This week, our In Focus section reviews the finalized coverage expansions for Medicare telehealth services in the Centers for Medicare & Medicaid Services (CMS) Calendar Year (CY) 2021 Physician Fee Schedule (PFS) Final Rule. Telehealth advocates will be pleased to see meaningful expansions; however, the response of advocates will also be tempered by the impending return of the geographic and site of service limitations that will follow at the conclusion of the COVID-19 Public Health Emergency (PHE). During the PHE, millions of patients and providers increased their use of telehealth services to expand access to care. Given this shift in the delivery of care, telehealth advocates had been hopeful CMS would make extensive permanent coverage expansions in the Medicare program. In light of this, CMS’s new regulation will come as a reminder to many that the key to long term expansions of Medicare telehealth coverage lies in the hands of the U.S. Congress.
Published on December 1, 2020, CMS’s CY 2021 PFS Final Rule expands coverage of Medicare telehealth services in several ways. The regulation finalizes policy which will result in Medicare covering 251 types of telehealth services as of January 1, 2021. These services fall into three groups, based on when Medicare coverage of these services is due to expire.
- First, CMS added several services permanently to its Medicare telehealth services list (Group A in the table below). This group represents 45 percent of the telehealth services (112 services) that will be covered by CMS on January 1 and includes services such as standard evaluation and management visits, group psychotherapy, neurobehavioral status exams, and short home visits. The majority of Medicare telehealth visit volume that is likely to occur will be in this group.
- Second, CMS will cover many services conducted via telehealth on a temporary basis until December 31, 2021 (Group B). This group represents 23 percent (57 services) of all telehealth services covered on January 1 and includes services such as emergency department visits (all levels), physical therapy, occupational therapy, and speech pathology. CMS’s rationale for covering these services on a temporary basis is to gather data to assess if these services should be covered on a permanent basis starting in 2022.
- Third, CMS will cover a large group of telehealth services only until the PHE expires (Group C). This group represents 33 percent (82 services) of all telehealth services covered on January 1 and includes services such as audio-only telehealth visit codes, initial hospital and nursing home visits, and home visits for new patients. Coverage for this group of services will end with the expiration of the PHE (currently set at to January 20, 2021 (HHS). The extension of the PHE for an additional 90 days beyond January 20, 2021 seems likely given the increase in COVID-19 cases observed in recent weeks.
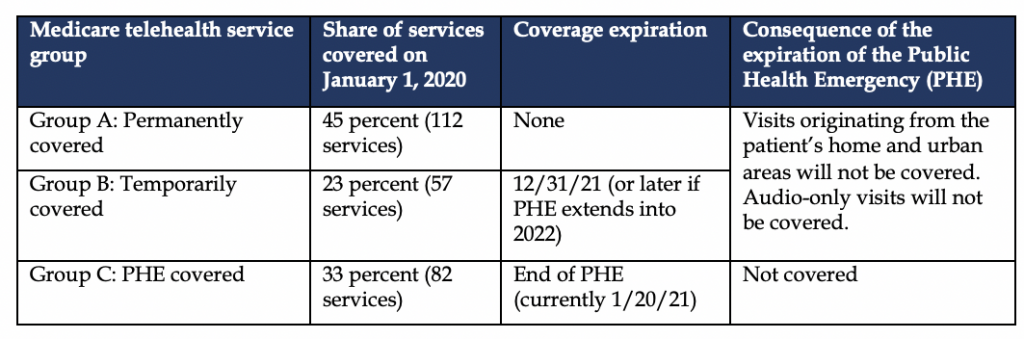
While Medicare telehealth service Group C will cease to be covered after the PHE expires, the expiration of the PHE will have other critical implications for service Groups A and B. For services in Groups A and B the expiration of the PHE will end the ability of providers and patients to conduct all of these services via audio-only communication, from the patient’s residence, and from locations in urban areas. These three Medicare telehealth limitations are written into statute at section 1834(m) of the Social Security Act, and CMS lacks the statutory authority to modify them. It was only through its waiver authority under section 1135 of the Social Security Act that CMS could temporarily remove these limitations during the PHE. Therefore, removing these three limitations to Medicare telehealth coverage requires Congress to pass legislation modifying section 1834(m) of the Social Security Act.
CMS also finalized in its recent regulation coverage enhancements for other Medicare virtual care services, such as remote patient monitoring (RPM) in patients’ homes and quick clinical visits described as communications technology-based services (CTBS). While neither of these services are bound by the limitations of section 1834(m) discussed above, CMS’s policy changes are expected to remove some of the barriers providers face in offering RPM and CTBSs to their patients. For RPM services, CMS will permit patient consent to be obtained at the time of service delivery and will permit auxiliary clinical personnel to provide RPM services. For CTBSs, CMS created a new billing code (G2252) for longer audio-only visits and will expand the types of clinicians eligible to bill CTBSs (e.g., physical and occupational therapists, and licensed clinical social workers).
Finally, CMS finalized policies which will increase opportunities to use telehealth services in the context of physician incident-to billing and in nursing facilities. For 2021, CMS enabled physicians to provide direct supervision of other clinical staff if they are immediately available to engage via interactive audio-video. In addition, CMS reduced the frequency limit for coverage of subsequent nursing facility care services furnished via telehealth from once every 30 days to once every 14 days.
Collectively, CMS’s recent telehealth policy decisions are likely to increase the use of telehealth services within the Medicare program. However, the extent of this increase is heavily dependent upon the date of which the PHE expires. After the PHE ends, some forms of telehealth service use are likely to recede unless Congress acts to modify section 1834(m) of the Social Security Act. Telehealth advocates are likely to be pleased by the potential service use increase, but will also be frustrated by the potential loss of audio-only services, visits from patients’ homes, and visits from urban areas when the PHE expires. The instability of Medicare’s coverage of telehealth services may create significant barriers to the adoption and use of telehealth services, particularly in urban areas. While CMS will continue to play a central role in future expansion of Medicare telehealth coverage, the U.S. Congress largely holds the key to expanding Medicare telehealth coverage at this time.
HMA continues to analyze the CY 2021 PFS Final Rule. For more information or questions about the Final Rule, telehealth services, or other Medicare physician policies please contact our experts below.

