This week's roundup:
- In Focus: Medicare Advantage Capitation Rates and Part C and Part D Payment Policies

- Health Management Associates Acquires Crestline Advisors

- Arizona to Award $40 Million to HCBS Providers

- California, Michigan Consider Legislation to Ensure Preventive Care Coverage at No Cost to Individuals

- Colorado Legislature Debates Fiscal 2024 Budget Bill with $80 Million to Replace Enhanced FMAP

- Connecticut House Committee Advances 2 Bills to Increase Income, Asset Limits for HUSKY C

- Indiana Legislature Extends Medicaid Reimbursement Rate Hike for Out-of-state Children’s Hospitals

- Iowa House Committee Holds Hearing on Bill to Create Eligibility Verification System for Medicaid

- Michigan Launches Enhanced Medicaid Dental Benefits, Increased Dental Provider Reimbursement Rates

- Montana House Passes Bill to Increase Medicaid Reimbursement Rates to Ambulance Providers

- New York Implements Medicaid FFS Pharmacy Benefit Program

- Redeterminations News: Oregon, Pennsylvania, Texas, Virginia

- CMS to Increase Medicare Advantage Payments by 3.3 Percent in 2024

- CMS Proposes Increasing Medicare Reimbursement Rates for Skilled Nursing Facilities by 3.7 Percent in 2024

- HouseWorks Acquires Associated Home Care

- UnitedHealth Group to Reduce Use of Prior Authorizations

In Focus
Medicare Advantage Capitation Rates and Part C and Part D Payment Policies
This week, our In Focus section reviews the recently announced major policy updates from the Centers for Medicare and Medicaid Services (CMS) that affect the Medicare Advantage (MA) and Part D programs.
First, on January 30, CMS released the final Risk Adjustment Data Validation Final Rule, a highly anticipated and controversial policy that establishes the agency’s approach to auditing MA Organizations’ (MAOs) risk-adjustment payments and collecting overpayments as needed. Second, CMS released the CY 2024 Advance Notice for MA Capitation Rates (Part C) and Part D Payment Policies on February 1, 2023. HMA’s summary of the advance notice is available here.
Most recently, on March 31, 2023, CMS released the CY 2024 Final Rate Notice for Medicare Advantage (MA) Capitation Rates and Part C and Part D Payment Policies, which incorporates CMS’s responses to public comments on the Advance Notice. These changes reflect CMS’ continued efforts to strengthen oversight in the MA program, including improving payment accuracy, and implementation of Part D policies from the Inflation Reduction Act (IRA).
Below are highlights of some of the key provisions of the CY 2024 Final Rate Notice and significant changes CMS made from the Advance Notice to the Final Rate Notice.
Risk Adjustment: The Final Rate Notice details the updated risk adjustment model using restructured condition categories based on ICD-10 codes, newer data, and clinical adjustments made to ensure the conditions are stable predictors of costs in the model. Specifically, diagnoses data will come from 2018 rather than 2014 and expenditure data will come from 2019 rather than 2015 to reflect changes in costs. These updates should more accurately reflect the cost of caring for beneficiaries and make payments less susceptible to discretionary coding that can lead to excess payments to MA plans.
Also, CMS changed course from its initial proposal in the Advance Notice to implement the above risk adjustment model changes fully in 2024, and instead decided to phase in these changes over three years. The updated risk adjustment policy will be phased in over three years for organizations other than PACE. As a part of the agency’s phase-in plan, 67 percent of the CY 2024 risk adjustment will come from the risk scores measured under the 2020 adjustments and 33 percent will come from the 2024 adjustments. In CY 2025, 67 percent of the risk adjustment will come from the 2024 adjustment. In 2026, 100 percent of the risk adjustment will come from the 2024 adjustment. For PACE organizations in CY 2024, CMS will continue to use the 2017 risk adjustment model and associated frailty factors to calculate risk scores.
Effective Growth Rate: The effective growth rate identified within the Final Rate Notice for CY 2024 is 2.28%, up from 2.09% in the Advance Notice. The Effective Growth Rate is largely driven by growth in Medicare Fee-for-Service expenditures. CMS will phase in a technical adjustment to remove MA-related indirect medical education and direct graduate education costs from the historical and projected expenditures. The technical adjustment to the Effective Growth Rate will be phased in over three years, where 33 percent of the adjustment will apply in CY 2024, 67 percent in CY 2025, and 100 percent in CY 2026.
Payment rate impact in MA: CMS expects that average payments to MAOs will increase by 3.32 percent in CY 2024 because of the finalized rate announcement, which is higher than the 1.03 percent increase outlined in the Advance Notice. This will result in an estimated $13.8 billion increase in MA payments for CY 2024.
Medicare Part D: The changes from the Inflation Reduction Act to the Part D drug benefit will be implemented as described in the Advance Notice. The changes for CY 2024 include:
-
- Elimination of cost sharing for covered Part D drugs for beneficiaries in the catastrophic phase of coverage.
-
- Increased income limits from 135 percent of the federal poverty limit (FPL) to 150 percent of the FPL for the low-income subsidy program (LIS) under Part D for the full LIS benefit with a $0 deductible.
-
- Continuation of the policy to not apply the deductible for any Part D covered insulin product. Also, in the initial coverage phase and the coverage gap phase, cost sharing must not exceed the applicable copayment amount, which for CY 2024 is $35 for a month’s supply of each covered insulin product.
-
- Continuation of the policy not to apply the deductible to any adult vaccine recommended by the Advisory Committee on Immunization Practices (ACIP). Also, the statute requires these vaccines to be exempt from any co-insurance or other cost sharing, including cost sharing for vaccine administration and dispensing fees for such products, when administered in accordance with ACIP’s recommendation, for beneficiaries in the initial coverage and coverage gap phases.
-
- Base beneficiary premium (BBP) growth will be held to no more than 6 percent by statute. The BBP for Part D in 2024 will be the lesser of the BBP for 2023 increased by 6 percent or the amount that would otherwise apply under the original methodology if the IRA were not enacted.
Star Ratings: Medicare Advantage star ratings for CY 2024 will include 30 measures with 12 included in the 2024 categorical adjustment index (CAI) values. By contrast, Part D star ratings for CY 2024 will include 12 measures with 5 of those measures included in the 2024 CAI values. The CAI for the 2024 Star Ratings is expected to be issued later in 2023. The CAI was introduced in 2017 as an interim analytical adjustment to address the average within-contract disparity in performance among beneficiaries who receive a low-income subsidy, are dual eligible, and/or are disabled.
The Final Rate Notice also includes three criteria for determining if Part C and D organizations are eligible for the “extreme and uncontrollable circumstances” adjustment to their Star Ratings. To be eligible, an organization must be in a 1) service area that is within the “emergency area” during the “emergency period,” 2) service area that is within a geographic area designated in a major disaster declaration under the Stafford Act and the Secretary exercised authority under the Act based on the same triggering events, and 3) a certain minimum percentage (25 or 60 percent) of beneficiaries must reside in the Federal Emergency Management Agency (FEMA) designated Individual Assistance area at the time of the extreme and uncontrollable circumstance. If an organization meets the criteria outlined and meets the 25 percent minimum, then they will receive the higher of their measure-level rating from the current and prior Star Ratings years for purposes of calculating the 2024 Star Ratings. For organizations meeting the 60 percent minimum and the other criteria, they are excluded from the measure-level cut point calculations for non-CAHPS measures, and the performance summary and variance thresholds.
Upcoming LinkedIn Live: Join HMA for our Future Frame Conversation on Policy Changes in Medicare Advantage and the Implications for Coding, Risk Adjustment, and Reimbursement. Tuesday April 11, 2023, at 12 p.m. E.T. Click here to register.
If you have questions about the contents of CMS’s MA final notice and how it will affect MA plans, providers, and patients, contact Julie Faulhaber, Amy Bassan, or Andrea Maresca.
Health Management Associates Acquires Crestline Advisors
Jay Rosen, founder, president, and co-chairman of Health Management Associates (HMA), announced on April 4, 2023, the firm’s acquisition of Crestline Advisors, an Arizona based healthcare consulting firm.
Founded in 2013, Crestline Advisors supports health plans, provider organizations, and state agencies with an array of services designed to help them navigate the changing healthcare landscape. The company’s team of independent consultants has an extensive track record of developing successful RFP responses, provider networks, and business development strategies to fuel client success.
“Crestline Advisors brings an impressive mix of expertise and relentless client focus – that delivers results – to HMA,” Rosen said. “Their ability to consistently develop winning proposal responses for Medicaid managed care organizations (MCO) complements our extensive MCO supports as we continue to expand the ways in which we serve our clients.”
In addition to Crestline’s proposal response development and MCO network management and operations support services, the company also assists clients with regulatory and contract compliance, accreditation, and strategic planning for business development.
“Crestline has demonstrated a commitment to supporting health plans, providers, and states to improve healthcare for Medicaid beneficiaries,” said Crestline CEO Susan Dess. “We firmly believe that as part of the HMA family of companies we will bring even more success to our clients and drive continued growth and development in Medicaid healthcare delivery.”
Dess and Tim Mechlinski will continue to lead Crestline Advisors, an HMA Company, as managing directors. Terms of the transaction were not disclosed.
HMA Roundup
Arizona
Arizona to Award $40 Million to HCBS Providers. The Arizona Health Care Cost Containment System announced on March 27, 2023, that it will award $40 million to providers for projects aimed at strengthening home and community-based services (HCBS). Applications are open from April 17 to May 16. Providers can apply for up to $500,000 for programmatic or infrastructure projects to improve health, safety, and member experience. Read More
California
California, Michigan Consider Legislation to Ensure Preventive Care Coverage at No Cost to Individuals. Becker’s Payer Issues reported on April 4, 2023, that California and Michigan are both considering legislation to ensure preventive care coverage at no cost to individuals after a federal judge struck down some of the requirements under the Affordable Care Act. The Biden administration has appealed the ruling. Read More
Colorado
Legislature Debates Fiscal 2024 Budget Bill with $80 Million to Replace Enhanced FMAP. The Denver Business Journal reported on March 30, 2023, that Colorado lawmakers are debating a budget bill for fiscal 2024 that includes $80 million to make up for the loss of enhanced federal Medicaid matching funds following the end of the national emergency. The bill also includes $3.9 million for the Office of Behavioral Health. Read More
Connecticut
House Committee Advances 2 Bills to Increase Income, Asset Limits for HUSKY C. The Connecticut Mirror reported on April 5, 2023, that the Connecticut House Human Services Committee advanced two bills (House Bill 5001 and House Bill 6630) to increase the income and asset limits for HUSKY C, the state’s Medicaid program for individuals who are over 65, blind or disabled. The first bill proposes raising the income limit from $1,182 to $1,465 per month and the asset limits to $3,600 for a single person, from $1,600, and to $5,400 for a couple, from $2,400. The second proposes bringing the HUSKY C income limit up to the same level as HUSKY D, which is 138 percent of the federal poverty level, and increasing the asset limits to $10,000 for an individual and $15,000 for a couple. Legislators are working to decide which bill will be included in the budget proposal. Read More
Medicaid Spending Increases 0.8 Percent in 2021, Report Finds. Connecticut Public Radio reported on April 3, 2023, that Medicaid spending in Connecticut increased by 0.8 percent in 2021, according to a report from the state Office of Health Strategy. The report also found that Medicare spending increased by 1.4 percent during that period. Overall health care spending increased by 6 percent, but most of the increase came from commercial health insurance. Read More
Florida
House Subcommittee Advances Bill Allowing Medicaid Beneficiaries with Serious Mental Illness to Avoid Drug Step Therapy. Health News Florida/News Service of Florida reported on April 4, 2023, that the Florida House Health Regulation Subcommittee advanced a bill (HB 183) that would allow Medicaid beneficiaries with serious mental illness to avoid drug step therapy, which requires an individual to try one type of medication to determine if it is effective before being allowed to try a more expensive one. A Senate version of the bill (SB 112) has been cleared by two committees. Read More
Hawaii
Senate Committee to Rehear Bill Allowing Medicaid Coverage of Autism Treatment for Adults. State of Reform reported on March 29, 2023, that the Hawaii Senate Health and Human Services Committee deferred for rehearing a bill (Senate Concurrent Resolution 119) that would require Medicaid coverage of applied behavioral analysis to adults diagnosed with Autism Spectrum Disorder. Read More
Idaho
House Passes Updated Fiscal 2024 Medicaid Budget. The Idaho Capital Sun reported on March 29, 2023, that the Idaho House passed a revised fiscal 2024 Medicaid budget. The revised budget lowered proposed Medicaid funding from $4.7 billion to $4.5 billion. The budget now heads to the Senate for consideration. Read More
Indiana
Legislature Extends Medicaid Reimbursement Rate Hike for Out-of-state Children’s Hospitals. Lakeshore Public Radio reported on March 29, 2023, that the Indiana Senate passed a bill (House Enrolled Act 1313) extending a temporary increase in Medicaid reimbursement rates for out-of-state children’s hospitals through June 2025. The bill now goes to Governor Eric Holcomb for his signature. Read More
Iowa
House Committee Holds Hearing on Bill to Create Eligibility Verification System for Medicaid. The Iowa Capital Dispatch reported on April 4, 2023, that the Iowa House Appropriations Committee held a public hearing on Senate File 494, a bill that would direct the Department of Health and Human Services to create a computerized income, asset, and eligibility verification system for public assistance programs, including Medicaid. The Senate already passed the bill, and a House subcommittee advanced it. Read More
Michigan
Michigan Launches Enhanced Medicaid Dental Benefits, Increased Dental Provider Reimbursement Rates. WILX reported on April 3, 2023, that Michigan has enhanced Medicaid dental benefits and increased Medicaid reimbursement rates for dental providers, effective April 1. Enhanced benefits include sealants, root canals, crowns, and deep cleanings. Providers will be paid at 100 percent of the average commercial rate to incentivize participation in Medicaid. Read More
Minnesota
Minnesota Continues to Face Behavioral Health Provider Shortage in Rural Counties. Kaiser Health News reported on April 3, 2023, that Minnesota continues to face a behavioral health provider shortage in its rural areas. Recent efforts to improve access to behavioral services have fallen short, the article points out. Read More
Montana
House Passes Bill to Increase Medicaid Reimbursement Rates to Ambulance Providers. KTVH reported on April 4, 2023, that the Montana House passed a bill (House Bill 828) to increase Medicaid reimbursement rates to ambulance providers. The increase would be funded by an ambulance provider assessment fee of 5.75 percent of revenues. Read More
New Hampshire
Adult Medicaid Dental Program Begins. The Concord Monitor reported on March 31, 2023, that New Hampshire launched its Medicaid dental program for adults on April 1. NorthEast Delta Dental, in partnership with DentaQuest, will provide the dental benefits. Eligible Medicaid beneficiaries were automatically enrolled. Covered services include X-rays and examinations, cleanings, fillings, and other oral surgeries, as well as transportation to dental appointments. Read More
New York
New York Implements Medicaid FFS Pharmacy Benefit Program. New York Governor Kathy Hochul announced on April 1, 2023, the implementation of NYRx, the state’s Medicaid fee-for-service (FFS) pharmacy benefit program. Previously, pharmacy benefits were carved into Medicaid managed care. Hochul committed $705 million in her fiscal 2024 budget to ensure 340b health care providers were not negatively impacted by the transition. Two New York community health providers filed a lawsuit in March to halt the transition. Read More
Oregon
Oregon Expects Up to 300,000 Medicaid Beneficiaries to Lose Coverage During Redeterminations. The Oregon Capital Chronicle reported on April 3, 2023, that the Oregon Health Authority expects up to 300,000 Medicaid beneficiaries to lose coverage when eligibility redeterminations resume. The state will send out renewal notices over the next 10 months and those who no longer qualify will have 60 days to find new coverage, most likely on the Exchange. The state will also have a transition team available beginning April 13 to help individuals find new coverage. In July 2024, Oregon is planning on launching its Basic Health Program to cover individuals from 138 to 200 percent of poverty. Read More
Pennsylvania
Medicaid Department Faces Staffing Shortages as Redeterminations Begin. The Gettysburg Times reported on April 4, 2023, that the Pennsylvania Department of Human Services is facing staffing shortages as it begins the Medicaid redeterminations process. Advocates are pushing the state to conduct more ex parte Medicaid renewals to make up for the shortages. Read More
Texas
Texas to Complete Medicaid Redeterminations by May 2024. The Texas Health and Human Services Commission (HHSC) announced on April 3, 2023, that it expects to complete the Medicaid redeterminations process by May 2024, with the help of an additional 1,000 staffers hired since last April. The state will utilize social media, emails, text messages, and partner organizations for outreach. Read More
Virginia
Governor Proposes $38 Million Amendment to Stopgap Budget for Medicaid Eligibility Redeterminations. The Center Square reported on March 30, 2023, that Virginia Governor Glenn Youngkin is proposing a stopgap budget amendment of $38 million to support Medicaid eligibility redeterminations. The legislature approved the stopgap budget before adjourning in February without passing a final budget. Lawmakers will return to session in April. Read More
National
Community Health Centers Worry About Financial Implications of Medicaid Redeterminations. Health Payer Intelligence reported on April 5, 2023, that community health centers are concerned about potential financial and operational challenges from the potential loss of Medicaid patients following eligibility redeterminations, according to a survey from the National Association of Community Health Centers. More than a quarter of health centers expect at least 15 percent of Medicaid beneficiaries will lose coverage during redeterminations, including patients receiving treatment for chronic conditions. Read More
CMS Proposes Increasing Medicare Reimbursement Rates for Skilled Nursing Facilities by 3.7 Percent in Fiscal 2024. Modern Healthcare reported on April 4, 2023, that the Centers for Medicare & Medicaid Services (CMS) released a proposed rule to increase Medicare reimbursement rates by 3.7 percent for skilled nursing facilities in fiscal 2024. CMS will also publish a regulation establishing minimum staffing ratios at nursing homes in the spring. Read More
House Speaker Proposes Strengthening Medicaid Work Requirements. The Hill reported on April 4, 2023, that House Speaker Kevin McCarthy (R-CA) has proposed strengthening Medicaid work requirements. Republicans want the proposal included in a bipartisan agreement on raising the debt ceiling. Read More
Rural Hospitals Pursue Mergers to Survive. Modern Healthcare reported on April 3, 2023, that about 17 percent of 325 unprofitable rural hospitals merged with another organization from 2010 to 2018, according to a Health Affairs study. While the mergers can help rural hospitals stay afloat, they often mean higher prices for services. Read More
Medicaid Reimbursement Rates for Mental Health Treatment Vary by State. Oregon Health and Science University reported on April 3, 2023, that Medicaid reimbursement rates for the same mental health treatment vary by state, in a study published in Health Affairs. The study found that Nebraska, Alaska, and Arkansas pay the highest rates, while Pennsylvania, Rhode Island, and Maine pay the lowest. The study also found that Medicaid paid about 80 percent of Medicare rates on average. Read More
CMS to Increase Medicare Advantage Payments by 3.3 Percent in 2024. The Centers for Medicare & Medicaid Services (CMS) said on March 31, 2023, that payments to Medicare Advantage and Part D plans will increase an average of 3.3 percent or $13.8 billion in 2024. In an earlier draft notice, CMS had proposed a one percent increase. This year, CMS will also begin to hold MA plans more accountable by cracking down on abusive marketing schemes, addressing problematic prior authorization practices, making behavioral health access easier, and raising the bar on quality. Read More
Medicare Funding Shortages Could Impact Benefits by 2031, Trustees Report Predicts. The Associated Press reported on March 31, 2023, that Medicare is expected to be unable to pay full benefits for inpatient hospital visits and nursing home stays by 2031, according to a report by the Trustees of the Social Security and Medicare. The report found that Medicare would be able to cover 89 percent of costs in 2031. The Trustees recommend Congress address the trust fund shortfalls. Read More
Biden Administration Appeals Judge’s Ruling Striking Down Mandatory Coverage of Preventive Care at No Cost to Members. CNBC reported on March 31, 2023, that President Biden has appealed a federal judge’s ruling that health plans do not have to cover preventive care at no cost to members, as mandated under the Affordable Care Act. The case now heads to the U.S. Fifth Circuit Court of Appeals. Read More
CMS Awards $5.9 Million to Increase Coverage of American Indian, Alaskan Native Children in Medicaid, CHIP. The Centers for Medicare & Medicaid Services (CMS) awarded on March 30, 2023, $5.9 million in cooperative agreements to seven organizations to increase the participation of eligible, uninsured American Indian and Alaskan Native (AI/AN) children in Medicaid and the Children’s Health Insurance Program (CHIP). The awards are part of the HEALTHY KIDS Act, which provides funding to educate AI/AN families about the availability of coverage under Medicaid and CHIP, identify AI/AN children likely to be eligible for these programs, and assist families in applying for and renewing coverage. Read More
U.S. Senate Passes Measure to End COVID-19 National Emergency. Roll Call reported on March 29, 2023, that the U.S. Senate voted to terminate the COVID-19 pandemic national emergency order. The House approved the measure in February. The national and public health emergencies are already set to end in May. President Biden is expected to sign the measure. Read More
Industry News
Pinnacle Treatment Centers Acquires Opioid Treatment Programs in New Jersey, Pennsylvania. Pinnacle Treatment Centers announced on April 5, 2023, the acquisition of four outpatient opioid addiction treatment programs in New Jersey and Pennsylvania. All four were previously operated by Recovery Centers of America. Read More
HouseWorks Acquires Associated Home Care. HouseWorks announced on April 4, 2023, its acquisition of Associated Home Care, the personal care division of Amedisys, which provides home health, hospice, and high-acuity care. HouseWorks provides personal care services in Massachusetts, New Hampshire, Pennsylvania, and Maine. Read More
Sanford Health, Fairview Health Services Delay Merger Again. Modern Healthcare reported on April 3, 2023, that Sanford Health and Fairview Health Services are delaying their $14 billion merger for the second time. The deal was initially expected to close on March 31 and then again on May 31 to give Minnesota Attorney General Keith Ellison more time to evaluate it. The health systems will notify the attorney general’s office with 90 days notice prior to the new closing date. Read More
Elara Caring to Acquire Assisted Daily Living. Home health provider Elara Caring announced on April 3, 2023, that it has signed a definitive agreement to acquire Rhode Island-based skilled home healthcare provider Assisted Daily Living. The deal is expected to close by the end of the year, following regulatory approval by the state of Rhode Island. Read More
AccentCare, Memorial Hermann Health System To Combine Home Health, Hospice Operations in South Texas. Hospice News reported on April 3, 2023, that Texas-based AccentCare and Memorial Hermann Health System are forming a joint venture, combining their home health and hospice operations in south Texas. The new entity will be managed by AccentCare, a portfolio company of private equity firm Advent International. Read More
CVS Health, Oak Street Health Move Forward with Merger. Modern Healthcare reported on March 30, 2023, that CVS Health and Oak Street Health are moving ahead with their merger, after federal regulators allowed the antitrust waiting period to lapse without taking action. Oak Street Health will seek shareholder approval on April 28. Read More
CVS Health Completes Acquisition of Signify Health. CVS Health announced on March 29, 2023, that it completed its acquisition of Signify Health, a home health provider and technology company with a network of more than 10,000 clinicians nationwide. The transaction is valued at approximately $8 billion. Read More
UnitedHealth Group to Reduce Use of Prior Authorizations. Reuters reported on March 29, 2023, that UnitedHealth Group will reduce the use of prior authorizations by 20 percent for some non-urgent surgeries and procedures. The reductions will begin in the third quarter and continue through the rest of the year. They will impact commercial and Medicare Advantage, as well as some Medicaid beneficiaries. The company plans on implementing a program in 2024 that ends the need for prior authorization for most procedures. Read More
Venture Capital Firms Continue to Eye Investments in Medicaid. Forbes reported on March 28, 2023, that venture capital firms continue to eye investments in Medicaid, especially startups involved in patient engagement, preventive care, and the ability to take on risk in areas like behavioral health, substance use disorder, maternal care, and complex care. Read More
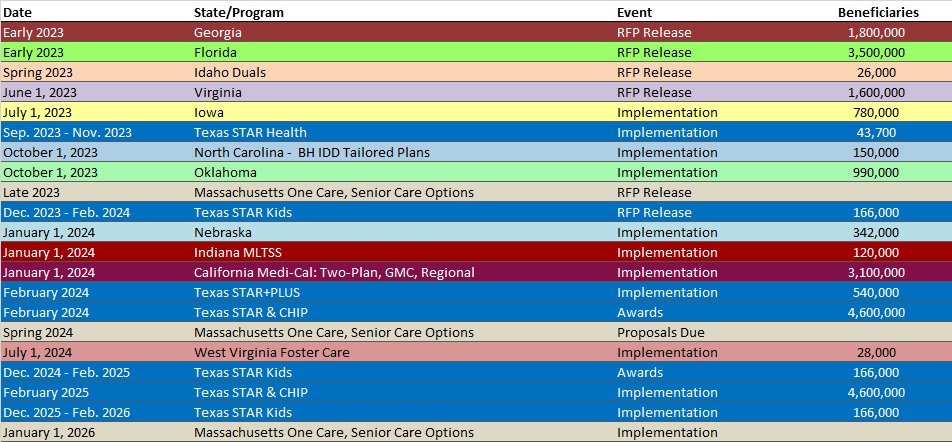
RFP Calendar
HMA News & Events
LEAVITT PARTNERS, AN HMA COMPANY, REPORT
Leavitt Partners Report Identifies Strategies to Improve Pharmacy Data Interoperability.
On April 4, 2023, Leavitt Partners, an HMA Company released a report outlining steps federal and state policymakers, technology and electronic health record (EHR) companies, health plans, pharmacies, and other healthcare providers can take to strengthen pharmacy data interoperability.
As patients access more services from pharmacies, the data interoperability of those pharmacies becomes increasingly important to patients and the healthcare system at-large. Pharmacy teams’ ability to provide optimal care and meaningfully contribute to the value-based care transformation depends on their ability to access and contribute to patients’ clinical records, just as hospitals, clinics, labs, and other providers need to know the information stored in pharmacies’ systems to appropriately serve their patients.
In “Supporting Pharmacy Data Interoperability: An Imperative for Patient Access and Outcomes,” Leavitt Partners shares findings from studying the progress made to improve data interoperability for pharmacies, as well as the remaining challenges. The report points out that important progress toward pharmacy data interoperability includes the use of clinical documentation systems, increased data sharing during the COVID-19 pandemic, state health information exchanges (HIEs), the Pharmacist eCare Plan, vaccination registries, prescription drug monitoring programs, and standardized data application programming interfaces (APIs). These are important tools, as recognized in the report, but were found to be insufficient and incomplete in their implementation.
Opportunities exist to address the current gaps and promote broader pharmacy data interoperability that elevates the effectiveness and efficiency of the healthcare system. The report’s recommendations relate to both policy and technology and center around three overarching themes: removing barriers to the provision of pharmacy-based clinical services; standardized, cost-effective, and clinically actionable data storage and sharing solutions; and collaboration across the healthcare ecosystem.
Download the report here.
Funding for this report was provided by the National Association of Chain Drug Stores (NACDS). None of the views or opinions expressed in the report are attributable to NACDS.
WAKELY, AN HMA COMPANY, WHITE PAPER
Identifying Medical Spend for Older Adults with Injurious Fall Related Claims- Lessons Learned. There have been significant challenges in the identification of fall related claims in Medicare data. Wakely partnered with Nymbl Science to design and deploy a new approach to assess claims for injurious falls that require medical care.
In this paper, we identify the limitations in identifying fall related claims, and present an analysis of the estimated cost impact of fall-related claims using a new model to identify fall-related claims. Read More
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- California Medicaid Managed Care Enrollment is Up 2.5%, Jan-23 Data
- Georgia Medicaid Managed Care Enrollment is Up 1.7%, Apr-23 Data
- Kentucky Medicaid Managed Care Enrollment is Up 1.2%, Feb-23 Data
- Louisiana Medicaid Managed Care Enrollment is Up 0.6%, Jan-23 Data
- Missouri Medicaid Managed Care Enrollment is Up 4.2%, Feb-23 Data
- Nebraska Medicaid Managed Care Enrollment Is Up 8.1%, Sep-22 Data
- Nebraska Medicaid Managed Care Enrollment Is Up 9%, Oct-22 Data
- Nevada Medicaid Managed Care Enrollment is Up 1%, Feb-23 Data
- New Jersey Medicaid Managed Care Enrollment is Up 0.5%, Jan-23 Data
- Wisconsin Medicaid Managed Care Enrollment is Up 0.6%, Jan-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Texas STAR, CHIP Managed Care RFP, Scoring, and Related Documents, 2022-23
- West Virginia Medicaid Specialized Managed Care for Children, Youth RFP and Scoring, 2022
Medicaid Program Reports, Data, and Updates:
- Colorado Prescription Drug Affordability Board Meeting Materials, 2021-23
- Connecticut Department of Social Services Annual Reports, 2012-22
- Maine Prescription Drug Affordability Board Meeting Materials, 2022-23
- Nebraska Medical Care Advisory Committee (MCAC) Meeting Materials, Feb-23
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.