Ratings, value-based payments, and digital measurement. Speakers will provide case studies and innovative approaches to ensuring quality efforts result in lasting improvements in health outcomes.
“What’s different about this conference is that participants will engage in working sessions that provide healthcare executives tools and models for directly impacting quality at their organizations,” said Carl Mercurio, Principal and Publisher, HMA Information Services.
Early Bird registration ends January 30. Visit the conference website for complete details or contact Carl Mercurio at 212-575-5929 or [email protected]. Group rates and sponsorships are available. The conference agenda appears below.
| Healthcare Quality Conference Agenda: What’s Next for Providers, Payers, and Policymakers: Focus on Quality to Improve Patients’ LivesFairmont Chicago, Millennium Park | |
| Monday, March 6 | |
| 7:00 – 8:00 am | Registration & Breakfast |
| 8:00 – 8:45 am | Keynote Address A Vision for Healthcare Quality: How Policy Can Drive Improved OutcomesFederal regulators are leading the charge on healthcare quality. During this keynote address, a leading CMS healthcare policymaker will discuss quality goals and initiatives in the Medicare and Medicaid programs, including a vision for how clinical standards and other quality requirements and incentives can translate into improved outcomes. The speaker will also provide an update on current CMS quality improvement programs as well as an overview of what’s likely to come.SpeakerLee Fleisher, MD, Chief Medical Officer, Director, Center for Clinical Standards and Quality, Centers for Medicare and Medicaid ServicesModeratorAmy Bassano, Managing Director, Medicare, HMA, Washington, DC |
| 8:45 – 10:00 am | Plenary Session Identifying and Addressing Roadblocks to Healthcare Quality Improvement Why has healthcare quality remained so elusive and what can be done to change that? During this plenary session, speakers will identify several pressing healthcare quality challenges, ranging from forward-looking questions over whether current quality initiatives truly improve outcomes to more immediate, practical concerns like how to move the needle on quality ratings and measures. Presentations will set the stage for later working sessions in which attendees will learn how to encourage innovation, solve specific quality problems in the context of a system-wide quality infrastructure, and foster continuous quality improvement. Speakers Oxiris Barbot, MD, CEO, United Hospital Fund Aneesh Chopra, President, CareJourney Eric Schneider, MD, Executive Vice President, National Committee for Quality Assurance Moderator Meggan Schilkie, Vice President, Strategic Focus Areas, HMA, New York, NY |
| 10:00 – 10:30 am | Break |
| 10:30 am – 12:00 pm | Concurrent Working Session Developing a Behavioral Health Quality Strategy Behavioral health has emerged as a critical component of any attempt to improve overall healthcare outcomes. During this breakout session, speakers will provide a framework for building a system-wide behavioral health quality strategy that dovetails with broader quality considerations. Attendees will also have the opportunity to apply this framework to their organizations. Topics will include identifying quality measures that inform behavioral interventions, use of collaborative care models to drive behavioral health quality improvement, and value-based payment models for behavioral health providers. Speakers Nazlim Hagmann, MD, Chief Medical Officer, Commonwealth Care Alliance Rhonda Robinson Beale, MD, SVP, Chief Medical Officer, Mental Health Services, UnitedHealth Group Moderator Gina Lasky, Managing Director, Behavioral Health, HMA, Denver, CO |
Concurrent Working Session Getting to Value in Healthcare: How Value-Based Care, Population Health, Incentives Drive Quality The simplest definition of achieving value in healthcare is the use of payment incentives to drive improvement in quality and outcomes for a population of patients. Which models and approaches best achieve this goal, however, is an open question. During this breakout session, speakers will provide an overview of getting to value in healthcare, including use of value-based care, population health, whole person care, and alternative payment models. Speakers will also show how to break down silos and develop a system-wide approach to quality improvement. Attendees will also have the opportunity to determine which of these models and approaches will provide the most value to their organizations. Speakers Keshia Bigler, Director Informatics and Evaluation, Quality & Innovation Support, CareOregon Connie Savor, MD, Chief Medical Officer, Denver Health Moderators Melinda Estep, Managing Directory, Delivery System, HMA, Denver, CO Kelsey Stevens, Principal, Wakely Consulting Group, An HMA Company, Tampa, FL | |
Concurrent Working Session The Final Frontier: Bringing State Intellectual and Developmental Disability Service Systems into the Quality Conversation Most states continue to rely on a fee-for-service payment model for intellectual and developmental disability (IDD) service systems, where quality metrics are nominal. Even states where payment systems have evolved toward a variety of managed care models have not made substantial headway in defining, measuring, and paying for quality outcomes. With the Settings Rule taking effect in 2023, CMS has established a clear and forward-looking framework for the delivery of HCBS services with a focus on consumer engagement, experience, and satisfaction. During this breakout session, speakers and moderators will share a framework for considering alternate payer models, taking into account the unique nature, duration, and array of IDD community services. Speakers will share research findings and input from a series of meetings involving a panel of national experts that highlight key components, characteristics, and considerations that policymakers, payers, and stakeholders should consider in the design and implementation of IDD community services with a goal of quality measurement and enhancement. Speakers: Mary Kay Rizzolo, CEO, Council on Quality and Leadership Donna Martin, Senior Director for State Partnerships and Innovation, ANCOR Moderators: Shane Spotts, Principal, HMA, Lansing, MI Kathy Carmody, CEO, Institute on Public Policy for People with Disabilities | |
Concurrent Working Session Medicaid Core Sets and the Growing Emphasis on Accountability Speakers Additional speaker to be announced. Moderator | |
| 12:00 – 1:30 pm | Lunch |
| 1:30 – 3:00 pm | Concurrent Working Session Quality Innovations: Healthcare Disrupters that Are Driving Improved Outcomes Frustrated with typical, ineffective approaches to quality, several healthcare organizations have taken matters into their own hands – developing innovative programs that are driving improvement in healthcare outcomes. During this breakout session, attendees will hear from organizations that are moving the needle on quality through the use of targeted interventions, whole-person care, digital quality measurements, improved access to care, and a variety of other effective techniques. Attendees will also have the opportunity to develop strategies for applying these approaches to their organizations. Speakers Frank Opelka, MD, Medical Director, American College of Surgeons Eric Schneider, MD, Executive Vice President, National Committee for Quality Assurance Jake Schwartz, CEO, Brave Health Moderators David Kulick, Managing Director, The Focus Group, an HMA Company, New Orleans, LA Ryan Howells, Principal, Leavitt Partners, An HMA Company, Washington, DC |
Concurrent Working Session Practical Approaches to Addressing Equity and Social Determinants of Health This breakout session will provide a platform for payers and providers to discuss institutional barriers and potential solutions for implementing screening and referral programs that address health-related social needs. Topics will include best practices for including screening in clinical and administrative workflows, implementing IT systems like social care referral platforms, obtaining patient consent to share data with social care providers, and measuring results. Attendees will learn how to put these practices into action when addressing health-related social needs at their organizations. Speakers Caroline Fichtenberg, Co-director, Social Interventions Research and Evaluation Network Jami Snyder, Former Director, Arizona Health Care Cost Containment System Moderators | |
Concurrent Working Session Moving the Needle on Medicare Stars Ratings During this breakout session, attendees will obtain a blueprint for improving Medicare Advantage plan Star Ratings and gain an understanding of how to apply this blueprint to their organizations. Topics will include the importance of ensuring executive management buy-in; use of data analytics to identify quality gaps, implement interventions, and track improvement; and strategies for avoiding the type of siloed initiatives that often fail to achieve lasting results. Speakers will also address the importance of quality in achieving market viability and financial sustainability. Speakers Katharine Iskrant, President, Healthy People Additional speaker to be announced. Moderator Mary Walter, Managing Director, Quality and Accreditation, HMA, Salt Lake City, UT | |
| 3:00 – 3:30 pm | Break |
| 3:30 – 4:30 pm | Bringing It All Together Next Steps in Positioning Your Organization for Continuous Quality Improvement During this closing keynote presentation, a leading quality expert will discuss how healthcare organizations can begin to prioritize quality initiatives and position their organizations for continuous quality improvement. This session will also address the role of executive leadership in maintaining a focus on quality, the need for cross-functional cooperation, and practical steps organizations can take ensure quality efforts tie into broader strategic and financial goals. Speaker Gregory Poulsen, Senior Vice President, Intermountain Healthcare Moderator Josh Trent, Principal, Leavitt Partners, an HMA Company, Washington, DC |
HMA Roundup
Arkansas
Arkansas Legislature Faces Potential Hurdles for Funding Medicaid Expansion. KUAR reported on January 17, 2023, that the Arkansas legislature may face hurdles to funding ARHOME, the state’s Medicaid expansion program using Exchange plans. In previous years, it took the legislature multiple attempts to approve the funding. Read More
Arizona
Arizona Governor Proposes $2.7 Million to Modernize Medicaid Enterprise System. State of Reform reported on January 18, 2023, that Arizona Governor Katie Hobbs is seeking $2.7 million in fiscal 2024 for modernizing the state’s Medicaid enterprise system. About $2 million of the funds would go toward systems integration and $700,000 would be used to replace the first modules. She is also seeking $257 million for Medicaid caseload growth and the end of the public health emergency, as well as funding for parent caregivers and home and community-based services grants. Read More
Georgia
Georgia House Speaker Does Not Plan to Take Up Medicaid Expansion. The Atlanta Journal-Constitution reported on January 20, 2023, that Georgia House Speaker Jon Burns (R-Newington) is not planning to bring a Medicaid expansion bill to a vote during the current session. Georgia’s limited Medicaid expansion program with work requirements called Georgia Pathways to Coverage is anticipated to be implemented in summer 2023. Read More
Iowa
Iowa House Committee Advances Bill for State Licensing of Rural Emergency Hospitals. The Gazette reported on January 24, 2023, that the Iowa House Health and Human Services Committee advanced a bill that would set up a state licensing process for rural emergency hospitals. The bill would also increase Medicaid and Medicare reimbursement rates for patients treated at a rural emergency hospital. Read More
Illinois
Illinois Governor Signs Healthcare Omnibus Bill. Health News Illinois reported on January 18, 2023, that Illinois Governor J.B. Pritzker signed a healthcare omnibus bill that changes the definition of rural emergency hospitals, expands eligible provider types for applied behavior analysis, and extends a fee waiver for providers to include podiatrists. The bill also allows county nursing homes to participate in the nursing home tax and assessment and provides one-time emergency funding for mental health and substance use disorder crisis intervention services. Read More
Massachusetts
Massachusetts Governor Appoints Kate Walsh as Secretary of Health, Human Services. WCVB reported on January 25, 2023, that Massachusetts Governor Maura Healey appointed Kate Walsh as secretary of the Executive Office of Health and Human Services (EOHHS). Previously, Walsh was chief executive of the Boston Medical Center health system. Read More
Michigan
Michigan Provides Pregnancy App for Eligible Medicaid Beneficiaries. mHealth Intelligence reported on January 24, 2023, that Michigan is providing a pregnancy app for eligible Medicaid beneficiaries. The app provides content, tools, and health department programs throughout the pregnancy and postpartum period. The state also recently extended postpartum Medicaid coverage to 12 months. Read More
Missouri
Missouri Senate Committee Considers Bill to Extend Postpartum Medicaid Coverage from 60 Days to 12 Months. The St. Louis Post-Dispatch reported on January 18, 2023, that the Missouri Senate Health and Welfare Committee is considering a bill to extend postpartum Medicaid coverage from 60 days to 12 months. An estimated 4,565 individuals would benefit from the extended coverage. Read More
Mississippi
Mississippi Advisory Committee Recommends Extending Postpartum Medicaid Coverage to 12 Months. Mississippi Today reported on January 20, 2023, that the Mississippi Medical Care Advisory Committee, which advises the state Medicaid program, recommended an increase in postpartum Medicaid coverage from 60 days to 12 months. In 2022, the state Senate passed a bill to extend coverage, but it was blocked in the House. Read More
Montana
Montana Legislative Subcommittee Hears Provider Testimony on Raising Medicaid Reimbursement Rates for Nursing Homes. McKnight’s Senior Living reported on January 23, 2023, that the Montana state legislature health and human services joint appropriations subcommittee heard testimony from state providers on why nursing home Medicaid reimbursement rates need to be increased. According to the testimony, the facilities are financially struggling due to increased operational costs. The legislature will consider the increases during the current session. Read More
New Jersey
New Jersey Expands Medicaid Eligibility to Children Regardless of Immigration Status. Trenton Daily reported on January 24, 2023, that New Jersey expanded NJ FamilyCare eligibility to all children under the age of 19, regardless of immigration status, effective January 1, 2023. The change, which will impact a projected 16,000 children, is part of the second phase of the state’s Cover All Kids initiative. Phase one included eliminating Children’s Health Insurance Program (CHIP) premiums and the 90-day waiting period after CHIP enrollment. Read More
New Mexico
New Mexico Medicaid Director to Step Down. The Albuquerque Journal reported on January 25, 2023, that New Mexico Medicaid director Nicole Comeaux is leaving her position, which she has held since 2019. The Human Services Department has not yet announced a replacement. Read More
New Mexico Announces Five-Year Primary Care Strategic Plan. The New Mexico Department of Human Services released on January 20, 2023, a five-year strategic plan to transform primary care delivery in the state. Comments will be accepted through February 20, 2023. Read More
New Mexico Has Yet to Announce Medicaid Managed Care Awards. Health Payer Specialist reported on January 20, 2023, that the New Mexico Department of Human Services has not yet released the notices of intent to award for the Turquoise Care Medicaid managed care program contracts, originally scheduled January 16, 2023. The finalized contracts will announced March 22. Read More
New Mexico Medicaid Beneficiaries Face Barriers to Healthcare Access, Legislative Report Finds. The New Mexico Legislative Finance Committee released a report on December 13, 2022, stating that Medicaid beneficiaries do not have access to timely healthcare. The report, titled Program Evaluation: Medicaid Network Adequacy, Access, and Utilization pointed to provider network shortages and inaccurate and outdated Medicaid managed care organization (MCO) provider directories. For example, one in four MCO network providers were unreachable and one in six were not accepting new patients. The report suggested holding MCOs accountable, potentially increasing Medicaid payment rates, and investing in provider recruitment and retention strategies. Read More
New York
New York Lawmakers Call For 20 Percent Increase in Medicaid Long-Term Care Medicaid Reimbursement Rates. Spectrum News reported on January 24, 2023, that a group of lawmakers and long-term care facility owners are urging New York Governor Kathy Hochul to include a 20 percent increase in long-term care Medicaid reimbursement rates in her fiscal 2024 budget proposal. About 70 percent of nursing home residents in New York are covered by Medicaid. Read More
New York Made $22 Million in Improper Medicaid Payments from October 2021 to March 2022, Audit Finds. The New York State Comptroller published on January 24, 2023, audits identifying $22 million in improper Medicaid payments from October 2021 to March 2022 and $1.1 million in Medicaid overpayments for brand name prescription drugs where generic were available from July 2016 through July 2021. Read More
New York Governor Announces $7.5 Million in Grants for Opioid Treatment Programs. Crain’s Health Pulse reported on January 24, 2023, that New York Governor Kathy Hochul announced $7.5 million in grants for up to 15 opioid use disorder treatment programs. The funding is the first round of grants from the $1.6 billion Opioid Settlement Fund from drug companies. Read More
New York Seeks Waiver from Medicaid IMD Exclusion. Behavioral Health Business reported on January 20, 2023, that New York State is seeking a federal waiver to allow Medicaid coverage with matching funds of behavioral health services for serious mental illness, substance use disorder, and serious emotional disturbance provided in institutions for mental disease (IMD). The request, which would allow the state to get around the IMD exclusion, was made as part of New York’s 1115 waiver application. Read More
New York Proposal to Push Retirees into Medicare Advantage Is Unlikely to Move Forward. The New York Daily News reported on January 19, 2023, that New York City Council members indicated they do not support legislation allowing the city to charge retirees $191 in monthly Medicare premiums if they elect to not enroll in a Medicare Advantage plan. Previously, Supreme Court Judges deemed the plan to be in violation of a city law requiring retirees to receive free health coverage for life. Read More
Oklahoma
Oklahoma Awards Medicaid Dental Contracts to 2 Plans. The Oklahoma Health Care Authority announced on January 19, 2023, its intent to award Medicaid dental managed care contracts to DentaQuest and Liberty Dental Plan of Oklahoma. The contracts will run through June 30, 2025, with five one-year options. Read More
Ohio
Ohio Launches Maternal Care Program for Medicaid Enrollees. The Journal-News reported on January 25, 2023, that Ohio launched a $5 million Comprehensive Maternal Care program that will provide quarterly payments to providers. These payments will fund the design and implementation of individualized maternal care plans and address social needs like food instability and housing insecurity among more than 14,000 pregnant and postpartum Medicaid members served by 77 medical practices. Payments to practices will be based on the number of patients served, with providers required to receive feedback from patients, utilize pregnancy risk assessments, and engage with community supports. Read More
Rhode Island
Rhode Island Legislators Introduce Medicaid Housing Supports Pilot Proposal. GoLocalProv reported on January 24, 2023, that Rhode Island legislators introduced a proposal for Medicaid to cover supportive housing services, behavioral health services, and case management for chronically homeless individuals through a pilot program. The pilot program is modeled after similar efforts in Arizona, Hawaii, and New York. Read More
Rhode Island Representative Introduces Bill to Expand Medicaid Eligibility for Seniors. ABC 6/WLNE reported on January 20, 2023, that Rhode Island Representative David Morales (D-Providence) introduced legislation that would expand Medicaid eligibility for seniors to 138 percent of federal poverty. The current limit for seniors is 100 percent of federal poverty. Read More
South Dakota
South Dakota Legislators Seek Medicaid Work Requirement Ballot Measure. KELOLAND News reported on January 23, 2023, that South Dakota lawmakers proposed a 2024 ballot measure imposing Medicaid work requirements for able-bodied individuals. The joint resolution, which is co-sponsored by 19 Republican lawmakers, calls for voters to approve a constitutional amendment adding work requirements. Read More
South Dakota Seeks Additional Employees to Implement Medicaid Expansion by July 2023. KELOLAND reported on January 17, 2022, that the South Dakota Department of Social Services is requesting 68 additional full-time employees to implement Medicaid expansion for nearly 58,000 individuals. The state intends to submit Medicaid State Plan amendments for federal approval in March 2023 and implement expansion in July 2023. Read More
Wisconsin
Wisconsin Adds Medicaid Work Requirement Advisory Referendum to April Ballot. Health News Wisconsin reported on January 20, 2023, that the Wisconsin legislature voted to add an advisory referendum to the April ballot asking voters whether they think Medicaid work requirements should be enacted. Republicans have in prior sessions introduced legislation to instate work requirements and prevent eligible Medicaid enrollees from turning down work while enrolled in coverage. Read More
West Virginia
West Virginia Reaches $83 Million Settlement with Pharmacy in Opioid Lawsuit. The Hill reported on January 18, 2023, that West Virginia reached an $83 million settlement agreement with Walgreens in a lawsuit regarding the pharmacy’s role in the state’s opioid crisis. The settlement will be paid over an eight-year period. West Virginia previously settled similar litigation with CVS, Walmart, and Rite Aid and is scheduled to go to trial with Kroger in June 2023. Read More
Wyoming
Wyoming Appoints Lee Grossman as State Medicaid Agent, Senior Administrator. The Wyoming Department of Health announced on January 18, 2023, the appointment of Lee Grossman as state Medicaid agent and senior administrator of the Division of Healthcare Financing, effective in March 2023 with the retirement of interim agent Jan Stall. Paul Johnson, MD, was appointed as Wyoming Medicaid medical director. Read More
Wyoming House Appropriations Committee Advances Medicaid Postpartum Coverage Bill. Wyoming Business Report reported on January 18, 2023, that the Wyoming House Appropriations Committee advanced legislation to extend Medicaid postpartum coverage to 12 months. The coverage extension would require almost $1.9 million in state funds in its first year. Read More
National
Exchange Plan Enrollment Rises Nearly 13 Percent to 16.3 Million in 2023. The Centers for Medicare & Medicaid Services announced on January 25, 2023, that more than 16.3 million individuals enrolled in Exchange plans on both federal and state Exchanges during the 2023 open enrollment period. The number of enrollees increased by nearly 13 percent from 2022 and almost 50 percent from 2021. Read More
CMMI to Release Advanced Primary Care, Total Cost of Care Payment Models. Fierce Healthcare reported on January 24, 2023, that the Center for Medicare and Medicaid Innovation (CMMI) will introduce three to four payment models aimed at advanced primary care and total cost of care. CMMI director Liz Fowler said the models will focus on addressing health equity and financial calculations that encourage participation by safety net providers. Read More
FCC Clears Medicaid Plans to Text, Robocall Beneficiaries for Eligibility Redeterminations. Fierce Healthcare reported on January 24, 2023, that the Federal Communications Commission (FCC) issued guidance allowing Medicaid plans to use texts and robocalls to communicate with beneficiaries regarding eligibility redeterminations. Read More
AHIP Urges States to Communicate With Medicaid Members Ahead of Redeterminations. Becker’s Payer Issues reported on January 23, 2023, that America’s Health Insurance Plans (AHIP) chief executive Matt Eyles urged states to communicate with Medicaid members about the redetermination process that will follow the end of the public health emergency in 2023. Other topics Eyles addressed in AHIP’s annual state of the industry discussion included expanding mental health networks, improving health equity, and addressing the cost of prescription drugs. Read More
States Increasingly Pay for Community Health Worker Services Through Medicaid. Kaiser Family Foundation (KFF) reported on January 23, 2023, that states increasingly are paying for community health worker (CHW) services through Medicaid, including coverage via state plan authority, Section 1115 waivers, and other pathways, according to the KFF annual Medicaid budget survey. KFF found that as of July 2022, more than half of responding states allow Medicaid coverage of CHW services. Read More
U.S. Representative Introduces Bill to Allow Counties, Cities to Expand Medicaid Without Statewide Approval. The Winston-Salem Journal reported on January 22, 2023, that U.S. Representative Lloyd Doggett (D-TX) introduced a bill (H.R. 31) that would allow the Centers for Medicare & Medicaid Services to work directly with counties and cities to implement Medicaid expansion without state legislature approval. The Republican majority in the House makes it unlikely that the bill will be passed, according to political analysts. Read More
MACPAC Meeting Scheduled for January 26, 27. The Medicaid and CHIP Payment and Access Commission (MACPAC) announced on January 20, 2023, that its next meeting will be held on January 26-27. Among the topics for discussion will be policy options for improving race and ethnicity data collection and reporting in Medicaid, potential nursing facility payment principles and recommendations, and Medicaid drug coverage based on Medicare national coverage determinations. Read More
Medicaid Expansion Is Associated with Positive Financial Outcomes for Providers, Study Finds. RevCycleIntelligence reported on January 20, 2023, that eight separate studies found that Medicaid expansion is associated with positive financial outcomes for hospitals and health centers, according to an analysis by the Kaiser Family Foundation. Positives have included higher reimbursements and decreased uncompensated care costs for hospitals and increased revenues for health centers. Read More
Medicare Home Health Rates Continue to Lag Costs, Study Says. Modern Healthcare reported on January 20, 2023, that Medicare reimbursement rates for 2023 continue to lag provider costs, according to a report from S&P Global. The Centers for Medicare & Medicaid Services authorized a 0.7 percent increase for 2023. Read More
Nearly Half of Medicare Advantage Provider Directories Have Inaccuracies, Federal Review Finds. Modern Healthcare reported on January 20, 2023, that nearly half of Medicare Advantage (MA) provider directories had inaccuracies in 2018, according to the most recent federal review. The Centers for Medicare & Medicaid Services has proposed a national provider directory to increase accuracy. Read More
CMS Sets Federal Poverty Guideline for Family of 4 at $30,000. The Centers for Medicare & Medicaid Services (CMS) released on January 19, 2023, the 2023 federal poverty level standards, which set the poverty guideline at $30,000 for a family of four living in one of the 48 contiguous states or the District of Columbia. The guideline reflects an eight percent increase from 2021 to 2022. Read More
Medicaid Expansion Is Associated with 13 Percent Decrease in Home Evictions, Study Finds. Health Payer Intelligence reported on January 18, 2023, that Medicaid expansion was associated with a 13 percent decrease in home evictions to 464 per county per month in 774 counties across 26 expansion states from 2002 to 2018. In 14 non-expansion states, evictions increased three percent to 490 per county per month across 720 counties. Read More
Provider Groups Urge CMS to Finalize Prior Authorization Rule. Fierce Healthcare reported on January 18, 2023, that medical groups are urging the Centers for Medicare & Medicaid Services (CMS) to finalize a rule that would mandate electronic prior authorizations by 2026 and require payers to decide on urgent prior authorization requests within 72 hours. Nonurgent prior authorization requests would need to be decided within seven days under the rule. The rule would apply to Medicaid managed care, Medicare Advantage, and Exchange plans. Read More
Industry News
Apara Autism Center Acquires Autism Learning Collaborative, Early Autism Services. Havencrest Capital Management portfolio company Apara Autism Center announced on January 25, 2023, the acquisition of Autism Learning Collaborative and the Missouri operations of Early Autism Services, both of which are applied behavior analysis (ABA) therapy providers for children with autism spectrum disorder. Apara provides ABA services throughout Texas. Read More
Centene Completes Divestiture of Magellan Specialty Health. Centene announced on January 23, 2023, that it has completed divestiture of Magellan Specialty Health to Evolent Health for approximately $660 million in cash and stock, plus incentive payouts of up to $150 million in 2024. Centene acquired Magellan Specialty Health in January 2022 through the acquisition of Magellan Health. Read More
Elevance Health to Acquire BCBS of LA. Elevance Health announced on January 23, 2023, a definitive agreement to acquire Blue Cross Blue Shield of Louisiana. The acquisition builds on the two organizations’ joint ownership of Healthy Blue, which serves Medicaid and dual eligible enrollees. The acquisition is expected to close this year. Read More
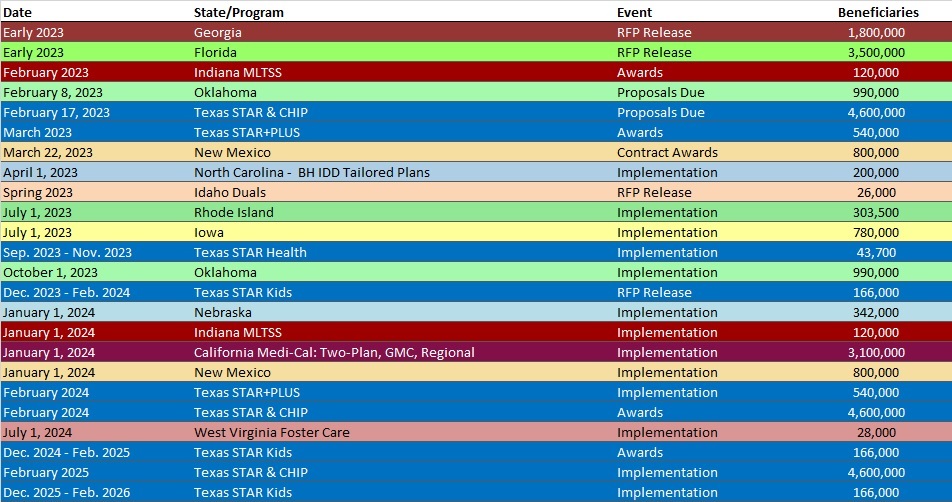
RFP Calendar
HMA News & Events
WAKELY, AN HMA COMPANY, WHITE PAPERS
