This week's roundup:
- In Focus: What’s Next in Quality: CMS Conference Highlights and Stakeholder Imperatives

- In Focus: Health Tech Ecosystem Leaders to Speak at HMA’s National Conference

- Iowa Names Lee Grossman New Medicaid Director

- Michigan Governor Urges Trump to Lengthen Transition Time for Medicaid Cuts

- Oregon Announces $1.8 Million in Marketplace Coverage Enrollment Grants

- Oklahoma to Submit SPA for Enhanced School-Based Medicaid Services

- Urban Hospitals Leverage Rural Designation Policy as H.R.1 $50B Fund Launches

- Six Additional States Receive Federal Approval for SNAP Food Choice Waivers

- Increased Medicaid Spending Did Not Boost Nursing Home Staffing, OIG Finds

- UnitedHealth Group Names Wayne DeVeydt CFO

In Focus
What’s Next in Quality: CMS Conference Highlights and Stakeholder Imperatives
This week, our In Focus section covers the 2025 CMS Quality Conference. The event convened healthcare leaders, clinicians, researchers, and patient advocates to explore strategies for improving outcomes and modernizing service delivery. Centers for Medicare & Medicaid Services (CMS) Administrator Dr. Mehmet Oz and senior CMS officials emphasized the agency’s evolving priorities under the Trump Administration, with a strong focus on digital transformation, patient empowerment, and fraud prevention.
In this article, Health Management Associates (HMA) experts highlight key themes from the conference. We note where these themes align with the agency’s recent proposed rules and requests for information (RFIs), including several RFIs included in the 2026 Medicare Physician Fee Schedule (PFS) proposed rule, with comments due September 12, 2025. Finally, they advise healthcare organizations of the immediate need to evaluate their risks and opportunities in this digital health ecosystem.
Key Themes of the Conference
Empower Patients with Data
CMS leaders shared a vision for enabling Medicare beneficiaries to experience healthcare technology in the same way that they use in banking and streaming services. Within a year, CMS committed to enabling real-time digital communication with beneficiaries, becoming the nation’s “best payer.” Notably, a patient safety advocate challenged CMS to think about bi-directional data exchange where patients should be able to share data with CMS.
Subsequent to the conference, Administration officials announced elements of the Health Technology Ecosystem infrastructure, including conversational AI tools, diabetes and obesity management platforms, and efforts to “kill the clipboard” by simplifying data access for patients and providers.
Reducing Waste and Tackling Fraud
The conference coincided with the federal government’s multi-billion dollar healthcare fraud takedown, underscoring CMS’ commitment to curbing waste. CMS officials highlighted several aspects of CMS’ work, including application of predictive algorithms dubbed “the Netflix model” to identify suspicious billing patterns. They also talked about the new CMS Innovation Center model—the Wasteful and Inappropriate Service Reduction (WISeR) Model—to engage technology companies to improve prior authorization processes in traditional Medicare, particularly for high-risk items like skin and tissue substitutes.
Focusing on Prevention
CMS tied the Make American Healthy Again (MAHA) agenda to quality measurement reform. CMS officials encouraged moving to two distinct sets of quality measures: one for treating illness and another for maintaining health. These measures could focus on preventing or delaying onset of disease and on measuring outcomes.
Moving to Digital Quality
CMS also emphasized its commitments to digital quality measurement and interoperability through the adoption of Fast Healthcare Interoperability Resources (FHIR®) application programming interface (API) technology. For example, CMS’ Center for Clinical Quality and Standards is testing a FHIR-based assessment tool for inpatient psychiatric hospitals. Separately, the Centers for Disease Control and Prevention (CDC) is transitioning National Healthcare Safety Network’s measures to FHIR.
Policy Connections: From Conference Themes to Federal Action
The conference themes reflect and preview broader federal policy changes including:
- The 2026 Medicare Physician Fee Schedule (PFS) proposed rule includes multiple requests for input on streamlining quality measures, enhancing chronic disease management, and expanding digital infrastructure.
- On July 30, CMS announced an updated voluntary blueprint for modern health data exchange, which encourages healthcare organizations to become CMS-aligned networks. The agency’s Interoperability Framework describes the voluntary criteria for CMS-aligned in areas of Patient Access & Empowerment, Provider Access & Delegation, Data Availability & Standards Compliance, Network Connectivity & Transparency, and Identity, Security & Trust.
The Road Ahead for Healthcare Organizations
Healthcare organizations need to prepare for a future regulatory environment that is significantly more digital, interoperable, and chronic disease–focused. CMS is building the highway that will enable healthcare organizations to build and maintain the technology necessary for these new initiatives.
This will require state and local government, healthcare organizations, and other partners to retool their infrastructure and workflows to optimize needed operational transformations. All entities should have a strategic roadmap for obtaining and using interoperable clinical data for care management, population health and quality, among other use cases.
Payers will benefit from initiatives such as:
- Exploring strategic partnerships to help accelerate technology advancement, such as digital identity providers and specialists in digital quality measurement
- Exploring ways to increase focus on prevention, such as increasing uptake of the Medicare Annual Wellness Visit or considering new payment approaches for services like medically tailored meals
- Staying current on AI tools and predictive analytics that identify individuals at risk for preventable conditions and working with their provider networks to intervene early
States can take steps to prepare, including:
- Exploring strategic partnerships to help accelerate technology advancement, such as digital identity providers and specialists in digital quality measurement
- Assessing the reach and impact of existing primary prevention programs to understand how they can use their levers to incentivize healthy lifestyles, encourage culturally responsive health education, and address root causes of preventable illness and disease
- Identifying opportunities for aligned efforts and referral pathways, including with community organizations, to address upstream health factors
Health systems and providers will need to reimagine the care experience by:
- Exploring early adoption of AI tools for medical documentation to improve both patient experience of care interactions and coding accuracy to support digital quality measurement
- Developing age-tailored checklists to ensure face-to-face time with patients to identify and support top primary prevention goals
- Evaluating and working with their patients to use digital tools that support chronic disease prevention, such as diabetes and obesity management platforms
Connect with Us
The CMS Quality Conference signaled a substantial shift toward streamlined regulatory approaches and expanded standard data exchange, digital quality reporting and measurement, and AI deployment in care settings and by payers. Stakeholders should anticipate additional federal guidance updates, including in the Medicare Physician Fee Schedule final rule in the fall.
HMA works with state agencies, payers, health systems, and providers to assess and implement digital health, quality systems, and information technology. We can help stakeholders develop cross-sector alliances, and organizations plan for and implement changes needed to react to these new initiatives. To discuss the implications of the Administration’s efforts in prevention, healthcare quality, and interoperability, contact our featured experts: Ryan Howells, Dr. David Polakoff, Sarah Hudson Scholle, and Maddy Shea.
Health Tech Ecosystem Leaders to Speak at HMA’s National Conference
The Trump Administration’s new Health Tech Ecosystem initiative is reshaping how patients and providers access health data, with the bold Kill the Clipboard road map offering a federal blueprint for modernization. At its National Conference being held October 14–16 in New Orleans, Health Management Associates (HMA) is bringing together healthcare leaders to explore how federal policy and industry innovation are driving smarter, more connected care.
About the Sessions
- Driving Digital Health Forward: Federal and Industry Enablers of Smarter, Connected Care
- The Digital Health “State of the Art”: Success Stories, Trends and Opportunities
- Seizing Disruption to Make a Lasting Impact in Healthcare
These and other sessions reflect the federal government’s evolving priorities around digital transformation, interoperability, and patient empowerment. The Health Tech Ecosystem initiative and CMS’s Interoperability Framework are setting new expectations for how healthcare organizations manage data, engage patients, and collaborate across sectors
Featured Digital Healthcare and Innovation Leaders Speaking at the HMA Conference
Our speakers will unpack the far-reaching impact of these advancements, spotlighting opportunities for smarter data exchange and care coordination in a connected ecosystem. In addition, experts from across the healthcare industry will share practical strategies for advancing digital maturity and overcoming operational challenges, with a focus on improving patient care and organizational efficiency.
- Secretary Bruce Greenstein, Louisiana Department of Health
- Jaime Bland, DNP, RN, Chief Executive Officer, CyncHealth
- Ryan Howells, Principal, Leavitt Partners (an HMA Company) and co-author of Kill the Clipboard
- Thomas Keane, MD, MBA, Assistant Secretary for Technology Policy and National Coordinator for Health IT, US Department of Health and Human Services
- Martin Lupinetti, President & Chief Executive Officer, HealthShare Exchange
- Juan Montanez, MBA, Managing Director, IT Advisory Services, HMA
- Curt Schatz, Vice President, Enterprise Clinical Enablement, Optum
- Chris Walker, Associate Vice President of Enterprise Transformation-Interoperability, Humana
Healthcare organizations need to prepare for a future regulatory environment that is significantly more digital, interoperable, and chronic disease–focused. From health plan executives and state Medicaid directors and policy teams, to provider organizations and health IT and digital health innovators, our speakers will discuss what changes are coming in the digital health space and how you can get your organization ready. Register for the conference today with the code HOTTOPIC25 to receive 20% off the standard conference rate through August.
HMA Roundup
Iowa
Iowa Names Lee Grossman New Medicaid Director. The Des Moines Register reported on July 31, 2025, that the Iowa Department of Health and Human Services has appointed Lee Grossman, former Wyoming Medicaid Director, to lead the state’s Medicaid program beginning in September. Grossman succeeds former Iowa Medicaid Director Liz Matney, who resigned November 1, 2024.
Michigan
Michigan Governor Urges Trump to Lengthen Transition Time for Medicaid Cuts. Iron Mountain Daily News reported on August 6, 2025, that Michigan Governor Gretchen Whitmer recently met with President Trump to discuss lengthening the transition period for some of the Medicaid cuts outlined in H.R. 1. The governor suggests a three-year period to allow the state to work with stakeholders and create a framework that would ensure stability of the Medicaid program. Whitmer also sought more flexibility and clarity on new changes made to the Insurance Provider Assessment and asked for more collaboration with the Centers for Medicare & Medicaid Services (CMS) to build a framework that ensures provider assessments meet the updated requirements.
Oregon
Oregon Announces $1.8 Million in Marketplace Coverage Enrollment Grants. The Oregon Health Authority announced on July 31, 2025, that it is awarding $1.8 million total to 37 community-based organizations and licensed insurance agents to help individuals navigate the Oregon Health Insurance Marketplace throughout the 2025-27 enrollment cycle. The awardees will offer free assistance in multiple languages to individuals enrolling in a Marketplace plan during the next enrollment period. Open enrollment will run from November 1, 2025, to January 15, 2026.
Oklahoma
Oklahoma to Submit SPA for Enhanced School-Based Medicaid Services. KGOU reported on July 31, 2025, that the Oklahoma Health Care Authority (OHCA) is preparing a Medicaid state plan amendment (SPA) that seeks to expand Medicaid-covered services in schools for eligible children. Oklahoma currently covers certain medically-necessary services, such as speech and hearing services, physical and occupational therapy, nursing, personal care, and behavioral health services provided to Medicaid-eligible children on Individualized Education Programs. The SPA seeks to extend this coverage to Medicaid-eligible children on other plans, including Individual Health Plans, 504 plans, and Behavioral Health Plans. It would also add additional behavioral health supports and medication administration to the services that schools could bill Medicaid for. OHCA intends to submit the SPA in November 2025, with implementation of enhanced services beginning March 2026.
National
Urban Hospitals Leverage Rural Designation Policy as H.R.1 $50B Fund Launches. Fierce Healthcare reported on August 4, 2025, that over 400 urban hospitals have obtained both urban and rural Medicare classifications since a 2016 regulatory shift, allowing them to access rural-specific reimbursement programs while retaining urban payment advantages, according to a Health Affairs study. These dual designations enable large nonprofit systems to qualify for rural support funds such as sole community hospital payments, 340B eligibility, and graduate medical education slots. This practice could affect the distribution of the $50 billion in new federal rural health funding authorized under H.R. 1.
Six Additional States Receive Federal Approval for SNAP Food Choice Waivers. The U.S. Department of Agriculture (USDA) announced on August 4, 2025, that West Virginia, Florida, Colorado, Louisiana, Oklahoma, and Texas have received federal approval for waivers allowing the states to ban certain foods from being covered by the Supplemental Nutrition Assistance Program (SNAP). Banned items include soda, candy, snack cakes, and other highly processed or low-nutritional-value products. The effort is part of President Trump’s “Make America Healthy Again” initiative, with 12 states now approved for food choice waivers that modify which items can be purchased with SNAP benefits.
Increased Medicaid Spending Did Not Boost Nursing Home Staffing, OIG Finds. Skilled Nursing News reported on August 4, 2025, that between 2018 and 2021, most nursing facilities increased the share of Medicaid reimbursement allocated to direct care compensation, yet many saw declines in nursing hours per resident day (HPRD), according to a new report from the U.S. Department of Health and Human Services (HHS) Office of Inspector General (OIG). The analysis found no consistent link between higher Medicaid spending and increased staffing, as funds often went to cover higher labor costs driven by retention bonuses, wage hikes, and reliance on contract labor during the COVID-19 public health emergency. Ownership structure played a key role, with nonprofit and government-owned facilities more likely to boost spending, while for-profits more often reduced both spending and HPRD.
Industry News
UnitedHealth Group Names Wayne DeVeydt CFO. Modern Healthcare reported on August 1, 2025, that UnitedHealth Group has named Wayne DeVeydt as chief financial officer, replacing John Rex. DeVeydt most recently served as managing director and operating partner at Bain Capital. Rex will become the strategic advisor to United’s chief executive Stephen Hemsley beginning September 2, 2025.
RFP Calendar
Actuaries Corner
HHS will Demo Drugmakers’ 340B Rebate Model in Limited Pilot Program. The Trump administration is accepting applications for a pilot program to demo rebates for 340B drugs, aiming to reduce abuse of the subsidy program by replacing traditional upfront discounts with post-purchase payments coordinated by drug manufacturers.
Discover other developments in the Wakely Wire here.
HMA News & Events
Leavitt Partners Webinar: Kill the Clipboard: What Does the CMS-Aligned Network Strategy Mean for the Future of Interoperability
NEW THIS WEEK ON HMA INFORMATION SERVICES
(Exclusive Access for HMAIS Subscribers):
HMAIS Medicaid Market Overviews, Reports, and Data
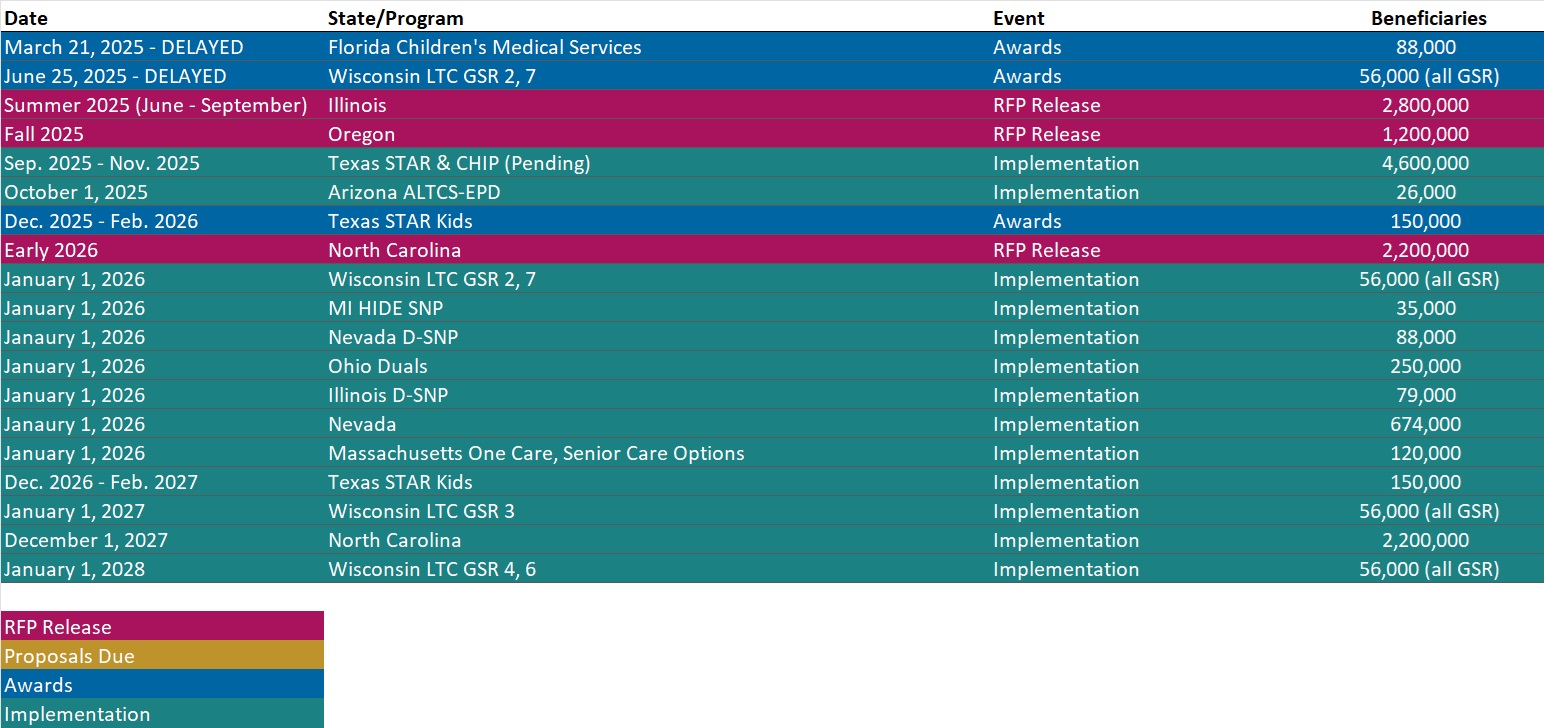
- Updated Medicaid Managed Care RFP Calendar
- Updated HMA Federal Health Policy Snapshot
- New Medicaid enrollment, RFP documents, and other market intelligence resources for dozens of states
- Updated Alaska Overview
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services.
If you’re interested in becoming an HMAIS subscriber, contact Andrea Maresca at [email protected].