HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- Florida Releases Medicaid Managed Care ITN

- Alabama House Committee Holds Meeting on Medicaid Expansion

- California to Seek Approval for Voluntary Medicaid Capitated Payment Model for FQHCs

- California Medi-Cal To Comply With Federal Law, Continue Business with Walgreens

- Delaware Struggles to Investigate Complaints Against Assisted Living, Nursing Facilities

- Georgia Proposes Using Directed Payments to Make Up for Financial Losses at Rural Hospitals

- Michigan to Release Medicaid Managed Care RFP in Fall 2023

- New Jersey Receives Approval for Medicaid Waiver on Coordinating Behavioral Health, Covering Social Needs

- New York Medicaid Audit Finds $184 Million in Uncollected Drug Rebates

- Oregon Medicaid Beneficiaries Struggle to Access Mental Health Care Despite Relatively High Medicaid Rates, Study Finds

- Pennsylvania Lawmakers Debate Medicaid Dental Benefits During Budget Hearing

- Texas Files Federal Lawsuit Over Medicaid Provider Tax Policy Change

- CMS Proposes 2.8 Percent Medicare Rate Increase for Hospitals that Meet Quality Reporting, Meaningful Use Standards

- Medicaid Enrollment to Settle At Higher Than Pre-Pandemic Levels in Many States, Analysis Finds

- Froedtert Health, ThedaCare to Merge

In Focus
Florida Releases Medicaid Managed Care ITN
This week our In Focus section reviews the Florida Statewide Medicaid Managed Care Program (SMMC) Invitation to Negotiate (ITN), released on April 11, 2023, by the Florida Agency for Health Care Administration (AHCA). SMMC consists of three programs: Managed Medical Assistance (MMA), Long-term Care (LTC), and dental, covering 4.4 million individuals. This ITN is for contracts to provide MMA and LTC.
Under the SMMC program, all enrollees receive their services from a single plan providing managed medical assistance, long-term care, and specialty benefits. (Dental benefits are provided separately.)
AHCA will select plans that will achieve the agency’s goals, including providing healthy birth outcomes for mothers and their infants, improving childhood and adolescent mental health, maximizing home and community-based placement and services, and supporting the HOPE Florida program. HOPE Florida utilizes ‘Hope Navigators’ to help individuals achieve economic self-sufficiency, develop long term-goals, and map out a strategic plan by focusing on community collaboration between the private sector, faith-based community, nonprofits and government entities.
Additionally, with the new contracts, AHCA will implement the following changes:
- Specialty plans will no longer be awarded separately but must be awarded to a comprehensive or MMA plan.
- Enrolling voluntary recipients (such as individuals with intellectual or developmental disabilities) into the SMMC program and providing the opportunity for them to opt out
- AHCA may mandatorily enroll into the MMA program full benefit dual-eligibles who are also in a Medicare Dual Eligible Special Needs Plan (DSNP).
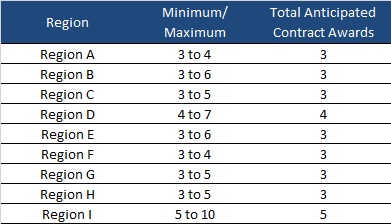
AHCA will invite 10 plans to negotiate for awards as shown below:
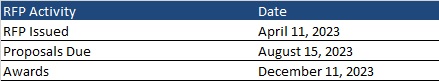
Timeline
Proposals are due August 15, 2023, with an anticipated award date of December 11. Contract will run from October 1, 2024, through December 31, 2030. Contracts may not be renewed, but AHCA may extend the term to cover any delays during the transition to a new plan.
Evaluation
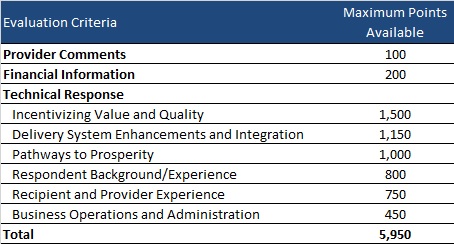
Plans can receive a total maximum number of points of 5,950. AHCA will invite top-ranking plans to negotiations to ensure that AHCA can enter into contracts with the minimum required number of plans per region.
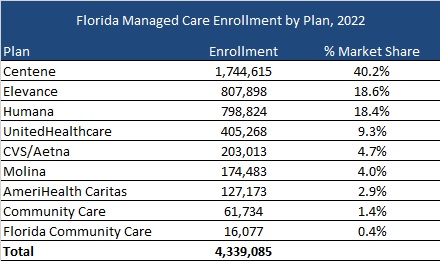
Current Market
As of December 2022, Florida served 4.3 million MMA and LTC enrollees, excluding an additional 97,000 Children’s Medical Services enrollees in the Children’s Medical Services Network plan. Centene had the highest market share based on enrollment, at over 40 percent.
HMA Roundup
Alabama
House Committee Holds Meeting on Medicaid Expansion. The Alabama Reflector reported on March 22, 2023, that the Alabama House Health Committee held a meeting on Medicaid expansion. The meeting, which was called “educational” by committee chair Rep. Paul Lee (R-Dothan), featured presentations by the Alabama Hospital Association and Blue Cross Blue Shield of Alabama. Read More
Arizona
Arizona Requests 1115 Waiver Amendment to Automatically Renew Medicaid Eligibility for Former Foster Care Individuals. The Centers for Medicare & Medicaid Services announced on April 12, 2023, that Arizona asked federal regulators to allow the state to automatically renew Medicaid eligibility for individuals 18 to 26 who were in the state’s foster care system. The request was made as an amendment titled Former Foster Youth Annual Automatic Renewal to the state’s 1115 waiver. If approved, the amendment would run through September 30, 2027. The federal public comment period will be open until May 12. Read More
Arizona Must Improve Health Care for Individuals in Carceral Settings, Judge Rules. The Associated Press reported on April 8, 2023, that a federal judge issued an injunction aimed at improving health care for individuals in carceral settings. The ruling calls for quicker follow-up appointments and diagnostic tests, patient confidentiality, having more experienced staff in supervisory roles, monitoring health care trends among patients, timely delivery of medications, and planning for when inmates transition back into society. Read More
California
California to Seek Approval for Voluntary Medicaid Capitated Payment Model for FQHCs. Healthcare Innovation reported on April 10, 2023, that California will seek federal approval for a voluntary Medicaid capitated payment model for federally qualified health centers (FQHCs). Implementation would be in January 1, 2024, through a state plan amendment expected to be submitted to federal regulators in late 2023. Oregon, Washington, and Colorado have developed similar models. Read More
Medi-Cal To Comply With Federal Law, Continue Business with Walgreens. Kaiser Health News reported on April 6, 2023, that California Governor Newsom said Medi-Cal, the state’s Medicaid program, will comply with federal law and continue to use Walgreens, after remarks that he is “done doing business” with the company. The remarks came after Walgreens said it would not provide abortion pills in 21 states. Medi-Cal would be in breach of federal Medicaid requirements that allow patients to fill prescriptions at any approved pharmacy if it were to no longer work with Walgreens. Read More
Delaware
Delaware Struggles to Investigate Complaints Against Assisted Living, Nursing Facilities. The Delaware News Journal reported on April 11, 2023, that the Delaware Division of Health Care Quality has investigated an average of 22 percent of complaints against assisted living facilities and 49 percent of complaints against nursing facilities from 2013-21, according to Delaware Online/News Journal. As of March 2023, the state had a backlog of almost 1,500 complaints against nursing and assisted living facilities. Read More
Delaware Health Care Expenditures Rose 11 Percent Per Capita in 2021. The Delaware Department of Health and Social Services (DHSS) released on April 6, 2023, its third annual Benchmark Trend Report, showing all payer total health care per capita spending rose 11.2 percent to $9,088. The report, which showed total expenditures of $9.1 billion in 2021, attributed the increase in part to normalized utilization trends following the COVID-19 pandemic. Read More
Georgia
Georgia Proposes Using Directed Payments to Make Up for Financial Losses at Rural Hospitals. Kaiser Health News reported on April 10, 2023, that the Georgia Department of Community Health is proposing using directed payments to make up for financial losses at rural hospitals. Georgia officials estimate that the state will net $1 billion in federal funds for hospitals and providers through the use of a directed payments program. Other states utilizing the program have brought in significant federal funds, including more than $6 billion in California in 2022 and more than $4 billion in Arizona from 2018 to 2022. Read More
Georgia Children on Medicaid Were Denied Psychotherapy Treatment, Report Says. The Associated Press reported on April 10, 2023, that Elevance Health/Amerigroup denied or partially denied more than 6,500 requests for psychotherapy for Georgia children covered by Medicaid from 2019 to 2022, according to the Atlanta Journal Constitution. The report found that many of the denied requests were for children in foster care. Read More
Iowa
Iowa Advocates Urge Legislators to Extend Postpartum Medicaid Coverage. The Gazette reported on April 9, 2023, that Iowa advocates are urging legislators to pass a bill to extend postpartum Medicaid coverage from 60 days to 12 months. Multiple bills have been filed during the current session, but none have advanced. Read More
Michigan
Michigan to Release Medicaid Managed Care RFP in Fall 2023. The Michigan Department of Health and Human Services announced on April 7, 2023, that it plans to release a request for proposals (RFP) for its Medicaid managed care program in fall 2023. The procurement will stress whole person health, giving kids a healthy start, health equity, operational excellence, and engaging members, families, and communities. Other areas of concern include integrating physical, behavioral and oral health, social determinants of health, and ensuring access. Read More
New Hampshire
New Hampshire House Passes Budget That Would Boost Medicaid Rates. The New Hampshire Bulletin reported on April 6, 2023, that the New Hampshire House passed a state budget that would increase Medicaid rates above what Governor Sununu and the House Finance Committee asked for. All providers except hospitals would receive an average three percent increase, with significant increases going to nursing homes and assisted-living facilities, community mental health centers, and agencies that provide care for substance use disorder. The budget now heads to the Senate. Read More
House Committee Hears Support for Permanent Medicaid Expansion Reauthorization Bill. The Conway Daily Sun reported on April 5, 2023, that the New Hampshire House Health and Human Services and Elderly Affairs Committee held a hearing on Senate Bill 263 to reauthorize Medicaid expansion permanently. Nearly all organizations, providers, and advocates testified in support of the bill. The House Finance Committee budget plan that is up for vote reauthorizes the program for only two years. Read More
New Jersey
New Jersey Receives Approval for Medicaid Waiver on Coordinating Behavioral Health, Covering Social Needs. NJ Spotlight News reported on April 10, 2023, that New Jersey received federal approval for a Medicaid waiver aimed at better coordinating behavioral health care and covering health-related social needs like housing, nutrition, and other supports. The changes will be rolled out over several years. Read More
New York
Medicaid Audit Finds $184 Million in Uncollected Drug Rebates. The Office of the New York State Comptroller reported on April 5, 2023, that the New York Department of Health (DOH) failed to collect a total of $183.7 million in available drug rebates under the federal Medicaid Drug Rebate Program, according to an audit of claims between April 2018 and March 2022. The largest portion, totaling $119 million, was due to errors in claims extraction procedures. The audit recommends that DOH invoice drug manufacturers to capture the missed rebates and improve its system to ensure claims include all necessary information. Read More
Oregon
Oregon Medicaid Beneficiaries Struggle to Access Mental Health Care Despite Relatively High Medicaid Rates, Study Finds. The Oregon Capital Chronicle reported on April 10, 2023, that despite relatively high mental health reimbursement rates, Medicaid beneficiaries in Oregon continue to struggle to access care, according to a recent Health Affairs study. The study found that administrative burdens on providers, high demand, and workforce shortages are hindering access. Read More
Pennsylvania
Lawmakers Debate Medicaid Dental Benefits During Budget Hearing. The Pittsburgh Post-Gazette reported on April 11, 2023, that Pennsylvania lawmakers debated whether to increase Medicaid dental benefits and raise dental reimbursements by eight percent during a House Appropriations Committee budget hearing. Pennsylvania had previously offered full dental benefits for adult Medicaid beneficiaries until 2011. Read More
Texas
Texas City Has Higher Uninsured Rate than Twin City in Arkansas. KERA News reported on April 10, 2023, that the uninsured rate in Texarkana — a city split in two by the Texas-Arkansas border — is 18 percent on the Texas side and 12 percent on the Arkansas side. Arkansas has implemented Medicaid expansion, while Texas has not. Read More
Texas Files Federal Lawsuit Over Medicaid Provider Tax Policy Change. Law360 reported on April 6, 2023, that Texas has filed a federal lawsuit arguing that the Centers for Medicare & Medicaid Services (CMS) improperly extended provider tax “hold harmless” provisions to private agreements between providers through an informational bulletin. The state argues the change will result in a costly administrative burden and may impact the amount of matching funds available to the state. Read More
Advocacy Group Points to Care Access Issues for Children with Complex Medical Conditions. State of Reform reported on April 6, 2023, that disparate Medicaid managed care policies and a lack of state capacity is impacting care for children with severe disabilities and complex medical conditions, according to a study commissioned by Protect Texas Fragile Kids (PTFK). PTFK supports legislation to create a pilot program providing comprehensive care to children with complex medical needs through an alternative payment model. Read More
Texas House Passes Bill to Use TANF, SNAP Eligibility Data for Enrolling Individuals in Medicaid, CHIP. The Herald Banner reported on April 6, 2023, that the Texas House passed the Express Lane Eligibility program (House Bill 1599), which would allow the Health and Human Services Commission to determine eligibility for Medicaid and Children’s Health Insurance Program (CHIP) using already-verified information from the Temporary Assistance for Needy Families (TANF) program, the Supplemental Nutrition Assistance Program (SNAP), and other programs. The bill is intended to increase efficiency across agencies and help get coverage to the 400,000 uninsured children who are eligible for Medicaid or CHIP but not enrolled. The bill now heads to the Senate for approval. Read More
West Virginia
West Virginia Adds $20 Million to Nursing Workforce Expansion Program. Williamson Daily News reported on April 10, 2023, that West Virginia will have $20 million in additional funding available for the state’s Nursing Workforce Expansion Program. The program, which is aimed at addressing the state’s nursing shortage, was included in the state budget approved in March. Read More
Wisconsin
Legislature Considers Bill Requiring Medicaid Eligibility Redeterminations Every Six Months. Wisconsin Public Radio reported on April 10, 2023, that the Wisconsin legislature is considering a bill (LRB 2171) that would require Medicaid beneficiaries to go through eligibility redeterminations every six months. Governor Tony Evers is unlikely to sign the bill if it passes. Read More
Medicaid Plan Expands Coverage to Additional Counties. WiscNews reported on April 6, 2023, that Group Health Cooperative of South Central Wisconsin expanded its Medicaid service area to Sauk, Columbia, Jefferson, Iowa, Grant, and Lafayette counties. Previously, it only served Medicaid enrollees in Dane County. Read More
National
CMS Proposes 2.8 Percent Medicare Rate Increase for Hospitals that Meet Quality Reporting, Meaningful Use Standards. Modern Healthcare reported on April 10, 2023, that the Centers for Medicare & Medicaid Services (CMS) proposed a 2.8 percent Medicare reimbursement rate increase for hospitals that comply with quality reporting rules and meaningful use of electronic health records. The increase is part of the hospital inpatient prospective payment system proposed rule that was published April 10. If you are interested in learning more about the IPPS rule, HMA will cover the topic in depth in our next In Focus article. You can also learn more by contacting Clare Mamerow at [email protected], Kevin Kirby at [email protected], Zach Gaumer at [email protected], or Amy Bassano at [email protected]. Read More
COVID-19 National Emergency Officially Ends; PHE to End May 11. CNN reported on April 10, 2023, that President Biden signed legislation ending the national emergency for COVID-19. The public health emergency is still scheduled to end on May 11. Read More
37 States Have Minimum MLR Requirements for Medicaid Managed Care Plans, KFF Finds. Kaiser Family Foundation (KFF) reported on April 10, 2023, that 37 of the 41 states with Medicaid managed care programs set minimum medical loss ratio (MLR) requirements, according to the KFF annual Medicaid budget survey. The survey also found that 28 states always require plans to pay remittances when the minimum MLR is not met, and 18 always include risk corridors in contracts. Read More
Health Plans to Cover Preventive Care Without Cost-Sharing Despite Judge’s Ruling. Modern Healthcare reported on April 10, 2023, managed care plans are likely to continue to cover preventive care without member cost-sharing, despite a federal judge’s ruling invalidating the Affordable Care Act mandate. Elevance Health, Kaiser Permanente, trade association AHIP, for example, released statements that preventive care without cost-sharing would continue. Read More
U.S. Representatives Reintroduce Legislation to Increase Reimbursement Rates for Rural Teaching Hospitals. The Pennsylvania Capital-Star reported on April 7, 2023, that U.S. Representatives Susan Wild (D-PA) and Dan Meuser (R-PA) reintroduced a bill to increase reimbursement rates for rural teaching hospitals. If signed into law, the bill would impact 14 hospitals across the country. Read More
Healthcare Employment Is Up 3.8 Percent in First Quarter of 2024. Modern Healthcare reported on April 7, 2023, healthcare employment was up 3.8 percent in the first quarter of 2024, compared to the same period a year prior, according to data from the Labor Department’s Bureau of Labor Statistics. While positions such as nursing, ambulatory care, and home care are in high demand, employers are actually trimming staff in other areas. Read More
Black Women Experience Poorer Maternal Outcomes Even in Least Vulnerable Counties, Study Finds. Fierce Healthcare reported on April 7, 2023, that Black women living in the least vulnerable areas of the U.S. are more likely to die or have worse birth outcomes compared to white women living in the most vulnerable areas, according to a recent study published in The Lancet. Federal data also showed that maternal mortality rates in the U.S. rose 40 percent in 2021, which is the highest rate in nearly 60 years. The study recommended locally informed health interventions and additional research into racism to achieve maternal health equity. Read More
State Medicaid Agencies to Rely on Consulting, Staffing, Technology Companies During Redeterminations. Modern Healthcare reported on April 6, 2023, that state Medicaid departments are signing contracts with consulting, staffing, and technology companies to aid with Medicaid redeterminations. Read More
Low Medicaid Rates May Be Leading to Evictions in Assisted Living Facilities. The Washington Post reported on April 6, 2023, that low Medicaid reimbursements, staffing shortages, and inflation are leading to evictions of Medicaid patients in assisted living facilities. State ombudsman programs for long-term care received 3,265 complaints in 2020 related to evictions from assisted-living facilities. According to assisted living facility trade association Argentum, private pay rates average $5,000 a month, while Medicaid is often about $3,000 a month. In Wisconsin, in the last few months, four facilities have canceled their Medicaid managed care contracts. Read More
MACPAC Meeting Is Scheduled for April 13-14. The Medicaid and CHIP Payment and Access Commission (MACPAC) announced on April 6, 2023, that its next meeting will be held on April 13-14. Among the topics for discussion will be policy options for automatic adjustments to disproportionate share hospital allotments, Medicare-Medicaid dual eligibles, Medicaid services for adults leaving incarceration, and the unwinding of continuous coverage requirements. Read More
CMS Finales Medicare Rule on Misleading Advertising, Improving Access to Affordable Drug Coverage. The Centers for Medicare & Medicaid Services (CMS) released on April 5, 2023, a final rule to strengthen Medicare. The rule will crack down on misleading marketing, improving access to affordable prescription drug coverage, removing barriers to care created by complex prior authorizations and utilization management, expanding access to behavioral health care, and promoting equitable care. Read More
Markets with High Medicare Advantage Penetration Have Lower Rates of Post-acute Care, Report Finds. Becker’s Payer Issues reported on April 5, 2023, that markets with high Medicare Advantage penetration have lower rates of post-acute care among all Medicare enrollees, according to a study in Health Affairs. The study looked at rates of post-acute care for congestive heart failure, hip fractures, and stroke from 2013-17 among enrollees in Medicare Advantage, traditional Medicare, and Medicare accountable care organizations. Read More
Medicaid Enrollment to Settle At Higher Than Pre-Pandemic Levels in Many States, Analysis Finds. Fierce Healthcare reported on April 4, 2023, that following the Medicaid redetermination process, 28 states will see Medicaid enrollment return to pre-pandemic or higher levels, according to an analysis by Moody’s Investors Service. The projection comes as enhanced federal Medicaid matching funds is phasing out. Read More
Industry News
Froedtert Health, ThedaCare to Merge. Fierce Healthcare reported on April 11, 2023, that Wisconsin-based Froedtert Health and ThedaCare have signed a letter of intent to merge, forming an 18-hospital system. They hope to complete the merger this year. Froedtert has 10 hospitals and 45 other care locations, while ThedaCare has eight hospitals and more than 180 care locations. Read More
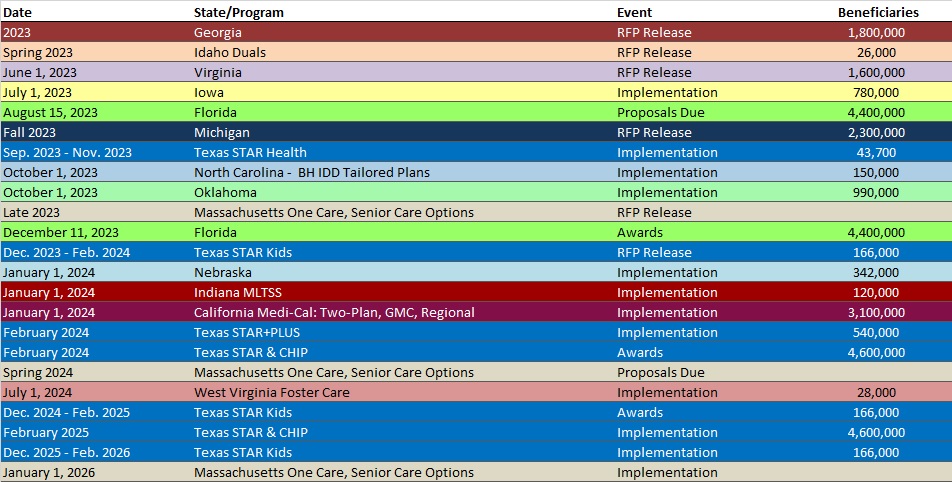
RFP Calendar
Company Announcements
MCG Announcements:
Implementers of the Nation’s First Successful Prior Auth Automation to Speak at HIMSS 2023. MCG Health, part of the Hearst Health network and an industry leader in evidence-based guidance and technology, announces its senior interoperability experts will join their counterparts from Regence and MultiCare Connected Care to present at the HIMSS Global Health Conference & Exhibition. The health IT innovators will discuss their recent success with automating prior authorization processes through newly developed technology and standards.
MCG’s Dr. William Rifkin to Speak at ACMA National Conference on the Management of Chest Pain Patients. MCG Health’s Dr. Rifkin will present the session, “Appropriate Evaluation and Management of Non-Low Risk Chest Pain Patients,” at the ACMA National Conference on Friday, April 21, 2023, from 3:30 p.m. to 4:30 p.m. ET. This session will focus on the importance of accurate risk stratification of patients presenting to the emergency department with possible acute coronary conditions.
HMA News & Events
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Illinois Medicaid Managed Care Enrollment is Flat, Feb-23 Data
- Illinois Dual Demo Enrollment is Down 5.3%, Feb-23 Data
- Mississippi Medicaid Managed Care Enrollment is Flat, Mar-23 Data
- Nebraska Medicaid Managed Care Enrollment Is Up 9.6%, Nov-22 Data
- Nebraska Medicaid Managed Care Enrollment Is Up 10.6%, 2022 Data
- Nebraska Medicaid Managed Care Enrollment Is Up 1.2%, Jan-23 Data
- Nebraska Medicaid Managed Care Enrollment Is Up 2.1%, Feb-23 Data
- Nebraska Medicaid Managed Care Enrollment Is Up 2.5%, Mar-23 Data
- New Mexico Medicaid Managed Care Enrollment is Up 0.7%, Feb-23 Data
- North Carolina Medicaid Managed Care Enrollment is Up 0.8%, Feb-23 Data
- Tennessee Medicaid Managed Care Enrollment is Up 0.8%, Jan-23 Data
- Virginia Medicaid Managed Care Enrollment is Up 2%, Feb-23 Data
- Virginia Medicaid MLTSS Enrollment is Up 0.7%, Feb-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- California Preadmission Screening and Resident Review (PASRR) Level II Evaluations IFB, Apr-23
- Florida Statewide Medicaid Managed Care (SMMC) Program ITN, Apr-23
- Minnesota Consultation Services to Mobile Crisis Responders for IDD, TBI, Co-occurring Mental Health Disorders RFP, Apr-23
- New Hampshire Medicaid System Evaluation RFP, Scoring, and Responses, 2022
- West Virginia Medicaid Specialized Managed Care for Children, Youth RFP, Proposal, and Scoring, 2022
Medicaid Program Reports, Data, and Updates:
- Arizona Quarterly Progress Reports for CMS, 2019-22
- Delaware Health Care Benchmark Trend Report for Calendar Year 2021, Apr-23
- Florida Medicaid Managed Care Data Book, Apr-23
- New York DOH Maximizing Drug Rebates Under the Federal Medicaid Drug Rebate Program Audit, Apr-23
- New York Medicaid Pharmacy Managed Care to FFS Transition Presentations, 2020-23
- Pennsylvania MLTSS Subcommittee Meeting Materials, 2021-23
- Texas HHS Presentations to Legislative Committees, Apr-23
- Texas Initiatives to Reduce Avoidable Emergency Room Utilization and Improve Health Outcomes in Medicaid Reports, 2022-23
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
