This week's roundup:
- In Focus: Evaluating the Delivery of Virtual Child Welfare Services
- Eligibility Redeterminations: Arkansas, Alaska, Centene, Idaho, Illinois, Minnesota, Texas
- California to Award Medicaid Bonus Payments to Nursing Homes
- Illinois Releases Medicaid FFS Dental Program RFP
- Indiana Awards Medicaid MLTSS Contracts to Four Managed Care Organizations
- Iowa House, Senate Pass Separate Bills to Change Medicaid Eligibility Asset Limit
- North Carolina Further Delays Implementation of Behavioral Health IDD Tailored Plans to October 2023
- New Mexico Lawmakers Question Cancellation of Medicaid Managed Care RFP
- Oregon Names Dana Hittle as Medicaid Director
- Medicare Advantage Insurers Report Average Margins Per Enrollee Twice as High as Other Health Insurance Markets
- Elevance Agrees to Acquire BCBS-LA for $2.5 Billion
In Focus
Evaluating the Delivery of Virtual Child Welfare Services
This week, our In Focus reviews a new Health Management Associates (HMA) report, highlighting hybrid (in-person & virtual visits) as the future of child welfare service delivery. During the COVID-19 public health emergency (PHE), the federal government waived the requirement for “once every 30 days” in-person visits by caseworkers for children in foster care, allowing these visits to occur virtually. In 2021, Casey Family Programs (CFP) commissioned HMA to evaluate the delivery of virtual child welfare services and outline the implications of the COVID-19 PHE on the child welfare system.
The report “Evaluating the Delivery of Virtual Child Welfare Services” is now available. It summarizes HMA’s findings and elevates the voices of staff in public and private child welfare agencies, and of youth and families with lived experiences, and examines their perspectives on how well virtual services have worked. It also details the implications of the COVID-19 PHE, the response from public child welfare agencies, and offers guidance on a hybrid (part in-person, part virtual) service model, which we believe will continue to be a factor in the future delivery of child welfare services.
As the COVID-19 PHE accelerated the spread and scale of telehealth adoption in health care, we surmised that the experience offered valuable opportunities to learn more about how the health care sector’s adoption of telehealth services could be applied in the child welfare community. While cognizant of the unique considerations for child welfare, this disruption also represents a substantial opportunity to rethink the child welfare system and advance both the use of technology as well as a more prevention- and strengths-based approach to child welfare.
The report highlights innovative approaches in the field, offers questions to frame a jurisdiction’s decision-making process, and provides a tool to facilitate an informed decision on the hybrid model. The report also offers a broader value proposition that outlines policy, practice, workforce, and technology imperatives to develop a hybrid approach to the delivery of child welfare services.
For questions, please contact Uma Ahluwalia, Rob Muschler, or Sarah Oachs.
HMA Roundup
Alaska
Alaska To Begin Medicaid Redeterminations in April. Alaska Public Media reported on February 26, 2023, that the Alaska Division of Public Assistance is expected to begin eligibility redeterminations for the state’s 263,000 Medicaid beneficiaries in April. Alaska is one of nine state’s that has not publicly released its plan on how it will handle redeterminations. Read More
Arkansas
Arkansas Begins Verifying Medicaid Eligibility Ahead of Redetermination Process. Politico reported on February 27, 2023, that the Arkansas Department of Human Services has begun sending out letters to Medicaid beneficiaries asking for proof of eligibility ahead of the restart of Medicaid redeterminations. The state has identified more than 420,000 beneficiaries who may now be ineligible and who will need to go through the redetermination process by the end of September. An additional 240,000 individuals will go through the renewal process within the year. Read More
California
California to Award Medicaid Bonus Payments to Nursing Homes. Modern Healthcare reported on February 27, 2023, that California intends to expand Medicaid bonus payments to nursing homes that hire additional workers, reduce staff turnover, or improve quality of care. The change means that even low-rated homes will likely receive bonuses, rather than only the top performers. The state is also allowing nursing homes to collect five percent more in labor costs annually through 2026. Read More
California Assembly Member Introduces Legislation to Extend Exchange Plan Eligibility to Undocumented Residents. The Sacramento Bee reported on February 24, 2023, that California Assembly member Joaquin Arambula (D-Fresno) introduced legislation that would extend Exchange plan eligibility to all qualified residents, regardless of immigration status. If passed, the state would likely have to wait until 2024 to seek federal approval of the plan. Read More
Idaho
Idaho Could Disenroll 150,000 from Medicaid in April 2023. The Idaho Department of Health and Welfare said on February 24, 2023, that it has identified 150,000 Medicaid enrollees with unknown eligibility status and who are at risk of losing coverage beginning April 1. Individuals who are disenrolled will be transitioned to state Exchange plans. Read More
Idaho Disenrolled 9,800 Medicaid Beneficiaries During Pandemic. NPR/ Kaiser Health News reported on February 27, 2023, that Idaho disenrolled 9,800 Medicaid enrollees while the federal ban on disenrollments was in effect. The state indicated the disenrollments occurred after multiple unsuccessful attempts to contact the beneficiaries. Read More
Illinois
Illinois Could Disenroll Up To 700,000 Medicaid Enrollees. The Chicago Tribune reported on February 28, 2023, that 384,000 to 700,000 Medicaid enrollees in Illinois could lose coverage during following eligibility redeterminations. Medicaid enrollment in the state increased by 1 million during the pandemic. Read More
Illinois Releases Medicaid FFS Dental Program RFP. The Illinois Department of Healthcare and Family Services released on February 23, 2023, a request for proposals (RFP) for the state’s Medicaid fee-or-service (FFS) dental program. The contract will cover approximately 780,000 individuals and run for five years, with one, five-year renewal option. Read More
Indiana
Indiana Awards Medicaid MLTSS Contracts to Four Managed Care Organizations. The Indiana Department of Administration announced on March 1, 2023, its intent to award contracts for the risk-based Medicaid Managed Care Long Term Services and Supports (MLTSS) program to Anthem Blue Cross and Blue Shield, Humana/Arcadian Health Plan, Molina Healthcare of Indiana, and UnitedHealthcare. The program will serve approximately 106,000 Medicaid enrollees aged 60 years and older, including Medicare and Medicaid dual-eligibles, individuals in a nursing facility, and individuals receiving LTSS in a home or community-based setting. The contracts are anticipated to begin on January 1, 2024, for a period of four years, with two one-year renewal options. Read More
Indiana Senate Committee Advances Legislation to Require Audits of Medicaid Drug Pricing. WIBQ reported on February 24, 2023, that the Indiana Senate Committee on Appropriations advanced legislation that would require audits of Medicaid drug costs for the last five fiscal years. The audits would cover cost sharing, spread pricing, discriminatory pricing, and more. Read More
Iowa
Iowa House, Senate Pass Separate Bills to Change Medicaid Eligibility Asset Limit. Iowa Public Radio reported on February 28, 2023, that the Iowa House and Senate passed separate bills to establish asset limits of $15,000 in liquid assets and personal property to qualify for Medicaid. The House version of the bill also directs the state to submit a request to enact Medicaid work and community engagement requirements for federal approval. Read More
Minnesota
Minnesota Could Disenroll Up to 25 Percent of Medicaid Members Following Redeterminations. The Star Tribune reported on March 1, 2023, that 15 to 25 percent of Minnesota’s 1.5 million Medicaid members could be disenrolled when redeterminations begin, according to the Minnesota Department of Human Services (DHS). Medicaid enrollment grew by 30 percent in the state during the public health emergency. DHS will start sending out renewal forms in May, starting with enrollees whose eligibility date is in July. Read More
Minnesota Awards $5.7 Million in Grants to Expand Access to Opioid Use Disorder Treatment. The Minnesota Department of Human Services announced on February 24, 2023, $5.7 million in grants awarded to 12 organizations to expand access to opioid use disorder treatment. The funding is largely going to organizations that primarily serve Native Americans and individuals of color. Read More
Mississippi
Mississippi House Committee Advances Bill to Extend Postpartum Medicaid Coverage. The Associated Press reported on February 28, 2023, that the Mississippi House Medicaid committee voted to advance a bill to extend postpartum Medicaid coverage from 60 days to 12 months. House Speaker Philip Gunn (R-Clinton), who had previously opposed the bill, has until March 8 to bring the bill to a full House vote. The Senate has already passed the bill. Read More
Mississippi Governor Asks Legislature to Pass Bill Extending Postpartum Medicaid Coverage from 60 Days to 12 Months. Mississippi Today reported on February 26, 2023, that Mississippi Governor Tate Reeves is asking the state legislature to pass a bill extending postpartum Medicaid coverage from 60 days to 12 months. The Senate recently passed the bill, and the House has until February 28 to advance it out of committee. House Speaker Phillip Gunn (R-Clinton) opposes the bill. Read More
Missouri
Missouri Audit Recommends State Refund $34 Million in Federal Medicaid Payments. The St. Louis Post-Dispatch reported on March 1, 2023, that the Missouri Department of Health and Human Services Office of Inspector General (OIG) is recommending that the state Department of Social Services refund at least $34.2 million in Medicaid payments to the federal government. The recommendation is based on an OIG audit, which found that some claims for consumer directed personal care assistance services did not comply with federal and state requirements. Read More
Missouri House Committee Advances Bill to Extend Postpartum Medicaid Coverage. The St. Louis Post-Dispatch reported on February 28, 2023, that the Missouri House Emerging Issues committee advanced a bill that would extend postpartum Medicaid coverage from 60 days to 12 months. The state Senate also recently passed a similar bill but with a provision that would exclude women who received abortions from the extra coverage. Read More
Montana
Montana Sees Savings from Medicaid Expansion, Report Finds. Health Payer Intelligence reported on February 28, 2023, that Medicaid expansion in Montana has resulted in cost savings, an 11 percent decline in emergency room visits, and increased access to preventive services increased, according to a report prepared by Manatt Health and the Montana Healthcare Foundation. Approximately 115,000 Montanans are covered by Medicaid expansion. Read More
Montana Senate Considers Bill to Revise How Nursing Home Medicaid Reimbursement Rates are Determined. Modern Healthcare reported on February 24, 2023, that the Montana Senate held an initial hearing on a bipartisan bill to revise how Medicaid reimbursement rates are set for nursing homes and assisted living facilities, including factors like inflation and cost-of-living adjustments. Lawmakers are also proposing fiscal 2025 rate increases. Read More
New Hampshire
New Hampshire House Passes Legislation to Extend Medicaid Postpartum Coverage to One Year. In Depth NH reported on February 22, 2023, that the New Hampshire House passed legislation to expand postpartum Medicaid coverage to one year for women and children, regardless of immigration status. Previously, the state offered Medicaid coverage for 60 days postpartum. Read More
New Hampshire Senate Committee Calls For Permanently Reauthorizing Medicaid Expansion. New Hampshire Public Radio reported on February 22, 2023, that the New Hampshire Senate Health and Human Services Committee recommended permanently reauthorizing the state’s Medicaid expansion program, which is currently set to expire in December 2023. The program, last reauthorized in 2018, currently covers 95,000 enrollees. Read More
North Carolina
North Carolina Further Delays Implementation of Behavioral Health IDD Tailored Plans to October 2023. The North Carolina Department of Health and Human Services announced on February 27, 2023, that it has further delayed the implementation of Behavioral Health and Intellectual/Developmental Disabilities (IDD) Tailored Plans until October 1, 2023. Implementation was originally scheduled for July 2022, then delayed to December 1, 2022, and then further delayed to April 1, 2023. Once implemented, the plans will cover nearly 150,000 individuals. Tailored Care Management launched on December 1, 2022, which provides some features of the tailored plans, including integrated care management. Read More
New Mexico
New Mexico Lawmakers Question Cancellation of Medicaid Managed Care RFP. The Albuquerque Journal reported on February 27, 2023, that New Mexico lawmakers are raising questions about the recent cancellation of the state’s Turquoise Care Medicaid managed care request for proposals (RFP). The RFP was cancelled after the state had already recommended that contracts be issued to four out of the five insurers who submitted bids. The state said the move was made to give the agency’s incoming leadership time to assess the design of the procurement. Read More
New York
New York House Republicans Propose Measure to Block State from Redirecting Medicaid Funds from Counties. Spectrum News reported on February 27, 2023, that New York House Republicans proposed a measure to block the state from redirecting Medicaid funds from counties. The proposal is in response to New York Governor Kathy Hochul’s proposed budget, which includes a proposal that would allow the state to use temporary enhanced federal Medicaid funding, instead of sharing it with counties. Read More
Oregon
Oregon Names Dana Hittle as Medicaid Director. The Oregon Capital Chronicle reported on February 23, 2023, that Dana Hittle has been named the permanent Medicaid director for the Oregon Health Authority. Hittle has been the interim director for the last two years. Read More
South Dakota
South Dakota Medicaid Work Requirements Ballot Measure Dies in Committee. South Dakota Public Broadcasting reported on February 24, 2023, that the South Dakota Senate Health and Human Services Committee killed a joint resolution that would have allowed Medicaid work requirements to be voted on in the next general election. Read More
South Dakota House Passes Legislation to Annually Adjust Community-based Provider Medicaid Rates. WNAX reported on February 23, 2023, that the South Dakota House passed legislation to annually adjust the Medicaid rates for community-based heath providers. The change is aimed at ensuring community-based providers are paid one hundred percent of costs, as opposed to 90 percent currently. Read More
Texas
Texas to Expand Staff to Process Medicaid Redeterminations; 1.7 Million Could Lose Coverage. State of Reform reported on February 24, 2023, that the Texas Health and Human Services Commission announced it plans to hire 600 additional employees to process Medicaid redeterminations starting in April. The state anticipates that up to 1.7 million enrollees will lose coverage, or 29 percent of the 5.9 million currently enrolled. Those who lose coverage will automatically have applications for the federal Exchange submitted. Read More
Wyoming
Wyoming Senate Committee Advances Medicaid Postpartum Coverage Extension Bill. The Casper Star Tribune reported on February 23, 2023, that the Wyoming Senate Labor, Health, and Social Services Committee advanced a bill that would extend Medicaid postpartum coverage for 12 months through 2027. The state currently offers postpartum coverage for 60 days. The bill will now be considered by the Senate Appropriations Committee. Read More
National
Medicare Advantage Insurers Report Average Margins Per Enrollee Twice as High as Other Health Insurance Markets. Kaiser Family Foundation reported on February 28, 2023, that Medicare Advantage plans reported average gross margins of $1,730 per enrollee in 2021, more than double the margins reported by individual, commercial, and Medicaid managed care insurers. Medicaid managed care insurers reported gross margins of $768 per enrollee, on average. Read More
Medicaid, Medicare Enrollment Nears 145 Million in November 2022, CMS Reports. The Centers for Medicare & Medicaid Services announced on February 28, 2023, that Medicaid and Children’s Health Insurance Program enrollment was almost 91.8 million in November 2022, a 0.5 percent increase from October 2022. Medicare enrollment was over 65 million, a 0.2 percent increase. More than 12 million individuals were eligible for both Medicare and Medicaid. Read More
MACPAC Meeting Is Scheduled for March 2. The Medicaid and CHIP Payment and Access Commission (MACPAC) announced on February 24, 2023, that its next meeting will be held on March 2. Among the topics for discussion will be policy options for countercyclical disproportionate share hospital allotments, an update on unwinding continuous coverage requirements in Medicaid, and findings from a focus group on experiences of people who are dually eligible for Medicaid and Medicare in integrated care models. Read More
CMS Proposes Rule to Address Medicaid DSH Payment Cuts to Hospitals. Revcycle Intelligence reported on February 24, 2023, that the Centers for Medicare & Medicaid Services (CMS) released a proposed rule aimed at addressing looming cuts to Medicaid hospital specific disproportionate share hospital (DSH) payments. Without the proposed rule, which involves a change in the methodology used to calculate payments, Medicaid DSH payments to hospitals will be reduced by $8 billion between 2024 and 2027. The comment period is open until April 24. Read More
CMS Awards Serco Exchange Eligibility Contract. Serco announced on February 23, 2023, it has been awarded a contract by the Centers for Medicare & Medicaid Services (CMS) to continue supporting eligibility determinations for individuals purchasing coverage through the federal Exchange. Serco has been working with CMS on Exchange eligibility since 2013. The contract is effective July 1, 2023, and will run for one year with four one-year options. It is worth approximately $690 million. Read More
Rural Hospitals Are Profitable for Year Ending June 2022 Due to COVID Relief Funds, KFF Analysis Finds. Kaiser Family Foundation (KFF) reported on February 23, 2023, that rural hospitals had a median operating margin of 3.9 percent in Medicaid expansion states and 2.1 percent in non-expansion states from July 2021 to June 2022, with federal COVID-19 relief funds buoying bottom lines. However, excluding relief funds, rural hospitals in non-expansion states would have had a negative median operating margin of 0.7 percent, and profits would have been lower in expansion states. Read More
CMS to Allow Medicaid Coverage of Substance Use Disorder, Mental Health Treatment in State Jails. The Associated Press reported on February 21, 2023, that the Centers for Medicare & Medicaid Services (CMS) will release guidance in Spring 2023 regarding Medicaid coverage of substance use disorder and mental health treatment in state jails, according to the Biden administration. Once guidance is released, states will need to submit waiver proposals to CMS in order to use Medicaid funding for these services. Read More
Industry News
Elevance Agrees to Acquire BCBS-LA for $2.5 Billion. Becker’s Payer Issues reported on February 28, 2023, that Elevance Health announced an agreement to acquire Blue Cross Blue Shield of Louisiana for more than $2.5 billion. Elevance expects to gain 1.6 million enrollees from the transaction. BCBS-LA will establish a foundation to address health equity with the funds from the deal. Read More
Family Practice Center to Transition to Full-Risk for Medicare Patients. Family Practice Center (FBC) announced on February 28, 2023, that it is partnering with Agilon Health to transition to a full-risk, value-based care model for its Central Pennsylvania Medicare patients. FPC is central Pennsylvania’s largest independent primary care physician group, serving more than 200,000 patients in 42 locations. Read More
Novant Health Agrees to Acquire Two Hospitals from Community Health Systems. Fierce Healthcare reported on February 28, 2023, that Novant Health agreed to acquire two hospitals in North Carolina from Community Health Systems for approximately $320 million. Following the transaction, Novant Health will have 17 medical centers and more than 800 locations across four states. Read More
Centene Expects 2.2 Million Medicaid Members to Lose Coverage After Redeterminations. The St. Louis Post-Dispatch reported on February 27, 2023, that 2.2 million of Centene’s 16 million Medicaid enrollees will lose coverage over an 18-month period as a result of Medicaid redeterminations, according to company projections. The insurer expects that up to 300,000 of these enrollees will transition to its Exchange plans. Read More
Humana to Focus on Government-Sponsored Health Plans, Phase Out Commercial Lines. Modern Healthcare reported on February 23, 2023, that Humana will focus on its government-sponsored insurance plans, including Medicare Advantage, after phasing out commercial lines in the next 18 to 24 months. The company had 986,400 enrollees in employer-sponsored plans as of December 2022. Read More
Pediatric Affiliates to Expand Transaction with Webster Equity Partners. Physician Growth Partners (PCP) announced on February 23, 2023, that it advised Pediatric Affiliates in a transaction with Webster Equity Partners, providing the New Jersey pediatric network with capital for expansion. Physician Growth Partners served as the exclusive transaction advisor to Pediatric Affiliates. Read More
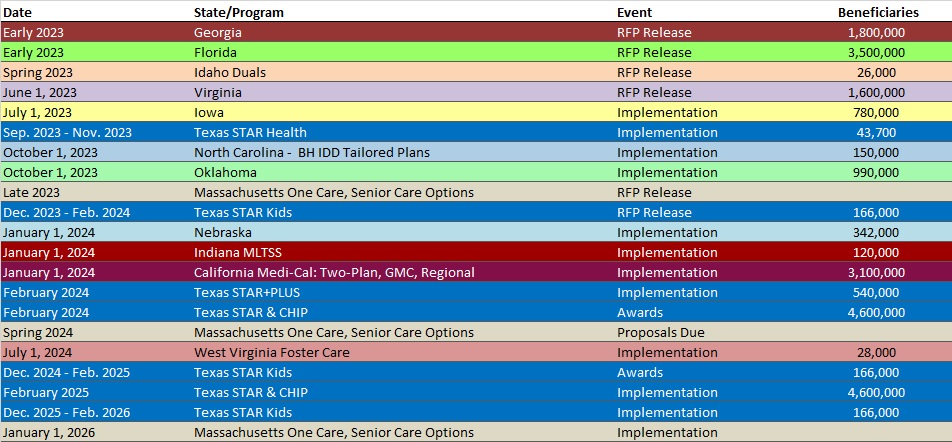
RFP Calendar
Company Announcements
HMA News & Events
The Moran Company Webinar. The New Technology Add-on Payment (NTAP) Program: What Life Sciences Companies Should Know About Medicare’s Time-Limited Program in 2023. Read More
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Colorado RAE Enrollment is Up 7.8%, 2022 Data
- District of Columbia Medicaid Managed Care Enrollment is Up 6.1%, Nov-22 Data
- Florida Medicaid Managed Care Enrollment is Up 11%, 2022 Data
- Illinois Medicaid Managed Care Enrollment is Up 5.5%, 2022 Data
- Illinois Dual Demo Enrollment is Down 2.2%, 2022 Data
- Maryland Medicaid Managed Care Enrollment Is Up 5.8%, 2022 Data
- Minnesota Medicaid Managed Care Enrollment is Up 7.5%, 2022 Data
- New Jersey Medicaid Managed Care Enrollment is Up 7%, 2022 Data
- New Mexico Medicaid Managed Care Enrollment is Up 2.3%, 2022 Data
- New York CHIP Managed Care Enrollment is Down 4.1%, 2022 Data
- Ohio Medicaid Managed Care Enrollment is Up 0.9%, 2022 Data
- Washington Medicaid Managed Care Enrollment is Up 7.2%, 2022 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Illinois Medicaid FFS Dental Program RFP, Feb-23
- Indiana Managed Long-Term Services and Supports RFP, Awards, and Proposals, Mar-23
Medicaid Program Reports, Data, and Updates:
- Arkansas Comprehensive Unwinding Plan, Feb-23
- New York Public Health Emergency and Continuous Coverage Unwind Plan, Feb-23
- Ohio Resuming Routine Medicaid Eligibility Operations Materials, 2022-23
- South Carolina DHHS Annual Accountability Reports, 2019-22
- South Carolina Medicaid Managed Care Rate Certifications, SFY 2019-23
- Washington Medicaid Managed Care External Quality Review Reports, 2012-22
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.