HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Low-Cost Carriers in ACA: Insights from the 2018-2021 Market Experience

- Alaska Releases Behavioral Health Information Management System RFI

- Delaware Releases Proposed 1115 Waiver Amendment

- Florida Can Recoup Medicaid Payments in Personal Injury Case, Supreme Court Rules

- Florida to Begin Medicaid Managed Care Procurement as Early as October 2022

- Florida Delays Award Announcements for Modular MMIS Vendors

- Georgia Releases Medicaid Managed Care RFI

- Illinois Increases Medicaid Funding for Nursing Homes by $700 Million

- Missouri Is Still Processing Medicaid Expansion Applications Slower than Federal Law Allows

- North Carolina Senate Gives Initial Approval to Medicaid Expansion Bill

- Oregon Medicaid CCO Completes Corrective Action Plan

- South Dakota Voters Deal Blow to Opponents of Medicaid Expansion

- Tennessee Issues RFI for Roadmap to Improve Oversight, Planning of D-SNPs

- FTC to Begin Inquiry Into PBM Practices

- Health Plans to Issue $1 Billion in MLR Rebates in 2022, KFF Projects

- Medical Transportation Management to Acquire Veyo

- UnitedHealth’s Optum Acquires Healthcare Associates of Texas

In Focus
Low-Cost Carriers in ACA: Insights from the 2018-2021 Market Experience
This week, our In Focus highlights a white paper from Wakely, an HMA Company, exploring the potential design elements and expected effects of a public option or a low-cost plan being newly introduced in the Affordable Care Act (ACA) individual market.
1332 state innovation waivers have been in place for a number of years and allow states to implement programs that increase access to and the affordability of healthcare coverage, subject to approval by the Department of Health and Human Services (HHS) and Department of Treasury (Treasury). Nearly all waiver programs in effect in 2021 employ a reinsurance program aimed at reducing the overall claim costs and premiums for members by reimbursing issuers for a portion of claim costs over a specified threshold.
A number of states have been exploring other ways to structure a waiver program, including introducing a public option plan into ACA markets (individual and small group plans subject to the ACA market reforms). The definition of a “public option plan” has evolved over time and can vary, but more commonly refers to a privately funded health plan with some level of government oversight or additional requirements established to improve consumer value and facilitate cost containment.
A public option plan aims to further increase access to coverage and affordability by offering a new qualified health plan, typically with a lower premium relative to existing premiums in the market. A public option plan specifically aims to extend a more affordable coverage to individuals who are currently not eligible for ACA subsidies (e.g., family glitch, non-citizens, and those with higher incomes). The plan could be structured in a variety of ways such as a state-sponsored product, state employee health plan buy-in, Medicaid plan buy-in, or a private plan offered by existing issuers. Colorado and Washington will require health plans to offer public option plans with a target premium reduction relative to other plans in the market, with constrained rate increases over time, giving health plans the opportunity to arrive at the lower premiums through their own means, for the 2023 plan year. Lower premiums would likely be achieved through a combination of lower provider reimbursement and lower risk margins.
Given the nature of premium subsidization in the individual ACA market, where premium subsidies are tied to the second lowest cost silver (SLCS) plan in the market, the introduction of a lower cost public option plan has a mixed impact on market growth and the types of member segments that benefit. Since Washington State is the only Exchange that currently offers a public option plan, there is minimal experience available to understand the impact a public option plan may have on the market. As a result, our goal was to look at states where a new issuer has entered a market as a low-cost plan over the last four years, to better understand plan enrollment migration (how many members switch to the low-cost carrier), competitors’ reactions, and the reduction in premium needed to incentivize members to take up coverage. This market dynamic potentially closely mimics a public option plan that offers lower premiums being introduced in a market. Over the last four years (2018-2021), we identified 51 instances of new issuers entering an individual on-Exchange market. Of those 51 new entrances, 25 met our criteria of a low-cost plan.
The analysis showed mixed impacts of a low-cost plan introduction in ACA markets, with minimal impact on the uninsured, but with improved affordability, particularly for the unsubsidized. The detailed observations are discussed further in this paper.
Please contact Ksenia Whittal at [email protected] with any questions.
HMA Roundup
Alaska
Alaska Releases Behavioral Health Information Management System RFI. The Alaska Department of Health and Social Services released on June 1, 2022, a request for information (RFI) for a comprehensive behavioral health Medicaid billing and clinical documentation information management system. The state Division of Behavioral Health currently uses the Alaska Automated Information Management System as its primary behavioral health information technology and data management system, which was developed in 2004. Responses are due on June 22.
California
California Exchange, Medicaid Members Are Mistakenly Bounced Between Programs. Kaiser Health News reported on June 2, 2022, that California Exchange and Medicaid members have been mistakenly bounced between programs due to computer glitches and human error. In one example, 131,000 enrollees were mistakenly dropped from coverage over several months in 2020; they were eventually reinstated. State officials have been working to eliminate errors that lead to loss of coverage. Read More
Colorado
Colorado Expands Medicaid to Pregnant, Postpartum Undocumented Women, Children. CPR News reported on June 7, 2022, that Colorado Governor Jared Polis signed legislation to expand Medicaid and Children’s Health Insurance Plan (CHIP) coverage to undocumented pregnant or postpartum women and their children for one year beginning in 2025. Medicaid and CHIP enrollees will have access to lactation supplies and support services. Read More
Delaware
Delaware Releases Proposed 1115 Waiver Amendment. The Delaware Division of Medicaid and Medical Assistance (DMMA) released on May 11, 2022, a draft of an 1115 waiver amendment to add five services to the Diamond State Health Plan, the state’s Medicaid managed care program. The amendment would incorporate into managed care home visits for pregnant women and children under the age of two; home-delivered meals; a pediatric respite benefit; a nursing home transition program (formerly Money Follows the Person Demonstration); and a self-directed state plan personal care option. DMMA is accepting public comments through June 10, 2022. Read More
Florida
Florida Can Recoup Past, Future Medicaid Payments in Personal Injury Case, Supreme Court Rules. CQ News reported on June 6, 2022, that the U.S. Supreme Court ruled that Florida can recoup $300,000 in past and future Medicaid costs out of an $800,000 settlement in the case of a child injured in an accident. The initial settlement allocated $35,000 for past medical care, but the court ruled 7-2 that the state was entitled to 37.5 percent of the settlement as allowed under state law. Read More
Florida to Begin Medicaid Managed Care Procurement as Early as October 2022. Florida Politics reported on June 4, 2022, that the Florida Agency for Health Care Administration (AHCA) is preparing to rebid the state’s Medicaid managed care contracts, which expire on December 31, 2023. The procurement process could begin at early as October 2022. AHCA received 54 responses to its recent managed care request for information from insurance companies, providers, hospital and health care associations, and advocacy groups. Read More
Florida Delays Award Announcements for Modular MMIS Vendors. Florida Politics reported on June 1, 2022, that Florida has delayed contract award announcements until the end of this month for two modules of the Florida Health Care Connections Medicaid information technology initiative: provider services and unified operations center. The contracts are set to run from September 1, 2022, to August 31, 2029, and are part of the state’s move to a modular Medicaid managed information system (MMIS). Read More
Georgia
Georgia Releases Medicaid Managed Care RFI. The Georgia Department of Community Health released on June 3, 2022, a request for information (RFI) on the reprocurement of the state’s Medicaid managed care program, including Georgia Families, the state’s traditional Medicaid and Children’s Health Insurance Program, and Georgia Families 360, which covers youths in foster care. Responses are due on June 24. Current contract holders are Anthem, CareSource, and Centene, serving more than 1.9 million beneficiaries as of May 2022. Existing contracts run through June 30, 2024. The request for proposals is expected to be released in late 2022 or early 2023. Read More
Georgia Board of Community Health Approves Extending Postpartum Medicaid Coverage to One Year. Capitol Beat News Service reported on June 2, 2022, that the Georgia Board of Community Health voted to seek federal approval to extend postpartum Medicaid coverage to one year effective October 31. Governor Brian Kemp signed the postpartum legislation in May. Read More
Illinois
Illinois Increases Medicaid Funding for Nursing Homes by $700 Million. McKnights Long-Term Care News reported on June 2, 2022, that Illinois Governor J.B. Pritzker signed legislation to increase annual Medicaid funding for nursing homes by $700 million or about 28 percent. Increases will be tied to star ratings and federal staffing guidelines. Read More
Missouri
Missouri Is Still Processing Medicaid Expansion Applications Slower than Federal Law Allows. The Missouri Independent reported on June 3, 2022, that the Missouri Department of Social Services took an average of 101 days to process a Medicaid expansion application in April, compared to the 45-day maximum allowed by federal law. According to Kim Evans, director of the Missouri Family Support Division, the state will be processing applications in under 45 days by the end of July and in 30 days by the end of August. There are currently 58,000 pending applications. Read More
North Carolina
Senate Gives Initial Approval to Medicaid Expansion Bill. The Associated Press reported on June 1, 2022, that the North Carolina Senate gave initial approval to a bill (HB 149) to expand Medicaid to approximately 600,000 adults. The bill includes a provision for work requirements, which has been struck down in other states. A number of other health care provisions are included in the bill, such as increased telehealth options, allowing advanced practice nurses to practice without physician supervision, and changes to certificate of need statutes. The Senate is expected to take a final vote soon before the bill moves to the House. House leaders have indicated they will not take up the bill during the current session. Read More
Ohio
House Passes Medicaid Coverage of Doula Services Legislation. The Statehouse News Bureau reported on June 6, 2022, that the Ohio House passed legislation to allow Medicaid to cover doula services. The bill now moves to the Senate. Ohio joins 17 other states that have implemented or are considering Medicaid coverage for doulas, according to an analysis by the Georgetown Center for Children and Families. Read More
Oregon
Oregon Medicaid CCO Completes Corrective Action Plan. The Oregon Health Authority announced on June 2, 2022, that Centene/Trillium Community Health Plan has completed a corrective action plan (CAP) concerning its expansion into the Tri-County, OR, service area. The CAP focused on network development, health equity, language access, community engagement, and intensive care coordination. Trillium is an Oregon Coordinated Care Organization (CCO), serving more than 50,000 members. Read More
Pennsylvania
House to Consider Legislation to Increase Medicaid EMS Reimbursement Rates. Fox 43 reported on June 2, 2022, that Pennsylvania Representative Martin Causer (R-Bradford) introduced legislation to increase Medicaid reimbursements for emergency medical services (EMS). Additionally, the bill proposes a 10 percent premium for “super rural” areas, as designated by the Centers for Medicare & Medicaid Services, and increased reimbursements based on mileage. The bill was passed by the Committee of Veterans Affairs and Emergency Preparedness and will be considered by the House. Read More
South Dakota
South Dakota Voters Deal Blow to Opponents of Medicaid Expansion. Forbes reported on June 8, 2022, that South Dakota voters rejected a proposed state constitutional amendment, which would have required a 60 percent supermajority to pass ballot measures, including Medicaid expansion. South Dakotans will vote on Medicaid expansion in November. Read More
Tennessee
Tennessee Issues RFI for Roadmap to Improve Oversight, Planning of D-SNPs. Open Minds reported on June 1, 2022, that Tennessee released a request for information (RFI) to help create an oversight and planning roadmap to improve programs for dual eligibles in the state’s Dual Special Needs Plans (D-SNPs). The state has contracts with three Medicaid managed care plans to operate aligned D-SNPs. Read More
Texas
Texas Announces Draft Policies for Telehealth Open for Public Comment. The Texas Health and Human Services Commission (HHSC) announced on June 6, 2022, draft policy changes concerning covered services using telemedicine, telehealth, and audio-only delivery if clinically appropriate and cost effective. HHSC has also drafted behavioral health service policy changes to allow non-local mental health authorities to deliver mental health targeted case management and mental health rehabilitation services to persons in fee-for-service Medicaid. The policy changes, which are in line with newly passed state laws, are open for public comment.
National
CMS Looks to Streamline Process for Individuals Moving Between Different Types of Coverage. CNBC reported on June 8, 2022, that the Centers for Medicare & Medicaid Services (CMS) wants to streamline the process for individuals moving between different types of coverage based on eligibility, according to administrator Chiquita Brooks-Lasure. With the public health emergency ending soon, there will be an estimated five million to 14 million individuals disenrolled who will need assistance transitioning to Exchange plans or Medicare or re-enrolling in Medicaid. Read More
FTC to Begin Inquiry Into PBM Practices. Modern Healthcare reported on June 7, 2022, that the Federal Trade Commission (FTC) will begin an inquiry into how vertical integration in the pharmacy benefit management (PBM) sector affects prescription drug access and pricing. The FTC will require the six largest PBMs, which control about 80 percent of the market, to provide information on their practices. The inquiry will look into clawbacks, efforts to direct patients to PBM-owned pharmacies, prior authorization policies, and the impact of manufacturer rebates. Read More
MACPAC Issues Brief on LGBT Medicaid Beneficiaries Accessing Care. The Medicaid and CHIP Payment and Access Commission (MACPAC) issued a brief in June 2022, which found that the majority of lesbian, gay, and bisexual (LGB) adults on Medicaid had a usual source of care and similar rates of physical health care service use as heterosexual adults on Medicaid. However, LGB adults were significantly more likely to report not having received necessary behavioral health or alcohol and drug treatment in the past 12 months. Medicaid-covered transgender and gender-diverse (TGD) adults reported similar rates of access to providers for both routine and most gender-affirming health care as those covered by private insurance, but those covered by Medicaid were more likely to report not being able to find in-network providers for gender affirming surgery. There are about 1.2 million lesbian, gay, bisexual, and transgender (LGBT) adults on Medicaid. Read More
CMS Launches National Quality Strategy Initiative. The Centers for Medicare & Medicaid Services (CMS) announced on June 6, 2022, the launch of a long-term national quality strategy aimed at improving outcomes through person-centric care in Medicare, Medicare Advantage, Medicaid, the Children’s Health Insurance Program, and Exchange plans. Goals include advancing health equity, promoting safety, embracing the digital age, fostering engagement, and increasing alignment across programs, performance metrics, and policies. CMS will begin stakeholder collaboration sessions on the strategy in summer 2022. Read More
FTC Moves to Block Hospital System Mergers in New Jersey, Utah, Citing Antitrust Concerns. Fierce Healthcare reported on June 3, 2022, that the Federal Trade Commission took action to block the merger of Utah healthcare systems HCA Healthcare and Steward Health Care as well as the acquisition of Saint Peter’s Healthcare System by New Jersey-based RWJBarnabas Health, citing antitrust concerns. Administrative trials are set to begin in late 2022. Read More
Community Health Centers Are Poised to Help Patients With Medicaid Redeterminations. Kaiser Family Foundation (KFF) reported on June 3, 2022, that most community health centers are poised to help patients maintain their Medicaid coverage after the public health emergency ends, according to a KFF survey. Nearly half of community health center patients are covered by Medicaid. Read More
HHS Announces One-Year Extension to Medicaid HCBS ARPA Spending Deadline. The U.S. Department of Health and Human Services (HHS) announced on June 3, 2022, that it has extended the deadline to spend funding from the American Rescue Plan Act (ARPA) by one year to March 31, 2025. The funding is to be used for activities to enhance, expand, or strengthen home and community-based services (HCBS) for Medicaid beneficiaries who need long-term services and supports. Read More
CMS Outlines 10 Fundamental Actions For States When Unwinding PHE. The Centers for Medicare & Medicaid Services (CMS) released on June 2, 2022, a tool for state Medicaid agencies to utilize in preparing for the end of the public health emergency (PHE) continuous enrollment period. The tool outlines 10 fundamental actions and resources for states, including creating an operational plan, coordinating with government partners, and strengthening automated processes. Read More
CMS Begins Implementation of Rule Establishing Standards for What Counts as HCBS Programs. Disability Scoop reported on June 1, 2022, that federal regulators have begun implementing a 2014 rule outlining the criteria home and community-based services (HCBS) programs must meet to obtain funding under Medicaid HCBS waivers. States have until March 17, 2023, to ensure the HCBS settings are places individuals choose to live, are integrated in the community, and allow individuals with disabilities to make independent choices about their daily activities and environment. The Centers for Medicare & Medicaid Services (CMS) expects the rule to impact over one million individuals. Read More
Health Plans to Issue $1 Billion in MLR Rebates in 2022, KFF Projects. Fierce Healthcare reported on June 1, 2022, that health plans are projected to issue $1 billion in rebates to enrollees this year, down from $2.1 billion in 2021, according to an analysis from the Kaiser Family Foundation (KFF). The majority of rebates, which are tied to minimum medical loss ratio (MLR) requirements, will go to enrollees in individual plans. Read More
Inpatient Rehab Providers Oppose Proposed Cuts to Medicare Reimbursement Rates for Early Transfers to Home Care. Modern Healthcare reported on June 1, 2022, that inpatient rehabilitation providers oppose an effort by federal regulators to reduce Medicare reimbursement rates for early transfers to home care. The policy could save nearly $1 billion, according to the U.S. Inspector General. Read More
Medicare Spending on Skilled Nursing Facilities Increased in 2020 Despite Utilization Decline, Report Finds. Skilled Nursing News reported on June 2, 2022, that Medicare skilled nursing facility (SNF) spending increased by $1.1 billion, or 4.4 percent, in 2020, according to a report from the Kaiser Family Foundation. However, the number of beneficiaries utilizing SNFs decreased by almost 200,000 users, contributing to a 16.3 percent increase in spending per user. Read More
Industry News
Medical Transportation Management to Acquire Veyo. Medical Transportation Management (MTM) announced on June 8, 2022, that it will acquire Veyo, a non-emergency medical transportation (NEMT) company based in San Diego, CA. The deal is expected to be completed this summer. Following the transaction, MTM will provide NEMT services to 16 million individuals in 31 states and the District of Columbia and generate approximately $1 billion in annual revenues. Read More
Oracle Is Cleared to Complete Acquisition of Cerner. Oracle Corporation announced on June 1, 2022, that it has received all necessary antitrust approvals to complete the acquisition of electronic health records company Cerner Corporation for approximately $28.3 billion. The deal is expected to be completed on June 6. Cerner will become part of Oracle’s industry business unit. Read More
UnitedHealth’s Optum Acquires Healthcare Associates of Texas. Fierce Healthcare reported on June 1, 2022, that Optum, a subsidiary of UnitedHealth Group, has acquired Healthcare Associates of Texas (HCAT), a primary care practice with 22 locations in the Dallas-Fort Worth area. HCAT, which was previously owned by Webster Equity Partners, has invested heavily in value-based care. Read More
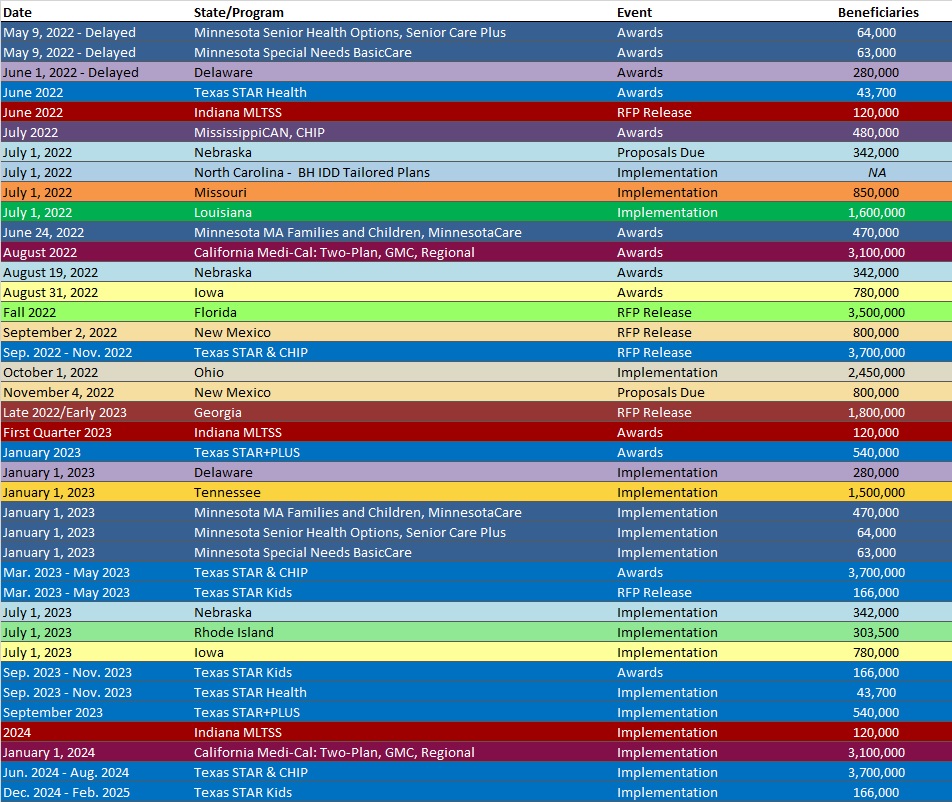
RFP Calendar
Company News
HMA News & Events
Health Management Associates Acquires Medical Audit Resource Services, Inc. On June 2, 2022, Jay Rosen, founder, president, and co-chairman of HMA, announced the firm’s acquisition of Medical Audit Resource Services, Inc. (MARSI). Founded in 1991, MARSI specializes in medical coding support, physician education and healthcare revenue cycle management. MARSI’s experts provide coding and auditing services for hospitals and physicians using inpatient, outpatient and risk adjusted reimbursement methodologies. Other clients include commercial fee-for-service plans as well as risk-adjusted plans. Read more
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
- Arizona Medicaid Managed Care Enrollment is Up 0.6%, Jan-22 Data
- California Dual Demo Enrollment is Up 0.6%, 2021 Data
- California Dual Demo Enrollment is Down 3.2%, May-22 Data
- California Medicaid Managed Care Enrollment is Up 7.3%, 2021 Data
- California Medicaid Managed Care Enrollment is Up 4.5%, May-22 Data
- Georgia Medicaid Managed Care Enrollment is Up 3%, Apr-22 Data
- Nebraska Medicaid Managed Care Enrollment Is Up 2.7%, Feb-22 Data
- Ohio Dual Demo Enrollment is Down 2.8%, Jan-22 Data
- Ohio Medicaid Managed Care Enrollment is Up 0.5%, Jan-22 Data
- Ohio Medicaid Managed Care Enrollment is Up 0.8%, Feb-22 Data
- Tennessee Medicaid Managed Care Enrollment is Up 1.5%, Mar-22 Data
- Wisconsin Medicaid Managed Care Enrollment is Up 10.1%, Nov-21 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Alaska Division of Behavioral Health Medicaid Billing and Clinical Documentation Information Management System RFI, Jun-22
- Colorado EpiTrax Implementation RFP, May-22
- Florida Medicaid Managed Care Re-Procurement RFI, May-22
- Georgia Medicaid Managed Care RFI, Jun-22
- Mississippi Support and Hosting of the Medicaid Eligibility System RFP, Apr-22
- Missouri HealthNet Managed Care RFP, Proposals, Awards, and Evaluation, 2021-22
Medicaid Program Reports, Data and Updates:
- Alaska DHSS Annual Medicaid Reform Reports, FY 2016-21
- Kansas KanCare Program External Quality Review Reports, 2020-22
- Massachusetts Medicaid Managed Care Quality Strategy Reports, 2017-22
- Nebraska Heritage Health External Quality Review Technical Report, 2021-22
- New Hampshire External Quality Review Organization (EQRO) Technical Reports, SFY 2018-21
- Oregon Medicaid External Quality Review Technical Reports, 2014-21
- Texas Medicaid Managed Care and CHIP External Quality Review Reports, 2016-21
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
