This week, our In Focus reviews the Mississippi request for qualifications (RFQ) for the state’s traditional Mississippi Coordinated Access Network (MississippiCAN) Medicaid program and the state Children’s Health Insurance Program (CHIP). The RFQ, released by the Mississippi Division of Medicaid on December 10, 2021, seeks two to three health plans to serve roughly 480,000 individuals. This is the first time the state is seeking plans, which it refers to as Coordinated Care Organizations (CCOs), to jointly administer MississippiCAN and CHIP.
RFQ
MississippiCAN and CHIP operate in all 82 counties of the state. Winning plans will be required serve eligible MississippiCAN and CHIP members statewide. The programs cover the populations shown in the tables below. Optional populations can voluntarily enroll in MississippiCan. If these members then choose to disenroll, they are moved to the state’s Medicaid fee-for-service program.
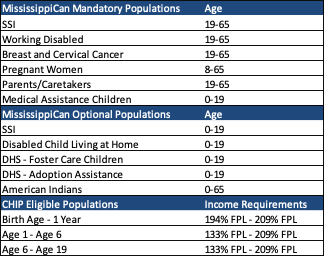
Covered services in MississippiCan include inpatient/outpatient emergency services, post-stabilization care services, EPSDT services, behavioral health/substance use disorder services, and foster care services.
Covered services in CHIP include inpatient/outpatient emergency services, post-stabilization care services, Well-Baby/Well-Child Services/Immunization Services, behavioral health/substance use disorder services, dental services, and vision services.
The Mississippi Division of Medicaid will contract with a Pharmacy Benefits Administrator (PBA) for management and payment of pharmacy claims, prior authorizations, and management of the pharmacy network for all Mississippi Medicaid, MississippiCAN, and CHIP populations.
New RFQ Provisions
CCOs will be required to develop care management partnerships with local organizations to address health equity and social determinants of health. Care management requirements were expanded to require closed-loop referrals, warm handoffs, and standardized assignment of risk levels.
CCOs will also be newly required to employ a Perinatal Health Director and a Behavioral Health Director.
Timeline
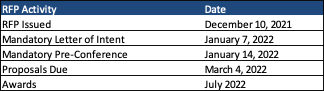
A mandatory letter of intent must be submitted on January 7, 2022, with a mandatory pre-qualification conference to be held on January 14th. Qualifications are due March 4th and awards are expected July 2022. The contracts will have an initial four-year term with two one-year renewal options.
Current Market
MississippiCan had 420,455 members as of November 2021, served by incumbent plans Centene/Magnolia Health Plan, Molina Healthcare, and UnitedHealthcare.
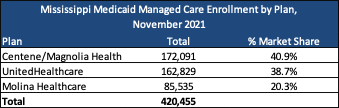
CHIP is currently served by Centene/Magnolia Health Plan and UnitedHealthcare, with a total of 42,609 members between the two plans.
Evaluation
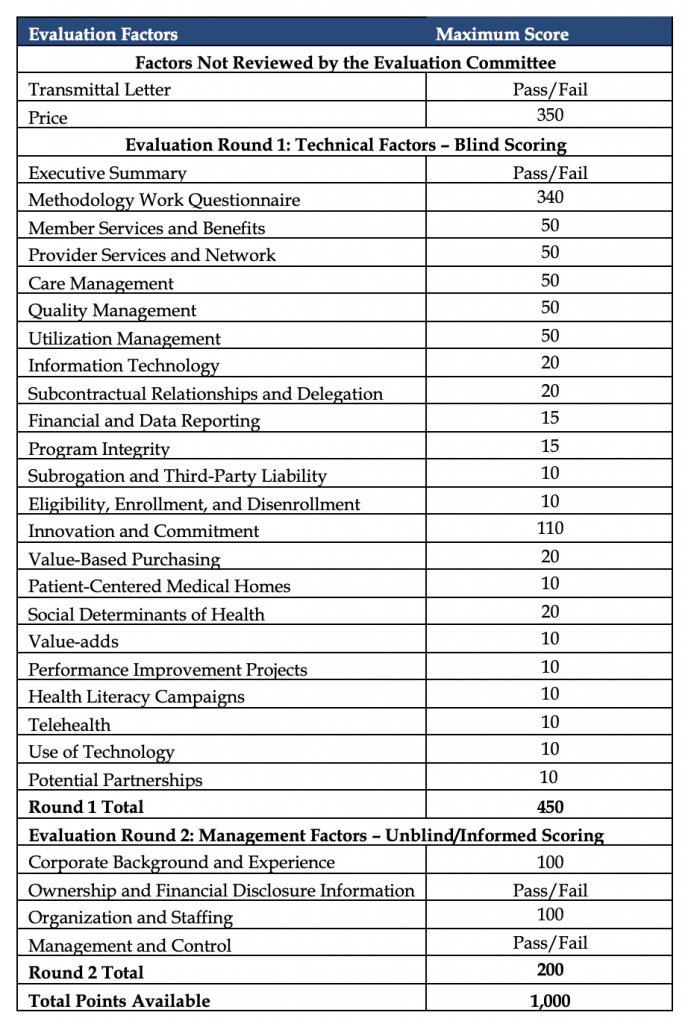
Evaluation of qualifications will be conducted in three stages, totaling a maximum of 1,000 points. In the first stage, each qualification is reviewed for responsiveness/completeness. In the second stage, qualifications are reviewed for meeting RFQ requirements. Finally, in the third stage, qualifications are scored based on price, technical factors, and management factors shown in the table below.