This week our In Focus reviews the Tennessee Medicaid managed care request for proposals (RFP) released on June 11, 2021, by the State of Tennessee, Division of TennCare. Tennessee will select three plans to provide physical services, behavioral services, and Managed Long-Term Services and Supports (MLTSS), including nursing facility services and home and community-based services (HCBS), to beneficiaries enrolled in TennCare (Medicaid), CoverKids (Children’s Health Insurance Program), and Dual Eligible Special Needs Plans (D-SNP). Current incumbents serve over 1.5 million beneficiaries, with contracts worth $12 billion annually.
TennCare covers approximately 20 percent of the state’s populations. Selected Medicaid managed care organizations (MCOs), in addition to providing Medicaid integrated full-risk coverage, will also be required to lead delivery system transformation efforts including:
- Patient-Centered Medical Homes (PCMH): to improve the quality of primary care services for TennCare members
- Episodes of Care (Episodes): to improve the health care delivered in association with acute health care events
- Tennessee Health Link (THL): to coordinate health care services for TennCare members with the highest behavioral health needs
- Quality Improvement in Long-Term Services and Supports (QuILTSS) initiatives: to improve quality and shifting payment to outcomes-based measures for the QuILTSS program and for enhanced respiratory care
MCOs will operate a statewide D-SNP to serve members with dual eligibility for Medicare and full Medicaid benefits. The state can continue to contract with other plans to operate a D-SNP for beneficiaries that have partial Medicaid benefits, such as Medicaid coverage of Medicare premiums and/or cost-sharing.
MCOs must also be willing to accept 50 percent of the eligible population in each region of the state, and up to 70 percent if the state determines another MCO in the region is not adequately serving members and chooses to transfer members.
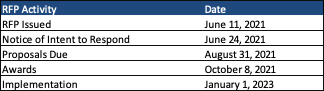
Timeline
Awards are expected October 8, 2021. Implementation is scheduled for January 1, 2023. Contracts begin January 2022 and run for three years with seven renewal options, not to exceed a total of 10 years.
Current Market
Incumbents Anthem, Blue Cross Blue Shield of Tennessee (BCBS-TN), and UnitedHealthcare served 1.56 members as of March 2021. BCBS-TN holds over 40 percent of the market share by enrollment.
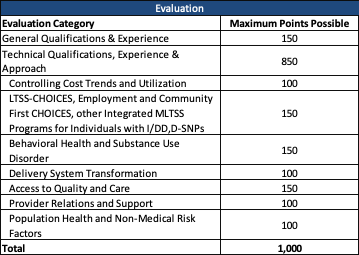
Evaluation
The state will score responses out of a total of 1,000 points, with the technical proposal worth 850 points.