This week's roundup:
- In Focus: Building State Capacities for Medicaid Work and Community Engagement Requirements
- HMA Experts in Action: Doug Shoemaker Appointed to Housing Authority of the City and County of San Francisco
- Iowa Seeks Additional Comments on 1115 Iowa Wellness Plan Demonstration Extension Request
- Michigan to Release Behavioral PIHP RFP in Summer 2025
- Montana Governor Enacts Medicaid Matching Ambulance Fee to Support Emergency Medical Services
- CMS Tightens Oversight on Federal Medicaid Funds Used for Undocumented Immigrants
- CMS Releases Updated Hospital Price Transparency Rules; Issues RFI
- CMS to Conduct Annual Audits of All Medicare Advantage Plans in Oversight Expansion
- Actuaries Corner: Judge Shuts Down Drugmakers’ 340B Rebate Plans, For Now
In Focus
Building State Capacities for Medicaid Work and Community Engagement Requirements
On May 22, 2025, the US House of Representatives advanced a comprehensive legislative package that includes expansive changes to healthcare spending and tax policies. The One Big Beautiful Bill Act, H.R. 1, will be subject to further revision in the Senate – and potentially again in the House – before it can be sent to the president for his signature. If enacted, the legislation would have significant implications for the Medicaid program, including a nationwide work and community engagement requirement. The House-passed bill establishes a deadline of December 31, 2026, for implementation, but individual states could move earlier.
As state legislatures pass work requirement bills, governors consider executive actions, and Congress contemplates revisions to the Medicaid work mandate, vetting key implementation issues may significantly affect the direction of related policies. Even before implementation, states must test operations, enable systems, and establish connections to beneficiaries to reduce potential implementation missteps, inappropriate disenrollments, and litigation risks.
If the goal of Medicaid work requirement policies is to stimulate connections between health benefits and employment/workforce, building state and federal capacities to support these approaches is critical to effectuating that change. In the remainder of this article, Health Management Associates (HMA), experts focus on the operational dynamics that need to be discussed, tested, and built as states begin introducing work and community engagement initiatives.
Federal Policies and Early State Actions on Work Requirements
The House bill would require all states to implement work and community engagement requirements for adults without dependents for at least 80 hours per month.[1] Employment, work programs, education, or community service (or a combination of those activities) would satisfy the requirement.
The work requirements in the House-passed legislation would apply only to individuals between the ages of 19 and 64 without dependents, and the following groups are exempted:
- Women who are pregnant or entitled to postpartum medical assistance
- Members of Tribes
- Individuals who are medically frail (i.e., people who are blind, disabled, with chronic substance use disorder, has serious or complex medical conditions, or others as approved by the Secretary of the US Department of Health and Human Services)
- Parents of dependent children or family caregivers to individuals with disabilities
- Veterans
- People who are participating in a drug or alcoholic treatment and rehabilitation program
- Individuals who are incarcerated or have been released from incarceration in the past 90 days
In addition, individuals who already meet work requirements through other programs, such as Temporary Assistance for Needy Families (TANF) or the Supplemental Nutrition Assistance Program (SNAP), would be exempt. However, the House-passed version would make the eligibility verification and work requirements for SNAP more stringent and shift program costs to these states, which would affect cross-functional eligibility. The legislation also includes temporary hardship waivers for natural disasters and areas with an unemployment rate greater than 8 percent (150 percent of the national average).
Though the federal budget package has received a great deal of attention, at least 14 states already have moved forward (see Table 1) in advance of the current federal debate by passing laws and submitting work requirement demonstration requests to the Centers for Medicare & Medicaid Services (CMS).
Table 1. A Review of 2025 States’ Approaches to Work Requirements in Medicaid
Key Questions to Guide State Policy Decisions
Considerable research and findings from previous Medicaid work requirement initiatives can help prepare policymakers to implement a potential new phase of Medicaid work requirement policies. Some previous findings include the high cost of administration relative to potential savings, the importance of systems that support foundational items like logging an enrollee’s compliance activities and exemptions, as well as developing an efficient appeals process. The Medicaid and CHIP Payment and Access Commission (MACPAC), General Accounting Office, National Institutes for Health, and multiple researchers have published assessments regarding previous experiences that could prove useful in policy making.
HMA experts have experience identifying key issues and considerations, analyzing options, and implementing critical issues and for state leaders and stakeholders who will be responsible for implementing work requirements. Several of these issues are described below and in more detail in the HMA blog, Building State Capacities for Medicaid Work and Community Engagement Requirements.
- Exemptions, particularly medical frailty definitions and assessments. The federal government and states will need to identify individuals classified as “medically frail” and make them exempt from the mandates. Medically frail individuals include those with chronic, serious, or complex medical conditions. Various methods can be employed to identify these people.
- Developing and streamlining systems and processes to promote continued coverage for eligible individuals. The Medicaid unwinding from the COVID public health emergency taught policymakers lessons about the complexities of Medicaid systems, patient engagement, and reliable methods of member outreach. State Workforce Commissions and Departments of Labor are clear partners, as they manage integrated eligibility systems and data-sharing agreements across programs like SNAP and TANF, which also serve many Medicaid participants. These and other partnerships will need further exploration.
- Clinical and utilization data that promote eligibility assessment. Many, but not all, individuals with chronic diseases may be exempt from the requirements. Knowing the health status and chronic conditions of the populations affected and the conditions that qualify people for exemption are variables as implementation questions, like the definition of medically frail, are addressed.
- Anticipated need for effective Medicaid managed care engagement in work requirements/community engagement initiatives. Approximately 80 percent of Medicaid expansion enrollees are members of comprehensive managed care organizations (MCOs). States will need to review the scope of existing vendor contracts as well as determine the need for new services, roles, third-party reporting, oversight, and potential exemptions for emergencies. Work requirements can disrupt MCO risk pool stability and care coordination. MCOs have a financial incentive to drive down inappropriate disenrollments and are uniquely positioned to support state responsibilities, including maintenance of up-to-date contact information.
- Measuring impact and adapting policies as needed. Dynamic metrics that provide actionable information to federal and state policy makers will support effective oversight and monitoring.
Connect with Us
HMA helps stakeholders—including state agencies and their partners—manage the challenges of implementing new Medicaid or CHIP initiatives, with a focus on ensuring efficient integration and improvements in outcomes. Our teams are adept at developing materials for and supporting stakeholder engagement from design to implementation, which is a critical aspect for work and community engagement initiatives and other potential new eligibility and renewal requirements.
For support tracking federal and state level developments and enhancing your organization’s strategy and preparations for new Medicaid requirements, contact our featured experts Loren Anthes and Matt Powers.
[1] U.S. Congress. House. One Big Beautiful Bill Act. H.R.1. 119th Cong., 1st sess. Introduced May 20, 2025.
HMA Experts in Action: Doug Shoemaker Appointed to Housing Authority of the City and County of San Francisco
On May 21, 2025, Health Management Associates (HMA), Principal Doug Shoemaker was appointed to the Board of Commissioners for the Housing Authority of the City and County of San Francisco by Mayor Daniel Lurie. Mr. Shoemakers will bring his extensive experience in affordable housing, community development, and the intersection of health and housing to advance the Housing Authority’s mission.
A recognized leader in the affordable housing field, Mr. Shoemaker has worked at the intersection of housing, community development, and healthcare to advance projects and policies that improve outcomes for lower-income individuals and communities. At HMA, Mr. Shoemaker has leveraged his expertise in housing development, financing, operations, and policy to create effective partnerships and community-based programs that address homelessness, senior living, and other complex challenges.
“Doug Shoemaker brings unmatched experience and a lifelong commitment to affordable housing and the families who benefit from it to the Housing Authority. I look forward to working with him to ensure the next generation of San Franciscans can afford to raise their kids here,” said Mayor Lurie.
The Authority’s primary programs are its Housing Choice Voucher and Public Housing programs, serving over 15,000 residents in all neighborhoods and districts within San Francisco. In recent years, the Authority has focused on leased housing through the federal US Department of Housing and Urban Development program called Rental Assistance Demonstration, which allows for the transfer of public housing unit property management to third-party management companies while the Authority retains land ownership.
Mr. Shoemaker previously served as president of Mercy Housing California, California’s largest nonprofit affordable housing developer. In this role, he oversaw the completion of more than 6,000 affordable homes and led a 3,500-unit development pipeline across major California markets including the Bay Area, Los Angeles, and Sacramento. Mr. Shoemaker successfully led a $45 million capital campaign for a new community center and gym and launched a $47 million land acquisition fund.
HMA Roundup
Iowa
Iowa Seeks Additional Comments on 1115 Iowa Wellness Plan Demonstration Extension Request. The Centers for Medicare & Medicaid Services (CMS) announced on May 22, 2025, that Iowa is requesting to extend its Section 1115 Iowa Wellness Plan demonstration, and while the application was originally posted in June 2024, it is being reposted to include additional evaluation documents. The extension includes no new changes and would continue key program features of Medicaid expansion such as premiums, healthy behavior incentives, and waivers for non-emergency medical transportation and retroactive eligibility for certain enrollees. The demonstration also offers dental benefits for adults and children through a Prepaid Ambulatory Health Plan (PAHP). The public comment period will run through June 21, 2025.
Michigan
Michigan to Release Behavioral PIHP RFP in Summer 2025. The Michigan Department of Health and Human Services (MDHHS) announced on May 23, 2025, that it will release a Request for Proposals (RFP) in summer 2025 for new contracts with Prepaid Inpatient Health Plans (PIHPs) to manage Medicaid-funded specialty behavioral health services. The state currently contracts with regional PIHPs to deliver these services in communities across the state, covering approximately 300,000 individuals with serious mental illness, substance use disorders, and developmental disabilities. The upcoming competitive procurement will be guided by stakeholder feedback and structured around four key goals: delivering timely, high-quality care; improving consistency across regions; enhancing accountability; and simplifying the system. Contracts are expected to begin on October 1, 2026.
Montana
Montana Governor Enacts Medicaid Matching Ambulance Fee to Support Emergency Medical Services. KTVH reported on May 22, 2205, that Montana Governor Greg Gianforte signed House Bill 56 into law which creates a 5.75 percent assessment fee on operating revenues of private and nonprofit ambulance providers to draw down additional federal Medicaid funds. The fee is expected to generate $6 million annually, potentially securing up to $30 million in federal matching funds to support emergency medical services statewide. The law excludes government and tribally run services and will require state rulemaking and federal approval before payments begin.
National
CMS Tightens Oversight on Federal Medicaid Funds Used for Undocumented Immigrants. The Centers for Medicare & Medicaid Services (CMS) announced on May 27, 2025, that it has increased federal oversight to prevent states from using federal Medicaid funds to cover healthcare for individuals without legal immigration status. CMS emphasized that federal Medicaid dollars are only intended to cover emergency services for such individuals and warned states against exceeding these limits. The agency will conduct targeted reviews of state spending, financial systems, and eligibility policies, with any improper expenditures subject to recoupment. The action aligns with a recent executive order focused on restricting taxpayer-funded benefits to lawfully eligible individuals.
CMS Releases Updated Hospital Price Transparency Rules; Issues RFI. Becker’s Hospital Review reported on May 22, 2025, that the Centers for Medicare & Medicaid Services has updated its hospital price transparency guidance to be in line with an executive order issued by President Trump in February 2025. The new guidance requires hospitals to display payer-specific standard prices as dollar amounts, including the negotiated amount, negotiated base rate, and the dollar amount. CMS also released a request for information (RFI) seeking feedback to help the agency improve compliance with and enforcement of the transparent reporting of pricing data. Responses to the request are due July 21, 2025.
Industry News
CMS to Conduct Annual Audits of All Medicare Advantage Plans in Oversight Expansion. Modern Healthcare reported on May 21, 2025, that the Centers for Medicare & Medicaid Services (CMS) has significantly expanded its Medicare Advantage (MA) audit program, now requiring annual audits of all eligible contracts, up from just 60 per year, to address concerns over improper payments. To support this initiative, the agency plans to increase its team of medical coders from 40 to approximately 2,000 by September 1, 2025, and deploy advanced technologies to expedite the review process. This effort aims to complete audits for payment years 2018 through 2024 by early 2026. Estimates suggest MA plans may overbill the government by $17 billion to $43 billion annually.
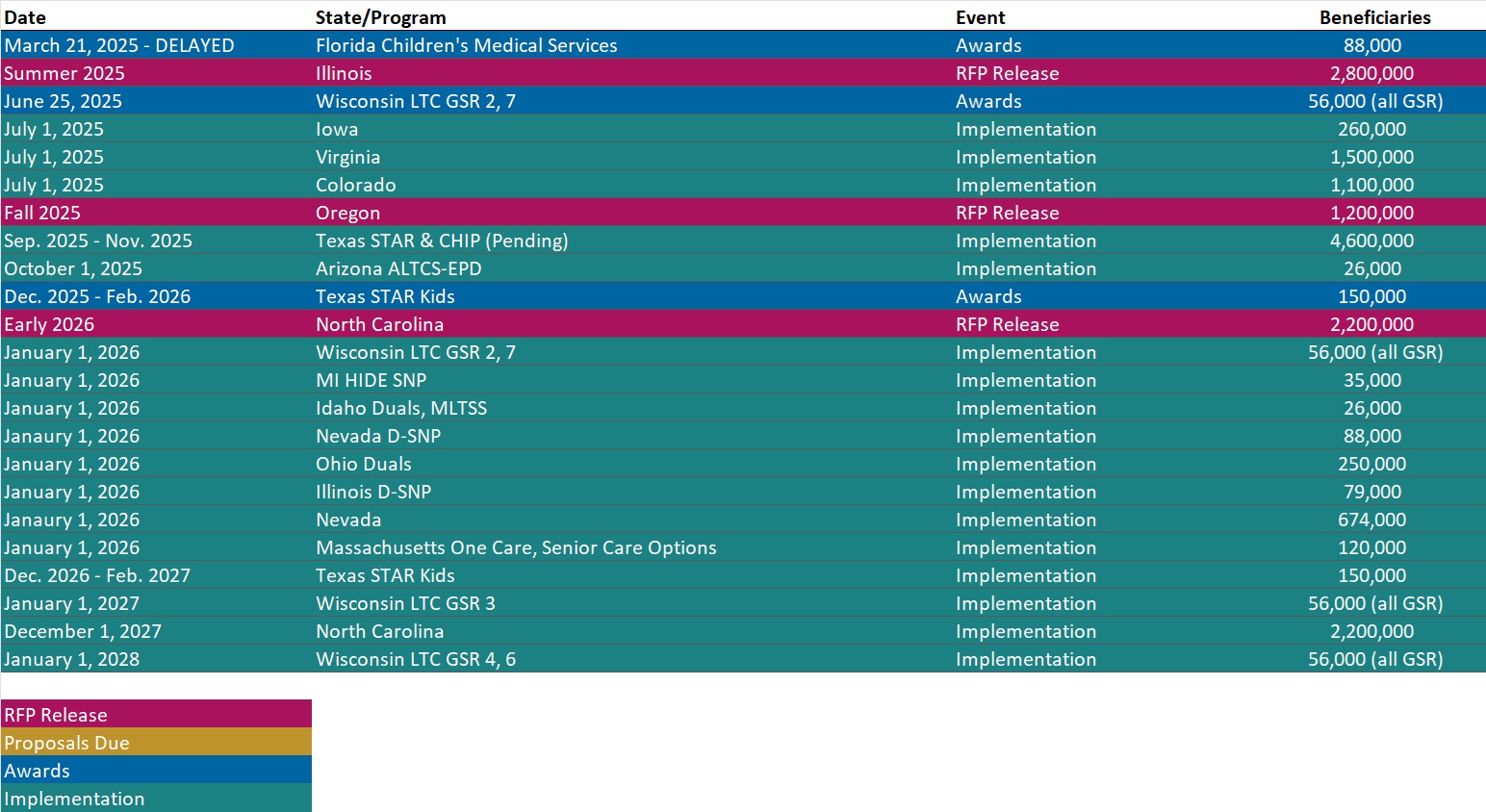
RFP Calendar
Actuaries Corner
Judge Shuts Down Drugmakers’ 340B Rebate Plans, For Now. A district court ruled that the HHS does have the power to review drug manufacturers’ plans to pay hospitals rebates instead of upfront discounts on 340B medications.
Discover other developments in the Wakely Wire here.
HMA News & Events
HMA Conference
Register Today for the HMA 2025 Conference. October 15, 2025 • 8:30 AM.
Where Healthcare’s Next Chapter Takes Shape. At a time of sweeping policy change and system-level transformation, the HMA Conference brings together the leaders who are making it happen.
From federal and state government officials to executives from provider organizations, payers, and community-based groups—you’ll be in the room with decision-makers who are actively designing, influencing, and implementing the future of care.
Whether you work in policy, strategy, operations, payment/finance, or care delivery, this event is designed to give you a clearer picture of what’s coming—and connect you with others navigating the same complexities.
Register Early & Save
Early bird rates are available through July 31, 2025.
We can’t wait to welcome you to New Orleans this October and continue the important work of shaping the future of healthcare—together.
HMA Podcasts
What If Mental Health Checkups Were as Normal as Mammograms? In this episode of Vital Viewpoints on Healthcare, Monica Johnson, managing director at Health Management Associates, takes us through her compelling journey from frontline caregiver to national leader in behavioral health policy. She reflects on the national rollout of the 988 crisis line as one of the most transformative shifts in creating a stigma-free behavioral health system of care that meets people where they are to support whatever crisis they may face. Monica shares personal stories and strategic insights that illuminate why policymakers must ensure these systems prioritize the local needs of patients and providers. We also explore the future of crisis care, the enduring need for bold federal-state collaboration, and why it’s time to normalize mental health checkups.
HMA Webinars
Ask HMA Experts: Behavioral Health Town Hall. Thursday, May 29, 2025, 12 PM ET. Join us for a dynamic and interactive Behavioral Health Town Hall hosted by Health Management Associates (HMA). Our experts will be available to answer your questions live on a wide range of critical topics, including:
- Federal policy, personnel, and funding changes;
- Emerging strategies for addressing social determinants of health, substance use disorder and crisis coordination (including 988);
- Behavioral health revenue cycle management and alternative payment models; and
- Innovations in addressing workforce shortages, integrated service delivery, digital mental health tools, and best practices for community mental health service delivery.
Whether you’re navigating regulations, searching for new funding, designing service delivery systems, or just trying to understand what happens next, this town hall is your chance to ask questions, share insights, and discuss real-world solutions with industry experts.
NEW THIS WEEK ON HMA INFORMATION SERVICES
(Exclusive Access for HMAIS Subscribers):
HMAIS Medicaid Market Overviews, Reports, and Data
- Updated Section 1115 Medicaid Demonstration Inventory
- HMA Federal Health Policy Snapshot
- New Medicaid enrollment, RFP documents, and other market intelligence resources for dozens of states.
- Updated Hawaii and Montana Overviews
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services.
If you’re interested in becoming an HMAIS subscriber, contact Andrea Maresca at [email protected].