This week, our In Focus section reviews the Oklahoma request for public feedback in the SoonerCare program design, released on June 18, 2020. The Oklahoma Health Care Authority (OHCA) and Governor Kevin Stitt are seeking stakeholder input for the state’s Medicaid managed care program design before finalizing a request for proposals (RFP). The RFP, which is currently in development, is scheduled to drop in the fall and has an implementation date of October 2021. Individuals, program participants, providers, trade associations, companies, and other organizations are encouraged to submit responses by August 17, 2020.
Background and Past Medicaid Managed Care Attempts
Oklahoma used to have a fully capitated Medicaid managed care program, which ended in 2003 following a rate dispute with one of its leading contracted plans. The program, called SoonerCare Plus, had served urban areas of the state. Between 1997 and 2003, managed care organizations (MCOs) began to drop out, leaving only three MCOs. The remaining MCOs sought an 18 percent rate increase for 2004. While two of the plans agreed to a lower rate, the remaining plan held out causing OHCA to end the program.
A separate Primary Care Case Management program serving rural areas called SoonerCare Choice was expanded statewide in 2004 and has been the state’s main Medicaid program ever since.
More recently, Oklahoma had attempted to create a managed care program for the aged, blind, and disabled (ABD) population, but in June 2017, canceled the procurement for SoonerHealth+ due to a lack of funding. Start-up costs for SoonerCare+ were projected at more than $100 million over the first several years of the program, and legislators denied a request for $52 million in near-term funding needed to move ahead with the RFP.
The newest push for a statewide Medicaid managed care program comes after Governor Kevin Stitt backtracked on a Healthy Adult Opportunity (HAO) waiver, which would have expanded Medicaid, created an enhanced Primary Care Case Management program, and implemented a block grant financing model.
On June 30, 2020, voters approved a ballot measure to expand Medicaid to eligible adults, estimated to cover 215,000 low income individuals.
Request for Public Feedback
Oklahoma is seeking feedback on the following categories to develop the new RFP: managed care enrollees; benefits provided through managed care organizations; quality and accountability; care management and coordination; member services; provider payments and services; network adequacy; grievances and appeals; and administrative requirements.
Some notable questions are summarized below:
Managed Care Enrollees
The ABD population and dual eligibles will initially remain in fee-for-service (FFS). However, the state wants to know from stakeholders how and when to transition ABD and other initially excluded individuals to managed care. Additionally, if the state should require each MCO to enroll all populations or allow specialty plans so that an MCO could propose to serve only certain populations, such as children in foster care, American Indians/Alaska Natives, people with Serious Mental Illness, or other groups.
Benefits Provided through MCOs
Under SoonerCare, MCOs will manage physical health, behavioral health, vision, and non-emergency medical transportation for their members. In relation to this, the state is seeking feedback on strategies to improve the integration of services, specifically behavioral and physical health, including through provider communication, shared assessments and planning, and data sharing. Furthermore, how MCOs can improve access to evidence-based behavioral health care and access to transportation for SoonerCare members, including if ride-sharing services like Uber and Lyft should continue to be an option.
Care Management and Coordination
The state is seeking input on how to best coordinate care for individuals with complex or multiple needs. MCOs will support Patient Centered Medical Homes under a re-design that utilizes a value-based strategy that includes integration of behavioral health and social determinants, enhanced care coordination payments, and performance measurement.
Administrative Requirements
Oklahoma is also considering whether to require MCOs to offer health plans on the Oklahoma Health Insurance Marketplace.
Current Market
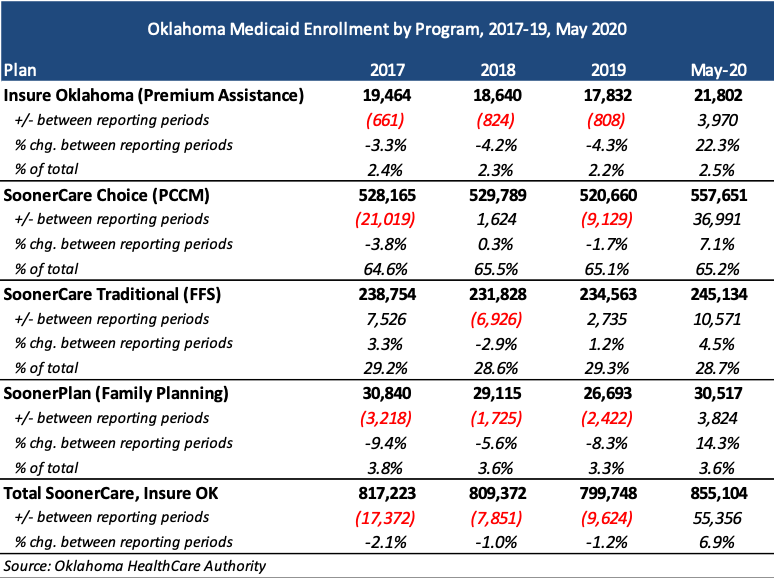
As of May 2020, there are over 855,104 Medicaid members. Approximately 65 percent are in the SoonerCare PCCM program and 29 percent are in the traditional FFS program.
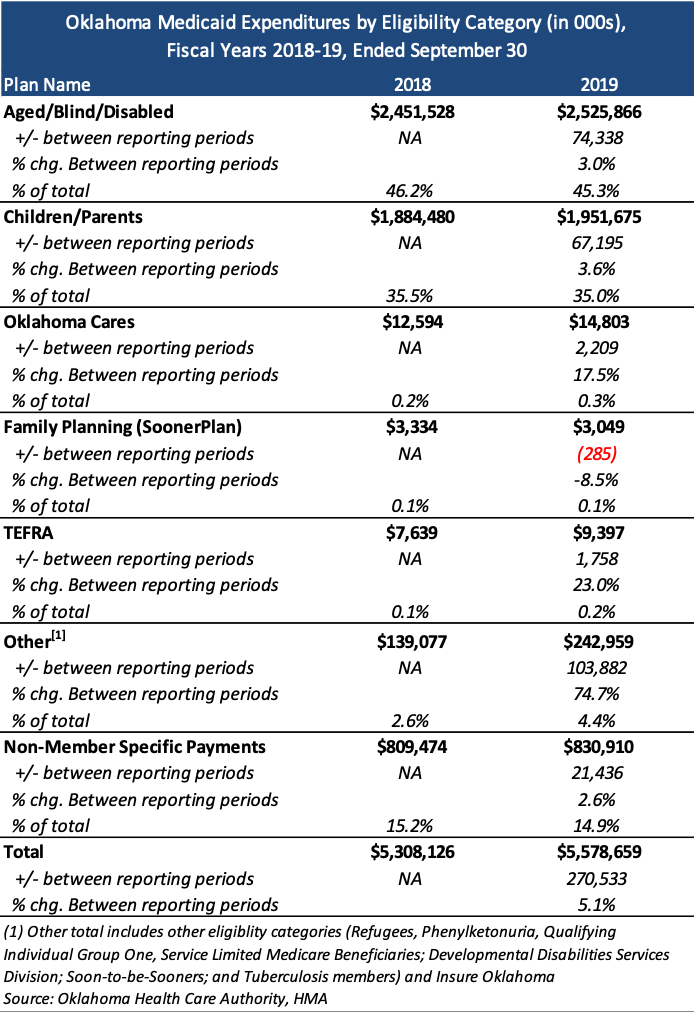
Total expenditures for Medicaid were approximately $5.6 billion in 2019.