This week’s In Focus is the second in a two-part look at the Centers for Medicare & Medicaid Services’ (CMS’s) recently proposed changes to the Medicaid program. Last week we covered CMS’s proposed changes to the federal Medicaid managed care regulations (CMS-2439-P). This week we review the Medicaid Access to Care proposed rule (CMS-2442-P).
As we discussed last week, the managed care and access to care rules include significant changes to core structural and financing aspects of the Medicaid program. Though state agencies, providers, health plans, consumer groups, and other stakeholders will want to understand the distinct requirements and expectations in each rule that apply to them, the proposed changes cannot be viewed in isolation.
The Access to Care rule addresses a range of challenges that shape the experience of Medicaid enrollees, regardless of whether they are in managed care programs or traditional fee-for-service (FFS). The proposed policy changes also are designed to create an updated federal framework for Medicaid’s home and community-based services (HCBS) programs. These proposals come at a pivotal time, as states are facing workforce shortages, particularly among HCBS direct care workers (DCWs).
The remainder of this In Focus delves into notable components of the proposed changes and includes analysis of the implications of these policies for stakeholders. CMS will benefit from stakeholder input; the deadline for submitting comments is July 3, 2023.
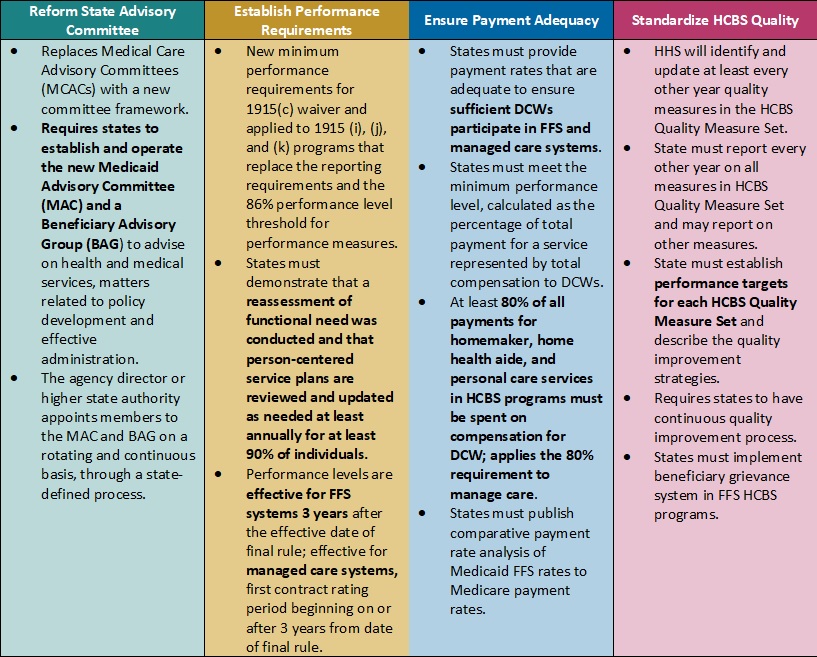
Table 1. Access to Care Regulations: Overview of Proposed Changes
Key Themes and Considerations
Ensuring Payment Adequacy for Key HCBS Services Experiencing Workforce Shortages. One of the most notable proposed changes that would directly impact DCWs is a requirement that at least 80 percent of Medicaid payments be spent on compensation. The proposed rule would apply to homemaker, home health aide, and personal care services, as they represent a large portion of HCBS services that DCWs provide. The proposal is based on feedback from states that have implemented similar provisions, which have ranged from 75 to 90 percent compensation requirements.
CMS specifically seeks stakeholder feedback on the percentage that should be adopted. This policy provision also is important from an equity perspective, given that 90 percent of DCWs are women and 60 percent are members of racial or ethnic minority populations. However, increased or mandated DCW rates may make it difficult for HCBS providers to sustain their businesses as they manage the increased administrative pressures of electronic visit verification, the complexity of filing claims for managed long-term services and supports (MLTSS), and the additional work that HCBS quality measurement may create. Smaller HCBS providers, some of which may have deep cultural expertise, may struggle to sustain themselves and meet these requirements.
Table 2. Access to Care Regulations: Snapshot of Proposed Rate, Access, and Payment Changes
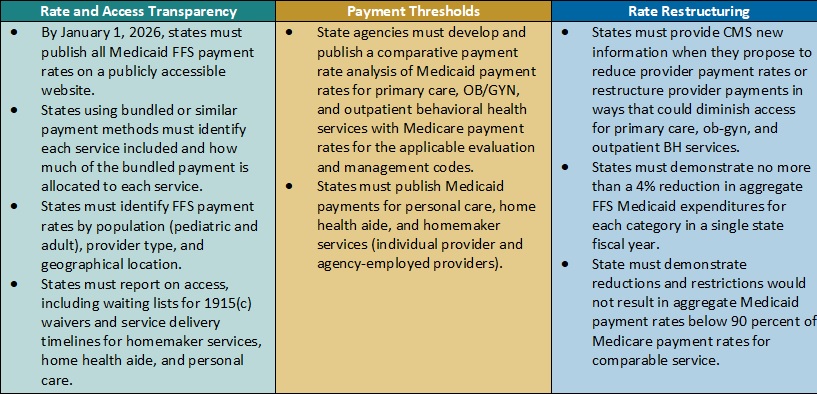
Payment Alignment. CMS is seeking to align access to care strategies and payment rate transparency more closely across the FFS and managed care delivery systems. The proposed rule includes several changes that CMS has developed achieve this goal. For example:
- CMS plans to require that states publish more detailed rate information in a consistent format. States, health plans, providers, and other interested stakeholders will want to consider the implications by delivery system. Additional transparency requirements could create a new opportunity to understand rates across payers and states and use this information in addressing access challenges for services.
- The proposed rule also would require extensive comparative analysis of Medicaid FFS rates and Medicare rates. CMS proposes to use Medicare non-facility payment rates as a benchmark to determine if states are meeting federal Medicaid access State analyses will be vital to CMS oversight as well as advocacy efforts within states to monitor and update FFS rates as needed.
Strengthening the Focus on Quality in State HCBS Programs. Over the last several decades, states and Medicaid stakeholders have made significant progress toward increasing participation in HCBS programs and community integration initiatives to counter Medicaid’s institutional bias. CMS is proposing more consistency in the expectations and reporting for HCBS quality measures to further the impact and create a consistent foundation for the recently mandated HCBS quality initiatives starting to take root.
In the short-term, the proposed changes will require states, and likely downstream providers and Medicaid agencies, to immediately change their quality reporting policies and systems. States and their stakeholders will want to map out processes for cyclical updates to HCBS quality measures, including cross-walking the future measures with existing ones, making systems changes, and updating dashboards. Targeted attention and focus will be needed to identify realistic HCBS performance targets that yield successful improvement strategies in the midst of a workforce crisis. Longer term, it will be necessary to map out when updates and reporting will be required to strengthen the rigor and accountability for state performance in the HCBS quality measure set, as well as reinforce the information available to make policy, clinical, and operational improvements to Medicaid programs.
HCBS Access Measurement. CMS is proposing new FFS HCBS payment and access transparency requirements to ensure compliance with Medicaid provider payment rules that require payments to be adequate to enlist at least the same number of providers that the overall geographic population can access. Because the targeted HCBS services do not have a comparable Medicare rate, CMS proposes implementation of a payment rate disclosure approach that would standardize data and monitoring across service delivery systems, with the goal of improving access. In addition to proposed payment transparency changes, CMS proposed new reporting on HCBS waiver waiting lists and timelines for the start of related services once authorized.
These new reporting requirements will provide stakeholders with more information to benchmark their state’s experience with other providers across the nation. This information could be influential to policymakers and legislators and help uncover some of the core contributors to our nation’s HCBS workforce shortage.
Improving Health Equity with Medicaid Beneficiary Input. CMS proposes overhauling the scope and membership of the state Medical Care Advisory Committee. The new Medicaid Advisory Committee (MAC) would continue to advise the state on health and medical matters and play an expanded advisory role on matters of policy development and effective administration of the program. CMS also plans to require that states establish a Beneficiary Advisory Group (BAG) composed of current or past Medicaid beneficiaries. A subset of BAG members would serve on the MAC to ensure their perspectives are integrated into the committee’s recommendations to states.
Under the new federal requirements, MAC representatives could have greater relative input and influence on policies and actions each state Medicaid agency advances. Medicaid stakeholders will want to ensure the MAC’s minimum federal requirements support effective structures and processes in states.
What’s Next
CMS plans to reframe Medicaid access as one of three parts of the continuum of care, along with enrollment and maintenance of coverage. The proposals in the Access to Care rule would have a meaningful impact on the volume and type of data available to evaluate the relationship between Medicaid payment rates and access across all delivery systems.
States, managed care organizations, providers, Medicaid enrollee advocacy organizations, and other interested stakeholders should analyze the proposals and consider submitting comments to CMS on the feasibility, potential impact, and, where applicable, alternatives to the proposed changes. They also can use this time to begin planning and determine which resources and tools they may need to prepare for implementation of changes across delivery systems in the Medicaid program.
HMA’s experts are taking a wholistic approach to reviewing the Access to Care and Managed Care proposed rules in tandem and identifying key points of intersection.
For more information on the access to care proposed rule, contact HMA’s team of experts, Susan McGeehan and Andrea Maresca.

