This week, our In Focus section reviews the Hawaii request for information (RFI) regarding reprocurement of the state’s QUEST Integration (QI) Medicaid managed care program, released on July 21, 2020. QI covers approximately 360,000 individuals, including pregnant women, children, parents/caretakers, adults, and individuals who are aged, blind, or disabled (ABD). The state had awarded contracts earlier this year, however, the contracts were rescinded as the state focused on their response to COVID-19.
Separately, Hawaii released an RFI for the reprocurement of the specialty behavioral health carve-out Community Care Services (CCS) program, which helps 5,200 Medicaid-eligible adults with severe mental illness connect with behavioral health resources, housing, employment, and transportation.
Background
Hawaii implemented the QI program in 2015. Previously, the state operated the Quest program, which covered acute, primary, and behavioral health care services for children, families, pregnant women, and childless adults, and the QUEST Expanded Access (QExA) program, which covered ABD individuals, dual eligibles, and individuals with intellectual or developmental disabilities. Under Quest Integration, the state was able to consolidate the two programs into one demonstration.
In 2013, the state began to move behavioral health services for individuals with a serious mental illness (SMI) or severe and persistent mental illness (SPMI) from fee-for-service to managed care through the CCS program. WellCare/Ohana has held the contract since 2013.
Hawaii also has a behavioral health carve-out for children, via an MOU with the Children and Adolescent Mental Health Division (CAMHD) at the Department of Health (DOH). Additionally, DOH recently launched the Coordinated Access Resource Entry System (CARES), a substance use disorder (SUD) organization, to further develop behavioral health resources in the state. The DOH Adult Mental Health Division (DOH-AMHD) provides behavioral health services for adults who are legally encumbered or uninsured.
Previous Quest Integration RFP
Hawaii released its QUEST Integration (QI) Medicaid Managed Care request for proposals (RFP) in September 2019, intending to contract with four health plans to serve Medicaid and CHIP members in Oahu; with two of the plans operating statewide. In January 2020, the state awarded the contracts to AlohaCare, Hawaii Medical Service Association (HMSA), UnitedHealthcare, and WellCare/Ohana. HMSA and United would have served statewide. Implementation was set to begin July 1, 2020, with contracts running through December 31, 2025, plus four optional years. However, the contracts, worth $2.2 billion annually, were rescinded and current contracts were extended. The decision to rescind the awards, which would have reduced the number of contracted Medicaid managed care plans serving members statewide, was prompted by COVID-19, according to Med-QUEST Division administrator Judy Mohr Peterson. Current incumbents are AlohaCare, HMSA, Kaiser, Ohana, and United.
Under the RFP, Hawaii also intended to implement the Hawaii ‘Ohana Nui Project Expansion (HOPE) program, focusing on health and wellness. The program would invest in primary care, prevention, and health promotion; improve outcomes for individuals with special health care needs through care management; reform and align payment to providers; and support community-driven initiatives to improve population health.
RFIs
Hawaii is seeking information for the reprocurement from all stakeholders, not just managed care organizations (MCOs). Responses are due August 14, 2020. The state emphasizes the QI procurement and the CCS procurement as interrelated programs and is soliciting feedback on how the two programs can achieve greater alignment. Stakeholders are not required to respond to both RFIs.
As per the last procurement, Hawaii is also intending to implement the HOPE initiative to address larger trends in healthcare delivery. Due to the COVID-19 pandemic, plans will need to accelerate efforts to provide services in new ways, like telehealth. The HOPE program will also focus on Medicaid beneficiaries with the highest cost, and most complex health and social needs.
Elements of the RFIs include:
Administration
The previous RFP was looking to contract with four health plans, two of which would operate statewide. The RFI asks how many plans stakeholders think should operate in the state, and how many should be regional and how many statewide.
Care Coordination/Integration
Hawaii is seeking information on how to best align all the programs and integrate behavioral health with physical health to promote a continuum of health and wellness. Furthermore, how to improve care and service coordination across the programs, specifically for individuals with complex needs.
COVID-19
The state is interested in understanding what program flexibilities should be continued beyond the public health emergency; how to expand telehealth; and how to support providers during the pandemic.
CCS
Hawaii is seeking feedback on the best ways to align CCS with QI, Hawaii CARES, DOH-AMHD, DOH-CAMHD. This includes standardizing and reducing administrative burden, as well as aligning incentives that improve outcomes. CCS has five service levels within a stepped care model; the state is seeking recommendation for a case management reimbursement model that would produce best case management practices and services and incentivize providers to place members along the stepped care continuum.
Current Market
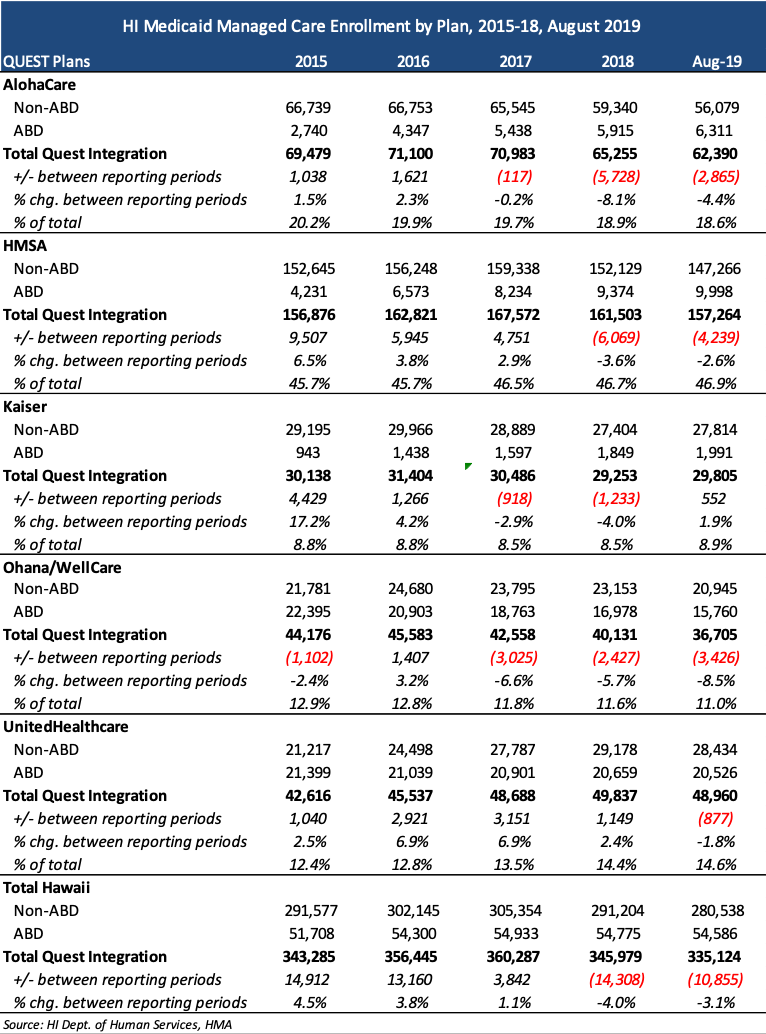
Current Medicaid MCO incumbents are AlohaCare, HMSA, Kaiser, WellCare, and UnitedHealthcare, serving more than 335,000 individuals, as of August 2019. HMSA (an independent licensee of the Blue Cross Blue Shield Association) has the largest market share, with 47 percent of current enrollment. Medicaid enrollment in Hawaii hit 348,000 as of May 2020, with recent enrollment growth tied to the COVID-19 pandemic. The RFI lists enrollment of 360,000 as of July 2020.