This week, our In Focus section reviews the District of Columbia (DC) Medicaid managed care request for proposals (RFP), released on November 19, 2021, by the District of Columbia Department of Health Care Finance. The procurement will cover DC Healthy Families Program (DCHFP), including adults with special health care needs; District of Columbia Healthcare Alliance Program (Alliance); and Immigrant Children’s Program (ICP). DC expects to award contracts to up to three managed care organizations (MCOs), covering physical, behavioral health, and pharmacy services. Contract approval is expected by June 2022 and implementation in October 2022.
Background
DC awarded contracts last year to AmeriHealth Caritas, CareFirst BlueCross BlueShield Community Health Plan (formerly known as Trusted Health Plan), and MedStar Family Choice. Incumbent plan, Anthem/Amerigroup, challenged the decision after failing to secure a contract. As a result, a DC Contract Appeals Board judge ordered the District to reassess its Medicaid managed care contracts after finding procurement law violations. A chief administrative judge concurred the decision. The ruling allowed DC to extend the exisiting contracts to allow beneficiaries to stay on their current plans. The judge found MedStar should have scored lower under the law because it did not include information about its leadership and submitted performance evaluations pertaining to two previous contracts instead of three.
Mayor Muriel Bowser declared a state of emergency to extend the MedStar Family Choice contract for nine months to avoid coverage disruptions, however the Council of the District of Columbia (DC’s legislative body) delayed the proposed Medicaid contract extension. MedStar also previously announced that it may no longer allow other Medicaid plan members in DC to access the organization’s network of primary care providers and specialists.
Prior procurements also failed to treat all bidders equally, resulting in rebids over the course of a few years.
In October 2021, chief procurement officer George Schutter, testified that the District of Columbia will increase oversight and the monitoring of Medicaid managed care procurements. Schutter noted that DC has selected a contracting officer and had convened an integrated procurement team that meets weekly.
RFP
The new RFP will cover the traditional Medicaid population through DCHFP; individuals not eligible for Medicaid who are over the age of 21 with an income up to 200 percent of the federal poverty level through Alliance; and immigrant children under the age of 21 with a household income under 300 percent FPL through ICP. In fiscal year 2021, DC transitioned adults with special health care needs, formerly enrolled in the Medicaid fee-for-service program, into the DCHFP. MCOs will focus on achieving better health outcomes, health care innovation, and cost-effective quality healthcare. They must offer a range of preventive, primary care, specialty services, and long-term services and supports. In 2023, MCOs must also cover mental health services and substance use disorder services through the District’s Medicaid waiver amendments and state plan amendments. While the RFP states it would begin April 2023, an updated timeline from the District now shows the carve-in will be effective October 2023.
The resulting contracts from the RFP will run for five years, with the option to extend the term for an additional five-year period (not to exceed ten years). The five-year base term is worth $2.8 billion. MCOs that submit proposals must include a subcontracting plan worth 7 percent of the five-year base term. Any proposals without the plan will be rejected.
Evaluation
MCOs can earn a total of 112 points. Technical proposals will be scored out of a maximum 90 points and consist of three parts:
- Technical Approach and Methodology (30 Points)
- Provider network (10 points)
- Services and supports (including value-added benefits) to address social factors (10 points)
- Integrating behavioral health and managing services for substance use disorders (10 points)
- Technical Expertise (40 Points)
- Claims processing, adjudication, and auditing (10 points)
- Case management and care coordination (15 points)
- Access and utilization of perinatal visits and birth outcomes (15 points)
- Past Performance (20 Points)
- Past experience providing managed care services; organizational history, past and current operational experience
MCO’s prices will be scored out of 10 points. The lowest price will receive the maximum points.
An additional 12 points can be earned as “preference points” for MCOs that are certified by the Department of Small and Local Business Development.
Timeline
The RFP was released on November 19, 2021, with proposals due December 20. Although not mentioned in the RFP, according to testimony from chief procurement officer George Schutter, awards are expected by June 2022 and implementation in October 2022.
Current Market
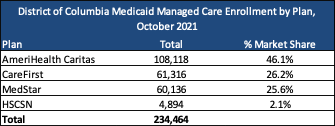
As of October 2021, the District has over 234,000 Medicaid managed care enrollees. An additional 51,182 individuals in the District are enrolled in Medicaid fee-for-service. The District’s goal is to move beneficiaries to managed care in the near future. AmeriHealth Caritas has the most beneficiaries, representing 46 percent of DC’s Medicaid managed care population. There were also 21,916 beneficiaries under Alliance and 4,207 under ICP.