This week, our In Focus reviews the the New Jersey Department of Human Services (DHS), Division of Medical Assistance and Health Services (DMAHS) draft proposal for the renewal of its 1115 Comprehensive Demonstration Waiver, released on September 10, 2021. The waiver was initially approved and implemented in October 2012. This demonstration is in its second five-year period and is slated to expire on June 30, 2022.
One significant change proposed in the draft renewal would be to further improve the integration and coordination of behavioral and physical health care by carving in most behavioral health services for all Medicaid beneficiaries in Medicaid managed care organizations (MCOs), beyond the BH services these organizations manage for a subset of members today. MCOs currently manage BH for members in managed long-term services and supports (MLTSS), individuals with developmental disabilities, and individuals dually eligible for Medicaid and Medicare (dual eligible) enrolled in a FIDE-SNP. BH services would now be carved into managed care for all Medicaid managed care members.
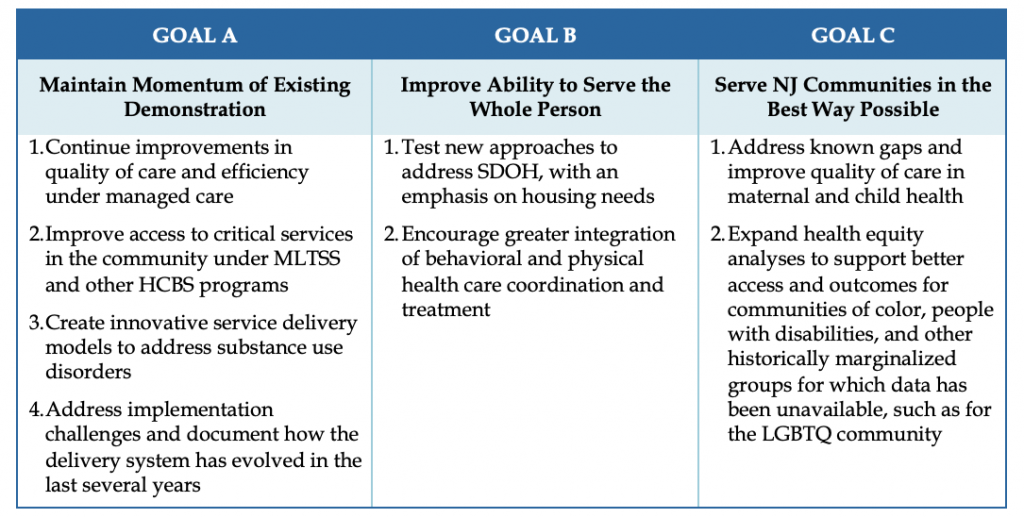
Proposed renewal goals align with the NJ FamilyCare program’s overall strategic goals. In a presentation to the New Jersey Medical Assistance Advisory Council (MAAC) on September 13, 2021, DHS and DMAHS leaders explained key strategic goals and elements of the proposal, with principal program goals as defined in Table 1.
Table 1. Principal Goals of New Jersey’s Proposed 1115 Waiver Renewal
The waiver renewal was well received by MAAC members who expressed optimism and appreciation to DHS and DMAHS leadership for preparing a comprehensive, thoughtful, and forward thinking strategy to guide the State’s Medicaid program over the next five years. Specific elements are detailed below.
Goal A. Maintaining Momentum On Existing Demonstration Elements
The State proposes to make further improvements to the Medicaid program for MLTSS enrollees by adding new nursing home diversion services – enhanced caregiver respite services from 30 to 90 days per year; caregiver counseling services; and additional nutritional supports such as a one-time pantry stocking for individuals who transition from an institution back to the community. The proposal would enable Medicaid eligibility sooner for individuals served by the Office of Public Guardian (OPG) who require long-term care through an OPG eligibility pilot program. It would also address challenges individuals seeking long-term care have experienced under the State’s Qualified Income Trusts program through a stakeholder engagement process.
The State is also proposing changes to the Community Care and Supports Programs with new flexibilities to allow for longer rehabilitation nursing facility stays for individuals served by the Division of Developmental Disabilities (DDD); modifying eligibility for the Supports program from the current threshold of beneficiaries age 21 and older to beneficiaries age 18 and older who are outside of their educational entitlement. The renewal would also modify the Community-Based Supports benefit to allow certain waiver services to be provided for DDD eligible members during an acute care hospital stay, such as communication and behavioral stabilization services that cannot be directly provided by the hospital. The State has also proposed to modify the current 30-day respite benefit for people enrolled in the Supports plus Private Duty Nursing (PDN) program from a community-based to an institutional setting.
Two important changes have been further proposed under the draft renewal waiver for individuals enrolled in the Children’s System of Care (CSOC), a division within the State’s Department of Children and Families (DCF). New Jersey seeks to qualify most children diagnosed with Serious Emotional Disturbance (SED) who meet the clinical and income eligibility criteria for Children’s Support Services Programs for full Medicaid State Plan services as a backstop to any existing health coverage, whether served in an institutional or community-based setting. Medicaid would remain the payor of last resort and children with SED would have access to all necessary behavioral and physical services. This change is designed to help further reduce the rates of institutionalization of children with SED in New Jersey. The proposal would also disregard parental income in the determination of Medicaid eligibility to allow certain children who currently have access only to waiver and behavioral health (BH) services to receive full State Plan benefits.
Goal B. Expand Ability To Serve The Whole Person
To better integrate behavioral and physical health care provided through NJ FamilyCare, the State has proposed an expansion of the role of Medicaid MCOs in their coordination and coverage of BH services. Under the current 1115 waiver MCOs are responsible for managing and paying for most Medicaid covered behavioral health services for members in MLTSS, individuals with developmental disabilities, and for dual eligibles enrolled in a FIDE-SNP. Under the latest proposal, these BH services would now be carved into managed care for all Medicaid managed care members. The State has further proposed to assess which BH services currently provided exclusively through Medicaid fee-for-service might be carved into managed care through a community-driven stakeholder process.
The renewal draft includes additional BH proposals including the placement of the State’s Certified Community Behavioral Health Clinic (CCBHC) pilot program under 1115 authority; Medicaid coverage of transitional BH services prior to release from a correctional facility; Medicaid reimbursement of short-term “diversion beds” to prevent unnecessary long-term psychiatric hospital placements; additional Medicaid funds to support BH providers in their adoption of electronic health records; and new adjunct therapies for children under age 21 with autism spectrum disorders.
To address the holistic needs of beneficiaries in relation to health and life outcomes, the State is requesting authority to rethink how the Medicaid program engages with members on SDOH, with a significant focus on health-related housing needs. Certain housing-related services would be exclusively available through the managed care delivery system, whether directly from the MCO’s housing specialist, contracted community-based organizations, or other vendors. The renewal proposal organizes housing services into two categories: Housing Transition Services such as a housing screening, individualized support plan, housing search and application supports, or assistance finding resources to cover housing expenses; and Tenancy Sustaining Services, for example, education and counseling on the role, rights, and responsibilities of a tenant and landlord, help resolving landlord or neighbor disputes, lease renewals, or budgeting and bill paying.
The State is also seeking authority under the renewal to expand eligibility for housing services. DMAHS further proposes to establish a housing team that will align Medicaid efforts with New Jersey’s existing housing ecosystem. The new housing team would identify synergies with other State agencies engaged in housing services; work with the State’s Healthy Homes initiative for individuals at risk of homelessness or institutionalization proposed in its American Rescue Plan spending plan; and monitor MCO accountability for health-related housing supports activities.
In addition to housing, SDOH enhancements would include the introduction of a Community Health Worker pilot program; a pilot program to provide medically-indicated meals for pregnant women who have pre-existing or gestational diabetes; and provide community-level support through the State’s Regional Health Hubs, not otherwise eligible for federal matching funds, to initiate other non-traditional Medicaid interventions. This might include support of wellness education primarily for the benefit of Medicaid beneficiaries, or direct investments in Health IT functionality that would facilitate improved care for Medicaid beneficiaries.
Goal C. Serve Communities The Best Way Possible
The waiver renewal proposes to improve upon the way NJ FamilyCare serves communities by reducing disparities in maternal and child health, and by promoting health equity and social justice.
To focus on maternal and child health the State recommends several strategies for addressing persistent racial and ethnic postpartum disparities, including Medicaid coverage, medical complications, emergency department utilization, postpartum-related hospitalizations and inpatient stays for ambulatory sensitive conditions, and neonatal expenditures. It also proposes to expand and extend its Home Visiting Pilot Program to complement universal home visitation legislation recently passed in New Jersey for newborns statewide.
DMAHS also commits to a renewed organizational focus on health equity and outcomes in its demonstration evaluation strategy by studying the impact of the 1115 waiver on improving access and outcomes based on race and ethnicity, immigration status, LGBTQ identity, geography, socioeconomic status, and other factors that have an impact on each beneficiary’s experience with the healthcare system.
Renewal Application Process
The State’s public comment period on the draft waiver renewal proposal runs from September 10 to October 11, 2021. The public can find the renewal application on the DHS website and how to submit comments here: https://www.state.nj.us/humanservices/dmahs/home/1115_demo.html.
DMAHS will integrate stakeholder feedback and estimates that it will submit a formal renewal application to CMS by November 1, 2021. CMS and DMAHS renewal negotiations are slated to begin December 15, 2021.