This week, our In Focus section focuses on five critical policy and program trends to provide integrated care to dual-eligible individuals for Medicare and Medicaid. Both federal and state governments continue to look for ways to improve coordination and integration for this population. We anticipate the emphasis on innovative approaches to whole person, person-centered care, care management and coordination, care transitions, and regulatory oversight to persist. 2020 has been an active year of policymaking by the Centers for Medicare & Medicaid Services (CMS) and states. HMA distilled the themes and their strategic implications in this article. We continue to assist clients in tracking new policies and industry trends, developing innovative plans and strategies, and delivering high quality care and services to this population.
- The Federal government strengthened requirements for the integration of Medicare and Medicaid programs in State Medicaid Agency Contracts (SMACS). States increasingly use SMACs as a vehicle to promote state specific integration priorities for Medicare Advantage Dual Eligible Special Needs Plans (D-SNPs).
Synopsis: D-SNPs are required to have a SMAC in order to conduct business in a state. The SMAC must contain federally-required provisions including Medicare-Medicaid integration requirements that are described in a 2019 Final Rule[1] and further clarified in CMS guidance.[2] In addition to required components, more states are now using the SMAC process to add additional contract provisions to further state integration goals between Medicare and Medicaid for dual-eligible individuals. Notable provisions that states have included in their SMACs and other states may adopt include the following:
- Ensuring information sharing and transition of care follow up (TN)
- Requiring Highly Integrated D-SNPs (also known as HIDE SNP[3]) to share hospital and nursing home admissions data where it was not required by CMS (WA)
- Prohibiting D-SNPs from marketing to beneficiaries residing in geographies where Medicare-Medicaid plans (MMPs) offer capitated financial alignment demonstrations or dual demonstration programs (OH)
- Requiring Medicare default enrollment[4] for D-SNPs that also contract with the state for their Medicaid managed long-term services and supports program (AZ, NY)
- Requiring D-SNPs to offer at least one supplemental benefit that is complementary to benefits offered in the Medicaid program (UT)
Implications: D-SNPs should review their current SMAC to ensure compliance with the existing requirements. Existing and new D-SNPs should anticipate the creation of 2022 SMACs, evaluate organizational integration strategies, review industry best practices and determine whether there are provisions that enable D-SNPs to further state integration goals. HMA continues to monitor innovations in various states. HMA Information Services (HMAIS) maintains a current library of select SMACs and is available to subscribers.
- Congress and CMS have granted new flexibilities under four different authorities for Medicare Advantage plans, including D-SNPs, to offer innovative supplemental benefits. Dual eligible individuals have higher rates of chronic illness and other social risk factors and may benefit from these additional flexibilities.
Synopsis: Congress and CMS have recently expanded the definition of supplemental benefit policies to grant Medicare Advantage (MA) plans more flexibility than ever before to design and target these benefits. These include: 1) expansion of the definition of “primarily health-related;” 2) the ability to target benefits to certain sub-populations only (i.e., offer them non-uniformly); 3) implementation of the value-based insurance design (VBID) demonstration; and 4) establishment of special supplemental benefits for the chronically ill (SSBCI).[5] While all four benefit flexibilities allow greater tailoring of benefits to the needs of the population, SSBCI is the only type of supplemental benefit that allows the inclusion of non-medical benefits.
2020 was the first year that health plans could offer SSBCI, permitting supplemental benefits that are “non-primarily health-related” for individuals with one or more of 15 designated chronic conditions.[6] This flexibility enables plans to offer supplemental benefits that are intended to address social needs, such as non-medical transportations and home modifications. Sixty percent of dual eligible individuals have multiple chronic conditions[7] and other social risk factors and may benefit from non-primarily health-related services. Only six percent or approximately 1.4 million individuals are enrolled in plans offering SSBCI in 2020. One-third of plans offering SSBCI are SNPs, most of which are dual eligible SNPs (D-SNP).[8] HMA continues to track the landscape and adoption of supplemental benefits.
Implications: As part of the product planning and development cycle for 2022, D-SNPs may be considering adding expanded supplemental benefits to fill a need in for its members and attract prospective members. We anticipate the availability of these benefits to evolve over time, especially if Medicare beneficiaries gravitate to MA plans offering these benefits and they demonstrate increased quality and lower health care costs. D-SNPs and traditional Medicare Advantage plans should review benefits offered in current and potential markets while developing its supplemental benefit designs for 2022.
- In addition to the Medicare Advantage flexibilities to address social determinates of health (SDOH) described above, states are increasingly requesting respondents to Medicaid requests for proposal including dual-eligible individuals to address SDOH needs in their responses, particularly as needs of dual eligible individuals have been amplified by the COVID pandemic.
Synopsis: The impact of Social Determinates of Health on dual-eligible individuals has been a concern for Federal and State officials prior to the pandemic and data released by CMS showed that dual-eligible individuals are even more susceptible to poor health and death during a public health crisis/pandemic. The data showed that dual-eligible individuals are more likely to contract and be hospitalized for COVID-19 than Medicare-only individuals and that dual-eligible individuals are hospitalized with COVID-19 complications at a rate of more than four times higher than Medicare-only individuals. [9] HMA has observed an increase in States’ focus on responders addressing SDOH needs of dual-eligible individuals in its Medicaid managed care requests for proposals, e.g., coordinating with employment programs, addressing food insecurity, and other SDOH. Managed Care Organizations (MCOs) expecting a state Medicaid procurement or re-procurement including dual-eligible individuals will want to prepare for the increased scrutiny in this area by having available data supporting their efforts to address SDOH and/or implement programs targeting SDOH. This may include developing relationships with community based organizations that specialize in meeting SDOH needs such as housing agencies and home delivered meals providers and vendors that offer services like pest control.
Implications: In developing benefits or services to address SDOH of members, in addition to its usual product development work, health plan should review State’s Managed Long-Term Services and Supports (MLTSS) program services effectiveness to deliver complementary and enhanced benefits to those benefits offered by Medicaid.
- CMS will not grant contracts to new D-SNP look-alike plans in 2022 and will not renew D-SNP look-alike plans in states with MMPs and/or D-SNPs for 2023.
Synopsis: D-SNP look-alike plans are traditional Medicare Advantage plans that are designed to attract dual-eligible individuals through coverage of supplemental benefits such as dental, vision, and hearing services and generous value-added benefits such as over the counter cards. This type of plan circumvents the requirement of having a State Medicaid Agency Contract (SMAC) to coordinate and integrate benefits and care between Medicare and Medicaid, among other D-SNP statutory and regulatory requirements. The criteria for identifying a D-SNP look-alike plan is the percentage of dual-eligible individuals enrolled in the plan. If dual-eligible individuals comprise 80 percent of more of the plan enrollment, it is considered a D-SNP look-alike plan.
D-SNP look-alike plans were often created by health plans that wanted to serve their dual-eligible membership but were not contracted to participate in a State’s MMP or Medicaid managed care programs and could not receive a SMAC from the State. D-SNP look-alike plans have grown across the country but are especially focused in California, Florida and New York, as some of these states prohibit D-SNPs in areas where Medicare-Medicaid Plans are offered or are unwilling to sign SMACs for organizations that do not participate in the state’s Medicaid managed care program.
Implication: There is no explicit CMS approved process to transfer members from D-SNP look-alike plans to other plan options so strategic planning is important. Health plans should determine if any of their products qualify as a D-SNP look-alike plans. If a health plan with a D-SNP look-alike plan is offering a D-SNP or MMP in the same service, evaluate why those plan options are not attracting membership and modify the product offering. Those organizations with a D-SNP look-alike product without a D-SNP or MMP should look to create a D-SNP.
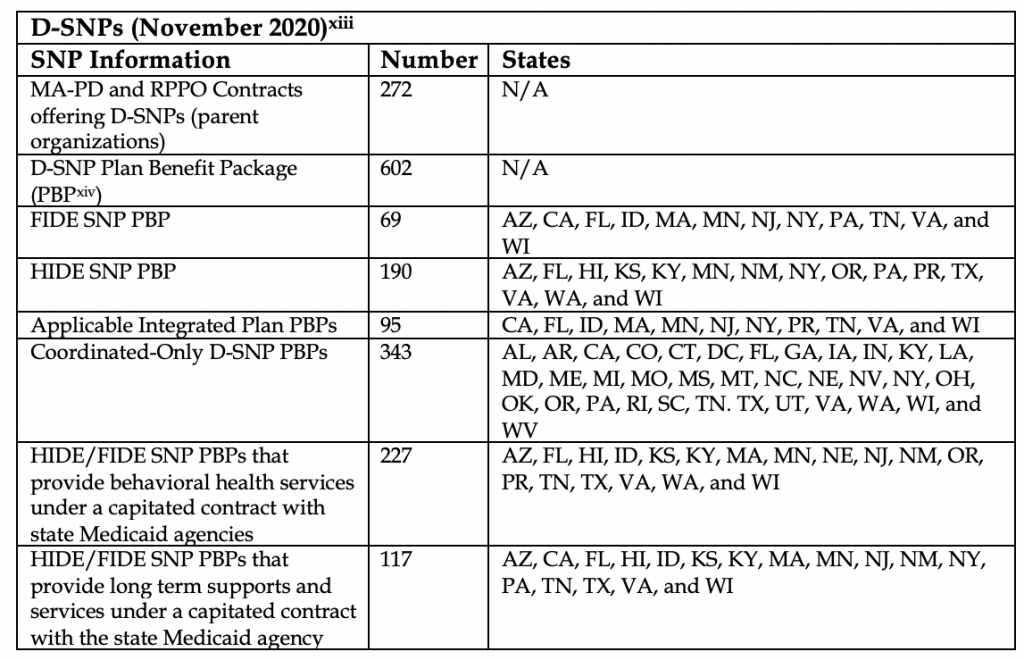
- CMS recently released data on the multiple categories of D-SNPs highlighting the varying levels of integration, different D-SNP types and where they operate. This information provides plans with important insights for 2022 and 2023 business and strategic planning.
Synopsis: The table below outlines the Medicare Medicaid Coordination Office’s finding upon completing their review of the 2021 SMACs, which included new mandated requirements for integration. D-SNPs are now categorized by FIDE, HIDE, Coordinated-Only D-SNPs and Applicable Integrated Plans. This categorization, which is described in a 2019 Final Rule[10] and further clarified in the CMS guidance[11], provides insight into whether and the extent to which states include in their SMAC nursing facility care, behavioral health benefits and/or long term services and supports, and whether the level of benefits meets the Highly Integrated Dual Eligible (HIDE) SNP or the Fully Integrated Dual Eligible (FIDE[12]) SNP designations. States may allow multiple types of D-SNPs to operate or limit to a certain type of D-SNP (e.g. HIDE SNP or FIDE SNP) to do business in the state. HMA is examining this data in conjunction with our available CMS county level data to support D-SNP targeted market strategies.
Implication: The newly available aggregate information supports planning for MA organizations currently operating or interested in applying for a D-SNP and for entities considering launching a D-SNP in a new state.
Next Steps
HMA continues to analyze Medicare Advantage and Medicaid policies and practices for dual-eligible individuals. For more information or questions about this update or D-SNP related polices, please contact Julie Faulhaber, Mary Hsieh, or Sarah Barth.
[1] CMS-4185-F, the “Medicare and Medicaid Programs; Policy and Technical Changes to the Medicare Advantage, Medicare Prescription Drug Benefit, Programs of All-Inclusive Care for the Elderly (PACE), Medicaid Fee-For-Service, and Medicaid Managed Care Programs for Years 2020 and 2021” final rule. Retrieved from https://www.govinfo.gov/content/pkg/FR-2019-04-16/pdf/2019-06822.pdf.
[2]Sharon Donovan, Dual Eligible Special Needs Plans, “Additional Guidance on CY2021 Medicare-Medicaid Integration Requirements for Dual Eligible Special Needs Plans (D-SNPs)”, memorandum, January 17,2020, Program Alignment Group. Retrieved from https://www.cms.gov/files/document/cy2021dsnpsmedicaremedicaidintegrationrequirements.pdf
[3]A D-SNP may meet the criteria for designation as a HIDE SNP if it covers, consistent with state policy, either (1) LTSS or (2) Medicaid behavioral health services, under a state contract either directly with the legal entity providing the D-SNP, with the parent organization of the D-SNP, or with a subsidiary owned and controlled by the parent organization of the D-SNP.” Sharon Donovan, Dual Eligible Special Needs Plans, “Additional Guidance on CY2021 Medicare-Medicaid Integration Requirements for Dual Eligible Special Needs Plans (D-SNPs)”, memorandum, January 17, 2020, Program Alignment Group. Retrieved from https://www.cms.gov/files/document/cy2021dsnpsmedicaremedicaidintegrationrequirements.pdf
[4] Enrollments of an organization’s Medicaid managed care enrollees into an affiliated dual eligible special needs plan (D-SNP) upon the individuals’ initial eligibility for Medicare.
[5] Narda Ipakchi, Jonathan Blum, Eric Hammelman and Mary Hsieh, “Medicare Advantage Supplemental Benefit Flexibilities: Adoption of an Access to Newly Expanded Supplemental Benefits in 2020”, May 2020. Retrieved from https://www.healthmanagement.com/wp-content/uploads/Medicare_Advantage_Supplemental_Benefit_Flexibilities_Issue_Brief_2-27-20_HMA.pdf
[6] Qualifying chronic conditions include: chronic alcohol and other dependence, autoimmune disorders, cancer (excluding pre-cancer conditions), cardiovascular disorders, chronic heart failure, dementia, diabetes mellitus, end-stage liver disease, End-Stage Renal Disease (ESRD) requiring dialysis, severe hematologic disorders, HIV/AIDS, chronic lung disorders, chronic and disabling mental health conditions, neurologic disorders, stroke.
[7] Medicare-Medicaid Coordination Office, “People Dually Eligible for Medicare and Medicaid”, Fact Sheet, March 2020, Centers for Medicare & Medicaid Services. Retrieved from https://www.cms.gov/Medicare-Medicaid-Coordination/Medicare-and-Medicaid- Coordination/Medicare-Medicaid-Coordination-Office/Downloads/MMCO_Factsheet.pdf
[8] Narda Ipakchi, Jonathan Blum, Eric Hammelman and Mary Hsieh, “Medicare Advantage Supplemental Benefit Flexibilities: Adoption of an Access to Newly Expanded Supplemental Benefits in 2020”, May 2020. Retrieved from https://www.healthmanagement.com/wp-content/uploads/Medicare_Advantage_Supplemental_Benefit_Flexibilities_Issue_Brief_2-27-20_HMA.pdf
[9] Seema Verma, ‘Medicare COVID-19 Data Release Blog”, blog post, June 22,2020. Centers for Medicare & Medicaid Services. Retrieved from https://www.cms.gov/blog/medicare-covid-19-data-release-blog#_ftn2
[10] CMS-4185-F, the “Medicare and Medicaid Programs; Policy and Technical Changes to the Medicare Advantage, Medicare Prescription Drug Benefit, Programs of All-Inclusive Care for the Elderly (PACE), Medicaid Fee-For-Service, and Medicaid Managed Care Programs for Years 2020 and 2021” final rule. Retrieved from https://www.govinfo.gov/content/pkg/FR-2019-04-16/pdf/2019-06822.pdf
[11] Sharon Donovan, Dual Eligible Special Needs Plans, “Additional Guidance on CY2021 Medicare-Medicaid Integration Requirements for Dual Eligible Special Needs Plans (D-SNPs)”, memorandum, January 17,2020, Program Alignment Group. Retrieved from https://www.cms.gov/files/document/cy2021dsnpsmedicaremedicaidintegrationrequirements.pdf
[12] A FIDE SNP is offered by the legal entity that also has a state contract as a Medicaid managed care organization (MCO) to provide Medicaid benefits, including long-term services and supports (LTSS) and behavioral health benefits, consistent with state policy. Sharon Donovan, Dual Eligible Special Needs Plans, “CY2021 Medicare-Medicaid Integration and Unified Appeals and Grievance Requirements for Dual Eligible Special Needs Plans (D-SNPs)”, memorandum, October 7, 2019, Program Alignment Group. Retrieved from https://www.cms.gov/Medicare-Medicaid-Coordination/Medicare-and-Medicaid-Coordination/Medicare-Medicaid-Coordination-Office/Downloads/DSNPsIntegrationUnifiedAppealsGrievancesMemorandumCY202110072019.pdf
[13] Sharon Donovan, Dual Eligible Special Needs Plans, “Results from the CY2021 State Medicaid Agency Contract (SMAC) Review and Release of the Dual Eligible Special Needs Plan (D-SNP) Management Module in the Health Plan Management System (HPMS)”, memorandum, November 24, 2020, Program Alignment Group. Retrieved from https://www.cms.gov/Medicare-Medicaid-Coordination/Medicare-and-Medicaid-Coordination/Medicare-Medicaid-Coordination-Office/D-SNPs
[14] A set of benefits for a defined Medicare Advantage service area.