This week, our In Focus reviews the Texas Health and Human Services Commission (HHSC) draft request for proposals (RFP) for Texas STAR Health, the state’s Medicaid managed care program for foster care kids. The state is also seeking public input for the STAR+PLUS and STAR Kids Accountable Care Organization (ACO) programs, in anticipation of the reprocurement of these Medicaid managed care programs.
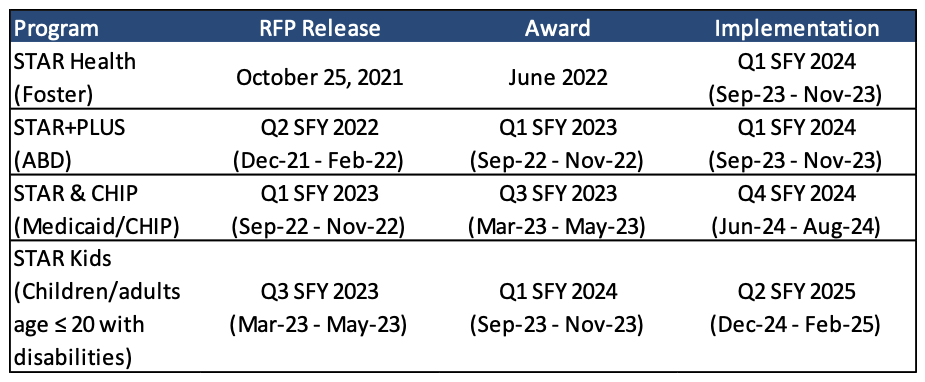
Upcoming Medicaid Managed Care Procurement Timeline
Texas is readying to release a multitude of RFPs for its Medicaid managed care programs according to the timeframes laid out in Table 1. In 2020, Texas cancelled the STAR and CHIP Medicaid managed care procurement and scrapped its STAR+PLUS contract awards because of discrepancies in the scoring of the bids.
Table 1. HHSC Medicaid Managed Care Procurement Timelines
Texas STAR Health Draft RFP
The first RFP scheduled for release is for STAR Health, which provides integrated physical and behavioral health services to children and young adults in the foster care system. Dental, vision, pharmacy, and personal care services are also included. There are approximately 43,700 beneficiaries enrolled in the program. Currently, Centene/Superior holds the contract.
An RFP for the STAR Health program was originally scheduled to be released in August 2021. Based on the draft RFP released by HHSC in early September 2021 (RFP No. HHS0010427), the final RFP is now scheduled for release on October 25, 2021, with a response submission deadline of December 28, 2021. HHSC will award one, six-year contract with up to three two-year renewals. Historically, the contract has been worth $361 million annually. The award is expected in June 2022, with implementation to be in the first state fiscal quarter of 2024, which runs from September 2023 through November 2023.
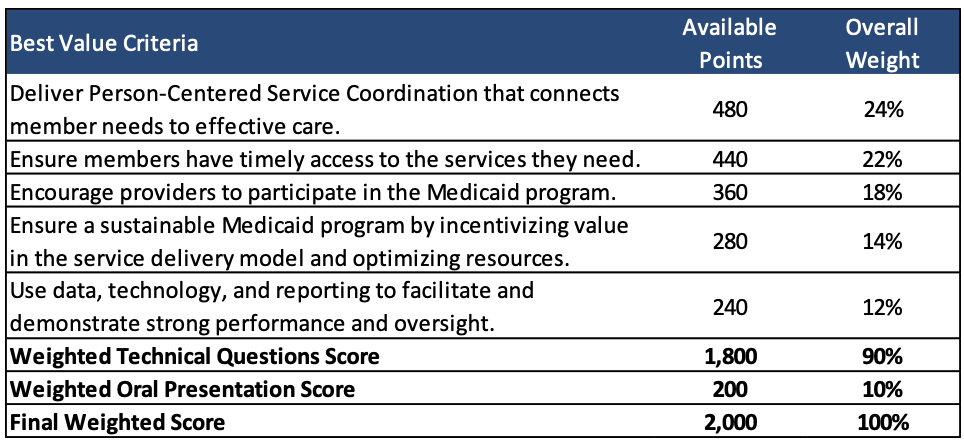
Proposals will be scored out of a total of 2,000 points. HHSC will award proposals that provide the best value to the state of Texas as determined by HHSC. Selection methodology after initial compliance screening will be based on a consensus scoring methodology as described in the draft RFP. Scoring along the best value criteria as detailed in the Draft RFP are described in Table 2.
Table 2. STAR Health Draft RFP Scoring
Texas STAR+PLUS Request for Public Input
The state threw out awards for the STAR+PLUS contracts in 2020 because of discrepancies in the evaluation and scoring of the bids. The STAR+PLUS contracts had been awarded to Aetna, Anthem/Amerigroup, Centene/Superior, El Paso Health, Molina, and UnitedHealthcare. Implementation was set to begin September 1, 2020. STAR+PLUS serves about 536,000 individuals who have disabilities or are age 65 or older. This marked the second time last year in which the procurement faced major setbacks because of problems with the procurement process. The current STAR+PLUS plans are Amerigroup/Anthem, Cigna, Centene, Molina, and UnitedHealthcare. At this time, Molina is in contract to purchase Cigna’s Medicaid STAR+PLUS and Medicaid-Medicare Program (MMP) business.
HHSC is now seeking public comments regarding the proposed best value criteria, which will be used to help evaluate bids for the upcoming STAR+PLUS Medicaid managed care procurement. The public comment period ends on September 17, 2021.
Texas STAR Kids ACO RFI
As required by the 86th Texas Legislature, HHSC released a request for information (RFI) on August 27, 2021, for “providing Medicaid benefits to children enrolled in the STAR Kids managed care program under an ACO or another value-based alternative payment model.” Responses are due September 27, 2021. The information gathered from the RFI will help HHSC determine the feasibility of using an alternative model. HHSC will need to consider the sustainability and long-term benefits of the model for providing care to children with complex medical needs. HHSC is gathering information on seven different elements to assess the potential options:
- Overall structure
- Including whether it should be a provider-led, MCO-led, or community partner-led model
- Payment structure
- Including whether it should be a shared savings model, a per-member-per-month payment for care coordination, a full-risk capitation model, a phased transition to a full-risk capitation model, or other model
- Contracting
- Care structure
- Quality Measures
- Claims and Data Collection
- General Information
STAR Kids serves a total of 168,000 individuals with disabilities age 21 or younger. CVS/Aetna Better Health was most recently awarded a Texas STAR Kids Medicaid managed care contract on May 8, 2020, in the seven-county Dallas service area. The procurement followed the exit of Children’s Medical Center, which served approximately 9,000 STAR Kids members. Anthem/Amerigroup also holds a STAR Kids contract for the Dallas Service Area. A new procurement for the entire STAR Kids program is expected to be released in 2023. Other incumbents include Blue Cross Blue Shield of Texas, Centene, Community First Health Plan, Cook’s Children’s Health Plan, Driscoll Children’s Health Plan, Texas Children’s Health Plan, and UnitedHealthcare.