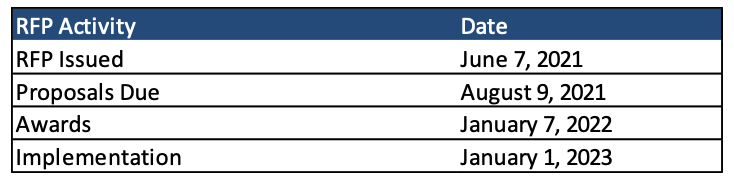
This week, our In Focus section reviews the Indiana Medicaid managed care request for proposals (RFP) for health plans serving beneficiaries enrolled in Hoosier Healthwise and Healthy Indiana Plan (HIP) programs. Contracts will be worth over $6 billion annually. The RFP was released on June 7, 2021, by the Indiana Department of Administration on behalf of the Family and Social Services Administration Office of Medicaid Policy and Planning.
Background
Hoosier Healthwise is Indiana’s traditional Medicaid program that covers pregnant woman, children (including those enrolled in CHIP), and some low-income parents/caretakers. Meanwhile, HIP covers low-income adults, including the Medicaid expansion population and the majority of low-income parents or caretakers, through a consumer-driven health insurance model. Beneficiaries in HIP receive a high-deductible health plan and a Personal Wellness and Responsibility (POWER) account, modeled after a Health Savings Account (HSA), into which members and the state contribute.
Separately, Indiana also has a Hoosier Care Connect Medicaid managed care program, which covers the aged, blind, and disabled (ABD) population. New contracts with Anthem, Centene/Managed Health Services, and UnitedHealthcare for this program went into effect April 1, 2021.
RFP Timeline
The state intends to contract with four managed care organizations (MCOs). Contracts will run for four years beginning 2023, with two one-year renewal options, for a possible total of six years.
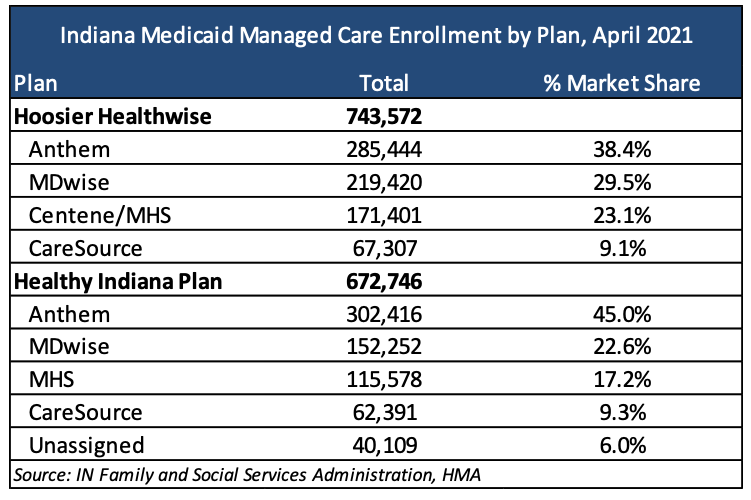
Current Market
Incumbents Anthem, CareSource, Centene/Managed Health Services, and MDwise serve approximately 1.4 million members as of April 2021. However, the state estimates enrollment to drop post-COVID. In 2023, Indiana predicts 680,293 to be enrolled in Hoosier Healthwise and 551,464 to be enrolled in HIP, totaling approximately 1.2 million members.
Evaluation
MCOs’ proposals will be scored out of a total 100 points (103 if bonus points are applied).
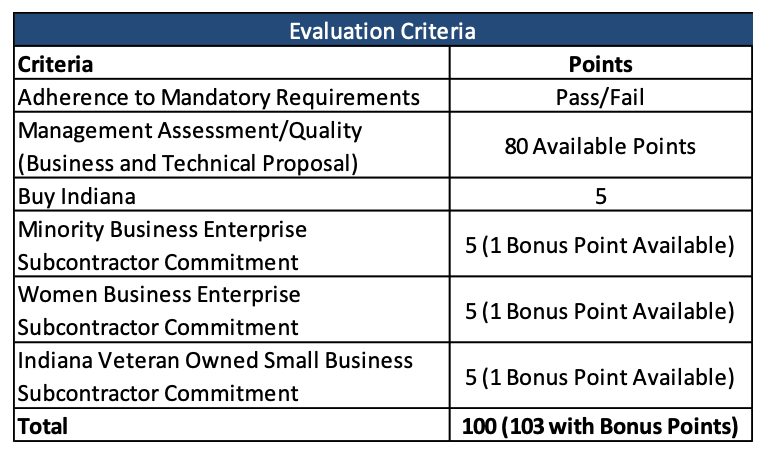
MCOs must submit proposals for both the Hoosier Healthwise and HIP programs. Technical proposals, worth up to 80 points, will be divided into three components: one common component that applies to both programs; one component that specifically addresses Hoosier Healthwise; and one component that specifically addresses HIP.
Common Component: Addresses overlapping requirements for both HHW and HIP:
- Section 1.0 (HHW + HIP) – Background
- Section 2.0 (HHW + HIP) – Administrative Requirements
- Section 7.0 (HHW + HIP) – Program Integrity
- Section 8.0 (HHW + HIP) – Information Technology (IT) Systems
- Section 9.0 (HHW + HIP) – Performance Reporting and Incentives
- Section 10.0 (HHW + HIP) – Failure to Perform/Non-compliance Remedies
- Section 11.0 (HHW + HIP) – Termination Provisions
Hoosier Healthwise Component: Addresses all other Hoosier Healthwise-specific SoW components not addressed in the Common Component:
- Section 3.0 (HHW) – Covered Benefits and Services
- Section 4.0 (HHW) – Member Services
- Section 5.0 (HHW) – Provider Network Requirements
- Section 6.0 (HHW) – Quality Management and Utilization Management
HIP Component: Addresses all other HIP-specific SoW components not addressed in the Common Component.
- Section 3.0 (HIP) – Covered Benefits and Services
- Section 4.0 (HIP) – Member Services
- Section 5.0 (HIP) – Provider Network Requirements
- Section 6.0 (HIP) – Quality Management and Utilization Management
- Section 12.0 (HIP) – HIP Plan Design and Member Eligibility
- Section 13.0 (HIP) – Billing and Collections
- Section 14.0 (HIP) – Personal Wellness & Responsibility (POWER) Accounts
The RFP can be found here.