This week's roundup:
- In Focus: Oklahoma to Transition to Medicaid Managed Care
- Arizona Awards Contract to Provide Healthcare in State Prison System to NaphCare
- California to Apply for IMD Exclusion Waiver
- California Governor Proposes Alternative Payment Model for Federally Qualified Health Centers
- Montana Appoints Mike Randol as Medicaid Director
- North Carolina Senate Introduces Medicaid Expansion Bill with Work Requirements
- Pennsylvania Removes Collective Bargaining Language from Medicaid Managed Care Contracts
- CMS to Reduce 2023 Medicare Part B Premiums
- CMS Approves 12-Month Postpartum Medicaid Coverage in California, Florida, Kentucky, Oregon
- CareMax to Acquire Medicare Value-Based Care Business of Steward Health Care System
- Sun Life Financial Completes Acquisition of DentaQuest
In Focus
Oklahoma to Transition to Medicaid Managed Care
This week, our In Focus section reviews a new Oklahoma law to implement Medicaid managed care by October 1, 2023. The law, signed by Governor Kevin Stitt on May 26, 2022, requires the state to issue a request for proposals and to award at least three Medicaid managed care contracts to health plans or provider-led entities like accountable care organizations.
Provider-led entities would receive preferential treatment, with at least one targeted to receive a contract. However, if no provider-led entity submits a response, the state will not be required to contract with one.
Goals of the legislation include:
- Improve health outcomes for Medicaid members and the state as a whole;
- Ensure budget predictability through shared risk and accountability;
- Ensure access to care, quality measures, and member satisfaction;
- Ensure efficient and cost-effective administrative systems and structures; and
- Ensure a sustainable delivery system that is a provider-led effort and that is operated and managed by providers to the maximum extent possible.
Plans would provide physical health, behavioral health, and prescription drug services. Covered beneficiaries would include traditional Medicaid members and the state’s voter-approved expansion population, but not the aged, blind, and disabled population eligible for SoonerCare.
Plans will need to contract with at least one local Oklahoma provider organization for a model of care containing care coordination, care management, utilization management, disease management, network management, or another model of care as approved by OHCA.
Oklahoma will also issue separate RFPs for a Medicaid dental benefit manager plan and a Children’s Specialty plan.
Background
Oklahoma currently does not have a fully capitated, risk-based Medicaid managed care program. The majority of the state’s more than 1.2 million Medicaid members are in SoonerCare Choice, a Primary Care Case Management (PCCM) program in which each member has a medical home. Other programs include SoonerCare Traditional (Medicaid fee-for-service), SoonerPlan (a limited benefit family planning program), and Insure Oklahoma (a premium assistance program for low-income people whose employers offer health insurance). Prior efforts to transition to Medicaid managed care have encountered roadblocks, starting in 2017 with a failed attempt to move aged, blind, and disabled members to managed care.
More recently, in June 2021, the Oklahoma Supreme Court struck down a planned transition of the state’s traditional Medicaid program to managed care, ruling that the Oklahoma Health Care Authority does not have the authority to implement the program without legislative approval.
Contracts had been awarded to Blue Cross Blue Shield of Oklahoma, Humana, Centene/Oklahoma Complete Health, and UnitedHealthcare. Centene/Oklahoma Complete Health also won an award for the SoonerSelect Specialty Children’s Health Plan program, covering foster children, juvenile justice-involved individuals, and children either in foster care or receiving adoption assistance.
Link to Senate Bill 1337
HMA Roundup
Arizona
Arizona Awards Contract to Provide Healthcare in State Prison System to NaphCare. Health Payer Specialist reported on May 31, 2022, that Arizona awarded a contract to provide healthcare for the state’s prison system to Alabama-based NaphCare. NaphCare will provide physician and nursing services, mental health services, and psychiatric care to inmates in state custody at 10 Arizona State Prison Complexes. Centene subsidiary Centurion health previously held the contract. Read More
Arizona Has Not Addressed Nursing Home Care Improvements, Audit Finds. Fronteras reported on May 25, 2022, that the Arizona Department of Health Services (DHS) has not addressed recommendations made in a 2019 report from the Arizona Auditor General’s office to improve nursing home care, according to a recent follow-up audit. The audit also found that DHS closed multiple high priority complaints without a required onsite investigation. Read More
California
California to Apply for IMD Exclusion Waiver. The Santa Monica Daily Press reported on May 28, 2022, that the California Department of Health is in the process of applying for an Institution of Mental Disease (IMD) exclusion waiver from the Centers for Medicare & Medicaid Services to allow for Medicaid coverage at mental health care inpatient facilities with more than 16 beds. The Los Angeles County Department of Mental Health is working to repeal the IMD Medicaid exclusion at the federal level. Read More
Governor Proposes Alternative Payment Model for Federally Qualified Health Centers. Healthcare Innovation reported on May 26, 2022, that California Governor Gavin Newsom proposed a pilot program to implement an alternative payment model for Federally Qualified Health Centers (FQHCs). The proposal, included in the Governor’s fiscal 2023 budget, would replace the volume-based prospective payment system for FQHCs with an upfront, clinic-specific capitation rate in order to incentivize delivery system and practice transformation. The program, if passed, would be implemented no earlier than January 2024. Read More
Illinois
Illinois Enacts Automatic Medicaid Renewal, Continuous Coverage Provisions. Illinois Senate Democrats announced on May 31, 2022, that Governor J. B. Pritzker signed legislation that allows for continuous Medicaid coverage without requiring individuals to report changes in income on a monthly basis. The law also allows for Medicaid coverage to be automatically renewed for individuals with zero income. Medicaid coverage will be extended to include midwife services and funding for dental care and non-emergency medical transportation. Read More
Louisiana
Louisiana Seeks Federal Approval to Continue OUD/SUD 1115 Waiver Demonstration. The Centers for Medicare & Medicaid Services (CMS) announced on May 26, 2022, that Louisiana is seeking approval to continue administering the Healthy Louisiana Opioid Use Disorder/Substance Use Disorder (OUD/SUD) section 1115 waiver demonstration with no changes. Public comments will be accepted through June 24, 2022. Read More
Missouri
Missouri Plan Appoints Jeff Johnston as Plan President, CEO. Centene’s Missouri-based Home State Health Plan announced on May 31, 2022, that Jeff Johnston has been appointed as plan president and chief executive officer. Previously, Johnston served as the executive vice president of community operations at Mercy Health. Johnston will oversee the organization’s Medicaid, Medicare, and Exchange plans. Read More
Missouri Stalls Legislation to Extend Postpartum Care for Women with SUD. The Missouri Independent reported on May 26, 2022, that Missouri lawmakers paused the implementation of a bill passed in 2018 to extend postpartum care for women with substance use disorders (SUD) from 60 days to a full year. Funding for full postpartum benefits was also removed from the final budget version passed by lawmakers. The Missouri Department of Social Services (DSS) “plans to regroup” with the Centers for Medicare & Medicaid Services (CMS) on waiver options to provide more comprehensive postpartum Medicaid coverage, according to a DSS spokeswoman. Read More
Montana
Montana Appoints Mike Randol as Medicaid Director. Kaiser Health News reported on June 1, 2022, that Mike Randol has been appointed Montana’s Medicaid director, effective May 31. Previously, Randol was an executive with Cerner Corp. and also served as Medicaid director for two Medicaid managed care states: Iowa and Kansas. Montana, which is not a Medicaid managed care state, has about 280,000 Medicaid members. Read More
North Carolina
Senate Introduces Medicaid Expansion Bill with Work Requirements. North Carolina Health News reported on May 26, 2022, that the North Carolina Senate introduced a bill (HB 149) to expand Medicaid to approximately 600,000 adults. The bill includes a provision for work requirements, which has been struck down in other states. Under the bill, the state would have the option to end expansion if the federal government reduces its 90 percent share of funding. A number of other health care provisions are included in the bill, such as increased telehealth options, privileges for advanced practice nurses to practice without physician supervision, and changes to certificate of need statutes. Leaders in the state House have indicated they may not take up the bill during the current session. Read More
Pennsylvania
Pennsylvania Removes Collective Bargaining Language from Medicaid Managed Care Contracts. The Center Square reported on May 31, 2022, that the Pennsylvania Department of Human Services removed language from its proposed HealthChoices Medicaid managed care contracts that would have prevented non-unionized providers that had work stoppages in the last five years from inclusion in managed care networks. The contracts are set to be implemented on September 1. Read More
National
Federally Qualified Health Centers At-Risk of Funding Loss when PHE Ends. Modern Healthcare reported on May 26, 2022, that federally qualified health centers (FQHCs) are likely to lose funding when the federal public health emergency (PHE) is lifted. FQHCs must care for patients regardless of ability to pay and as many as 16 million individuals nationally may lose Medicaid coverage due to redeterminations. Additionally, the Community Health Center Fund, which provides federal grants to FQHCs, expires in 2023. Congress is expected to renew the funding, but the health centers are unsure how much will be allocated. Read More
HHS Withdraws SUNSET Rule. Modern Healthcare reported on May 26, 2022, that the U.S. Health and Human Services Department (HHS) withdrew the SUNSET rule, which would have required nearly all HHS regulations to be reviewed for economic impact after 10 years and automatically eliminated if not reviewed within that time frame. The SUNSET rule was initiated during the Trump administration. Previously, HHS postponed implementation of the rule until September 2022. Read More
Bipartisan Senate Group Proposes Telehealth Mental Health Care Bill. Modern Healthcare reported on May 26, 2022, that a group of bipartisan leaders from the Senate Finance Committee proposed a draft of the Telemental Health Access to Care Act to strengthen access to and support for telehealth services for mental health care. The bill would also eliminate the Medicare in-person visit requirement. Read More
CMS Race and Ethnicity Data from 22 States Unusable, of High Concern, Study Finds. EHR Intelligence reported on May 26, 2022, that race and ethnicity data reported to the Centers for Medicare & Medicaid Services (CMS) was unusable or of high concern in 22 states, according to a study from Health Affairs. Race and ethnicity data from the Transformed Medicaid Statistical Information System (T-MSIS) Analytic Files (TAF) was missing for more than 10 percent of enrollees in most states. Data was of low concern in 15 states. Read More
CMS to Reduce 2023 Medicare Part B Premiums. The Associated Press reported on May 27, 2022, that U.S. Health and Human Services Secretary Xavier Becerra announced a reduction in Medicare Part B premiums in 2023 after a new Alzheimer’s drug Aduhelm cost was halved. The Centers for Medicare & Medicaid Services increased Part B premiums by $22 per month in 2022, in part to cover the drug. Read More
CMS Approves 12-Month Postpartum Medicaid Coverage in California, Florida, Kentucky, Oregon. The Centers for Medicare & Medicaid Services (CMS) announced on May 25, 2022, that California, Florida, Kentucky, and Oregon are approved to expand postpartum Medicaid coverage to 12 months to cover a total of 126,000 additional families. California, Kentucky, and Oregon have implemented new state plan amendments through the American Rescue Plan Act, while Florida will offer coverage through a section 1115 waiver demonstration. Read More
Industry News
CareMax to Acquire Medicare Value-Based Care Business of Steward Health Care System in $135 Million Deal. Publicly traded CareMax announced on June 1, 2022, an agreement to acquire the Medicare value-based care business of Steward Health Care System for $135 million in cash and stock. CareMax will manage 170,000 Steward patients, including 50,000 in Medicare Advantage, 112,000 in the Medicare Shared Savings Program patients, and 9,000 through Direct Contracting. The deal will add $1.6 billion to $1.7 billion in annual revenues to CareMax. Including the potential for an additional earnout of CareMax shares, Steward would own 41 percent of CareMax class A common stock. Read More
Sun Life Financial Completes Acquisition of DentaQuest. Financial services company Sun Life Financial announced on June 1, 2022, the acquisition of DentaQuest, a dental plan serving more than 33 million members in 36 states. Sun Life acquired DentaQuest from CareQuest Institute for Oral Health and Centerbridge Partners. Read More
The Stepping Stones Group Acquires HM Therapy. The Stepping Stones Group announced on May 31, 2022, the acquisition of HM Therapy, a therapeutic and behavioral company for children in home and community based settings. The Stepping Stones Group provides therapeutic, behavioral, autism, nursing, and educational services to children in school, home, and community settings. Read More
Trinity Health at Home Acquires Above & Beyond Home Health Care. Hospice News reported on May 26, 2022, that Trinity Health at Home acquired Above & Beyond Home Health Care, an Iowa-based home health and hospice provider. Trinity Health at Home, a branch of the Trinity Health system, serves roughly 45,000 patients annually in 13 states. Read More
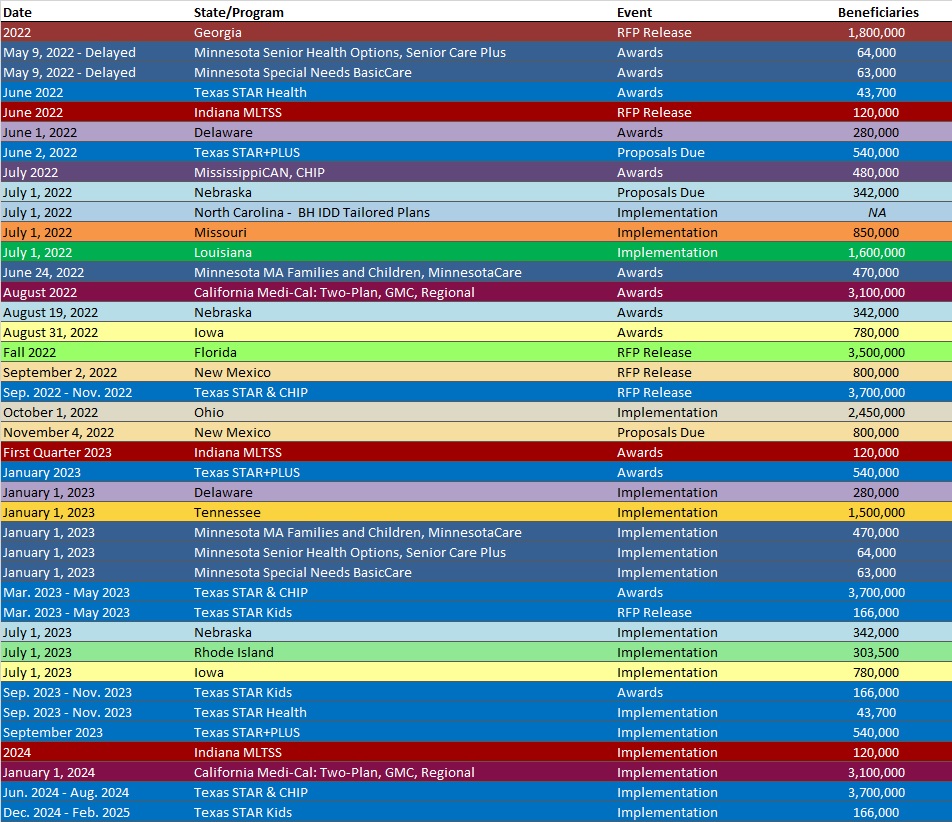
RFP Calendar
HMA News & Events
Medicaid Plans, Providers, States to Address Health Equity at HMA Conference in Chicago, October 10-11
HMA will host a breakout session on health equity at the fifth annual HMA conference, October 10-11, 2022, at the Fairmont Chicago, Millennium Park. Top executives from Medicaid managed care plans, state Medicaid departments, provider organizations, and other stakeholders will discuss how they are responding to emerging requirements and demands aimed at making health equity a key component of overall quality efforts. To register visit https://conference.healthmanagement.com/.
Confirmed speakers to date include (in alphabetical order):
The Role of Health Plans, Providers, and States in Addressing Health Equity
Kody Kinsley, Secretary, North Carolina Department of Health and Human Services
Andrew Martin, National Director of Business Development (Housing+Health), UnitedHealth Group
Joshua Traylor, Senior Director, Health Care Transformation Task Force
Shannon Wilson, VP, Population Health & Health Equity, Priority Health; Executive Director, Total Health Care Foundation
Keynote Q&A: Key Strategies, Opportunities, and Concerns for Medicaid Managed Care
John Barger, National VP, Dual Eligible and Medicaid Programs, Humana, Inc.
Aimee Dailey, President, Medicaid, Anthem, Inc.
Rebecca Engelman, EVP, Medicaid Markets, AmeriHealth Caritas
Brent Layton, President, COO, Centene Corporation
Kelly Munson, President, Aetna Medicaid
Timothy Spilker, CEO, UnitedHealthcare Community & State
Keynote Q&A: State Medicaid Priorities, Challenges – Now and After the Public Health Emergency
Jacey Cooper, Medicaid Director, Chief Deputy Director, California Department of Health Care Services
Allison Matters Taylor, Medicaid Director, Indiana
Dave Richard, Deputy Secretary, North Carolina Medicaid
Jami Snyder, Director, Arizona Health Care Cost Containment System
Keynote Address: Politics and the ‘New Normal’ for U.S. Healthcare
Drew Altman, President and CEO, Kaiser Family Foundation
Featured Speakers
Michael Brodsky, MD, Medical Director, Behavioral Health and Social Services, L.A. Care Health Plan
Cindy Cota, Director of Managed Medicaid Growth and Innovation, Volunteers of America
Daniel Elliott, MD, Medical Director, Christiana Care Quality Partners, eBrightHealth ACO, ChristianaCare Health System
Rebecca Engelman, EVP, Medicaid Markets, AmeriHealth Caritas
Martin Lupinetti, President, CEO, HealthShare Exchange (HSX)
Todd Rogow, President, CEO, Healthix
Debra Sanchez-Torres, Senior Advisor, Centers for Disease Control and Prevention
Mark Sasvary, Chief Clinical Officer, CBHS, IPA, LLC
Jim Sinkoff, Deputy Executive Officer, CFO, SunRiver Health
Tim Skeen, Senior Corporate VP, CIO, Sentara Healthcare
Courtnay Thompson, Market President, Select Health of SC, an AmeriHealth Caritas Company
Amanda Van Vleet, Associate Director, Innovation, NC Medicaid Strategy Office, North Carolina Department of Health & Human Services
The overall theme of this year’s conference is How Medicaid, Medicare, and Other Publicly Sponsored Programs Are Shaping the Future of Healthcare in a Time of Crisis. HMA will also host a pre-conference workshop on Sunday, October 9, on important trends and developments in value-based care.
HMA’s last national conference brought together 500 executives from health plans, providers, state and federal government, community-based organizations and others serving Medicaid, Medicare, and other vulnerable populations. Sponsorships and group discounts are available. For additional information, contact Carl Mercurio, cmercurio@healthmanagement.com.
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Minnesota CCBHC Outreach Efforts to Address COVID-related Impacts That Prevent Individuals from Accessing Integrated Mental Health and SUD Services RFP, May-22
- Nebraska Medicare Advantage Dual Special Needs Plan Contracts, CY 2022
- North Dakota Project Manager for Unwinding of Medicaid Eligibility at the End of the PHE RFP, May-22
Medicaid Program Reports, Data and Updates:
- Arizona DHS Long-Term Care Audit, May-22
- Indiana MLTSS Report to the Indiana General Assembly, Feb-22
- Indiana MLTSS RFI Co-Design Meeting Materials, Apr-22
- Iowa External Quality Review Technical Report, CY 2016-21
- Kansas Medical Care Advisory Committee Meetings, 2019-21
- Massachusetts Health Safety Net Annual Reports, 2015-20
- North Dakota Medicaid Expansion Program Annual Technical Reports, 2017-21
- Ohio Medical Care Advisory Committee Meeting Materials, 2019-21, May-22
- Pennsylvania Medical Assistance Advisory Committee (MAAC) Meeting Materials, May-22
- Vermont EQRO Annual Technical Reports, 2015-22
- Washington Medicaid Managed Care Comparative Analysis HEDIS Reports, 2013-20
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.