HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Financial Impact Summary of the 2024 Medicare Advantage Advance Notice

- Arizona House Committee Advances Bill to Reduce Medicaid Redetermination Period

- Colorado Lawmakers Introduce Bill to Authorize Medicaid Reimbursement for Community Health Services

- Redeterminations News: Delaware, Nebraska, Nevada, North Carolina, Rhode Island

- Maryland Health Information Exchange to Expand Medicaid Eligibility Redetermination Notifications

- Mississippi Releases Medicaid Utilization Management, Quality Improvement Organization IFB

- New Jersey Senate Committee Advances Bill to Increase Medicaid Reimbursement Rates for Assisted Living Facilities

- New Mexico House Passes Bill to Study Medicaid Buy-in Program

- North Carolina Senate Committee Advances Medicaid Expansion Bill

- Wisconsin Governor Proposes Tying Medicaid Expansion to Medicaid Reimbursement Rates

- West Virginia House Passes Bill to Scrap Medicaid Managed Care RFP Process, Move to Applications

- 15 States Seek Section 1115 Waiver Amendments to Provide Medicaid Services to Incarcerated Individuals Prior to Release

- VillageMD Acquires CT-based Multispecialty Group Starling Physicians

- Presbyterian Healthcare Services, UnityPoint Health to Merge

In Focus
Financial Impact Summary of the 2024 Medicare Advantage Advance Notice
This week, our In Focus section highlights a Wakely, an HMA Company, summary and analysis of the 2024 Medicare Advantage Advance Notice, prepared for America’s Health Insurance Plans (AHIP). The Centers for Medicare & Medicaid Services (CMS) released the contract year (CY) 2024 Advance Notice with an accompanying fact sheet on February 1, 2023. AHIP has retained Wakely Consulting Group to provide a financial impact summary report of the information presented in the notice. Specifically, Wakely was asked to analyze changes to Medicare Advantage (MA) revenue, risk adjustment models, and fee-for-service (FFS) normalization.
Key highlights of the analysis are:
- The CY 2024 FFS growth rate is lower than projections from the 2023 Final Announcement. A portion of the downward restatement is driven by a technical change. CMS has not commented on the additional drivers.
- Based on a large sample of plans, Wakely estimated that the proposed Part C risk adjustment model is expected to decrease plan risk adjusted payment by 3.7 percent overall, which represents a bigger headwind than the CMS estimated decrease of 3.12 percent. The impacts vary significantly by model segment and geographic region, and for individual plans.
- The proposed FFS normalization factor excludes PY 2021 risk scores in the calculation of the underlying trend. The exclusion of PY 2021 increases the FFS normalization factor which decreases PY 2024 risk scores.
The report, released March 6, 2023, provides additional detail and discussion of these issues. For questions, please contact Tim Courtney or Rachel Stewart.
HMA Roundup
Arizona
Arizona House Committee Advances Bill to Reduce Medicaid Redetermination Period. State of Reform reported on March 3, 2023, that the Arizona House Health Committee advanced a bill (HB 2624) to reduce the Medicaid redetermination period from 12 months to nine months for all members by December 31. An estimated 600,000 Medicaid members will no longer qualify. Read More
Colorado
Lawmakers Introduce Bill to Authorize Medicaid Reimbursement for Community Health Services. The Greeley Tribune reported on March 6, 2023, that lawmakers introduced a bill (SB 23-2) that would authorize the Colorado Department of Health Care Policy and Financing (HCPF) to seek federal approval to provide Medicaid reimbursement for community health worker services. HCPF would determine what qualifications community health workers would need, what services Medicaid might cover, and how they would be reimbursed. The bill would also require the state to present a report on how community health workers are being utilized through Medicaid by January 31, 2026. Read More
Connecticut
General Assembly Committee Advances Proposal to Extend Medicaid Coverage to Individuals Under 19 Without Legal Status. The Record-Journal/The Connecticut Mirror reported on March 6, 2023, that the Connecticut General Assembly Human Services Committee advanced a proposal to extend Medicaid coverage to individuals 18 and under, regardless of immigration status, beginning January 1, 2024. In 2022, the General Assembly extended coverage to individuals 12 and under without permanent legal status, as long as their family meets the qualifying income limits for Medicaid. The proposal now goes to the Appropriations Committee for review. Read More
Delaware
Delaware Could Disenroll Up to 50,000 Medicaid Enrollees When Redeterminations Begin. The Delaware Department Health and Social Services announced on March 1, 2023, that a projected 40,000 to 50,000 Medicaid enrollees could be disenrolled when redeterminations begin. The state, which has about 310,000 Medicaid members, will be working with Medicaid plans to reach out to beneficiaries. Read More
Florida
Florida Made an Estimated $6.9 Million in Improper Capitated Medicaid Payments in August 2020, Federal Audit Finds. The Washington Examiner reported on March 3, 2023, that the Florida Agency for Health Care Administration (AHCA) made an estimated $6.9 million in Medicaid capitation payments in August 2020 on behalf of enrollees who were residing in another state and concurrently enrolled in both Florida and another state Medicaid program, according to a report by the U.S. Office of the Inspector General (OIG). Read More
Maryland
Maryland Health Information Exchange to Expand Medicaid Eligibility Redetermination Notifications. CRISP, Maryland’s health information exchange, announced on March 3, 2023, that it would expand its effort to notify the state’s 1.6 million Medicaid enrollees of upcoming eligibility redeterminations. CRISP, which rolled out the program with Federally Qualified Health Centers in February 2023, will now make it available to all participating providers and Medicaid managed care plans by May. Read More
Massachusetts
Massachusetts Makes $92 Million in Improperly Documented Behavioral Telehealth Payments, Audit Finds. The Massachusetts Office of the State Auditor announced on March 2, 2023, that MassHealth made approximately $92 million in improperly documented payments to providers for behavioral telehealth services, according to the Medicaid Audit Unit annual report. The audit also found $4.6 million in improper payments to dental providers. Read More
Mississippi
Legislature Passes Bill to Extend Postpartum Medicaid Coverage to 12 Months. Mississippi Today reported on March 7, 2023, that the Mississippi House passed a Senate bill to extend postpartum Medicaid coverage from 60 days to 12 months. The bill now goes to Governor Tate Reeves, who is expected to sign it. Read More
Mississippi Releases Medicaid Utilization Management, Quality Improvement Organization IFB. The Mississippi Division of Medicaid released on March 3, 2023, an invitation for bids (IFB) for a single contractor to provide utilization management (UM) and quality improvement organization (QIO) for the Medicaid fee-for-service population for medical services, behavioral health services, dental services, and level care of reviews. The contractor will also provide peer review services, clinical/medical consultation, quality improvement services, and care management services. Responses are due April 28, with awards expected May 19. Contract implementation will be July 6, with the operational phase beginning February 1, 2024. The current UM/QIO contract with Alliant Health Solutions ends on January 31, 2024. The new contract will also include non-emergency, outpatient advanced imaging services, currently under a separate UM/QIO contract ending on November 30, 2023, with two option years. Read More
Montana
Montana Bills to Raise Medicaid Reimbursement Rates Advance in Legislature. The Bozeman Daily Chronicle reported on March 3, 2023, that a Montana bill (HB 649) to raise Medicaid reimbursement rates passed a second House reading and now moves to an appropriations committee. Another bill (SB 296) also cleared an initial vote in the Senate. The bill would require nursing home rates to increase annually in line with inflation up to 3 percent starting in 2025 and require an analysis every four years to determine if a new base level for Medicaid reimbursements is needed. The Senate bill would also move people from the Big Sky Waiver program to the Community First Choice program, which allows older or disabled persons to “self-direct” their care to someone of their own choice. Read More
Nebraska
Nebraska Projects Up to 80,000 Medicaid Enrollees Could Lose Coverage During Redeterminations. The Nebraska Department of Health and Human Services announced on March 3, 2023, that 40,000 to 80,000 Medicaid enrollees could lose coverage following Medicaid eligibility redeterminations. The state has sent notice of renewal to 390,000 beneficiaries, and those deemed ineligible will be directed to the federal Exchange. Read More
Nevada
Nevada Says 200,000 Medicaid Beneficiaries Could Be Impacted by Redeterminations. KOLO reported on March 1, 2023, that Nevada projects 200,000 Medicaid beneficiaries could be impacted when eligibility redeterminations begin, according to the state Department of Health and Human Services (HHS). HHS is sending out renewal packets so beneficiaries can reapply. Read More
New Jersey
Senate Committee Advances Bill to Increase Medicaid Reimbursement Rates for Assisted Living Facilities. The New Jersey Monitor reported on March 6, 2023, that the New Jersey Senate Health, Human Services and Senior Citizens Committee advanced a bill to increase daily Medicaid reimbursement rates for assisted living. The bill calls for a $10 to $13 increase to $114 for assisted living facilities, $104 for comprehensive personal care homes, and $94 for assisted living programs. Rates would be effective July 2023 and recalculated annually. Read More
New Mexico
House Passes Bill to Study Medicaid Buy-in Program. The Albuquerque Journal reported on March 7, 2023, that the New Mexico House passed a bill to commission a study on allowing individuals not eligible for Medicaid to access coverage on a sliding scale of premiums. The goal of the study is to determine the impact on private insurance, medical providers, and other stakeholders. The bill now heads to the Senate. Read More
North Carolina
North Carolina Senate Committee Advances Medicaid Expansion Bill. The Associated Press reported on March 7, 2023, that the North Carolina Senate Health Care Committee advanced a Medicaid expansion bill. The bill also includes changes to hospital certificate of need rules. The bill is expected to advance through two other committees and go to the full Senate for a vote. Read More
House, Senate Leaders Agree on Medicaid Expansion Bill. The News & Observer reported on March 2, 2023, that North Carolina House speaker Tim Moore (R-Cleveland) and Senate leader Phil Berger (R-Rockingham) announced an agreement on a Medicaid expansion bill. The bill will ease hospital certificate of need regulations, a roadblock to prior House and Senate agreement. Read More
North Carolina Could Disenroll Up to 300,000 Medicaid Enrollees when Redeterminations Begin. The North Carolina Department of Health and Human Services announced on March 1, 2023, that up to 300,000 Medicaid members in the state could be disenrolled when redeterminations begin. The state is working with counties to reach beneficiaries to redetermine eligibility. Read More
Rhode Island
Rhode Island Could Disenroll 22,000 Medicaid Members After Redeterminations Begin. The Providence Journal reported on March 1, 2023, that about 22,000 Medicaid enrollees in Rhode Island could lose coverage when eligibility redeterminations begin. The state has about 360,000 Medicaid beneficiaries. Read More
South Carolina
South Carolina Announces $35 Million in Grants for Behavioral Health Crisis Stabilization Services. The South Carolina Department of Health and Human Services announced on March 2, 2023, the availability of $35 million in grants for building specialized hospital-based emergency departments and observational units dedicated to behavioral health. The state will be accepting grant applications until April 24.
Wisconsin
Governor Proposes Tying Medicaid Expansion to Medicaid Reimbursement Rates in Fiscal 2025 Budget. The Wisconsin Examiner reported on March 3, 2023, that Wisconsin Governor Tony Evers is proposing increases in Medicaid reimbursement rates for hospitals and providers in his fiscal 2025 budget, but only if the state implements Medicaid expansion. The increases would boost hospital rates by $626 million and other provider rates by $250 million. Read More
West Virginia
House Passes Bill to Scrap Medicaid Managed Care RFP Process, Move to Applications. West Virginia News reported on March 7, 2023, that the West Virginia House passed a bill that would scrap the Medicaid managed care request for proposals process, allowing any health insurance entity to submit an application to participate as long as it meets state and federal requirements. The current request for proposals process limits the awards to three managed care plans. The bill now moves to the Senate. Read More
Wyoming
Wyoming Extends Postpartum Medicaid Coverage from 90 Days to 12 Months. Buckrail News reported on March 6, 2023, that Wyoming Governor Mark Gordon signed a bill (HB0004) to extend postpartum Medicaid coverage from 90 days to 12 months. The bill will be in effect from July 1, 2023, through March 31, 2027, and cost an estimated $3.8 million in state and federal funding. Read More
National
15 States Seek Section 1115 Waiver Amendments to Provide Medicaid Services to Incarcerated Individuals Prior to Release. Kaiser Health News reported on March 8, 2023, that 15 states are seeking Section 1115 waiver amendments to allow eligible incarcerated individuals to receive Medicaid coverage prior to release. California is the first state to receive federal approval to provide the services. Read More
Biden Wants Medicare to Negotiate Prices for Additional Drugs in Fiscal 2024 Budget. Fierce Healthcare reported on March 7, 2023, that President Biden has proposed allowing Medicare to negotiate prices for additional drugs in the proposed fiscal 2024 budget, to be released on March 9. Building on the drug price reforms under the Inflation Reduction Act, Medicare will negotiate prices for a small number of drugs beginning in 2026 and bring drugs into negotiation sooner after they launch. Read More
Hospital Groups Urge Congress to Delay Medicaid DSH Cuts. Becker’s Hospital Review reported on March 7, 2023, that nine organizations representing hospitals and health systems are urging Congress to delay Medicaid disproportionate share hospital (DSH) cuts, which are currently set to begin in fiscal 2024. Hospital stakeholders estimate the cuts will total $8 billion. Read More
U.S. House Committee Launches Investigation into PBMs. Modern Healthcare reported on March 6, 2023, that the U.S. House Oversight and Accountability Committee Chair James Comer (R-KY) launched an investigation into the anti-competitive tactics of pharmacy benefit managers (PBMs). Comer sent letters to CVS Health’s Caremark, UnitedHealth Group’s OptumRx, and Cigna’s Express Scripts, seeking information on how they design formularies, engage patients, collect rebates from pharmaceutical companies, and establish differential pricing arrangements. The committee also requested information from federal agencies about how PBMs interact with government health programs. Read More
AHIP Expresses Concern Over Changes to Medicare Advantage Risk Adjustment Model. America’s Health Insurance Plans (AHIP) said on March 6, 2023, that it had “serious concerns” over proposed changes to the Medicare Advantage (MA) risk adjustment methodology, citing a Wakely study suggesting the changes would result in payment cuts of 3.7 percent to MA plans and 6.4 percent for dual eligibles in 2024. AHIP noted its concerns in formal comments to the Centers for Medicare & Medicaid Services regarding the Advance Notice of Methodological Changes for Calendar Year 2024 for MA and Part D. Read More
Federal Judge Orders CMS to Reinstate Medicaid Coverage for Members Eligible for Medicare Savings Program. CT Insider reported on March 6, 2023, that a federal judge in Connecticut ordered the Centers for Medicare & Medicaid Services (CMS) to reinstate Medicaid coverage for individuals who lost coverage due to a Trump administration rule that allowed the disenrollment of Medicaid members eligible for the Medicare Savings Program. Read More
U.S. House Democrats Oppose Potential Medicaid Cuts by Republicans in Fiscal 2024 Budget Talks. The Hill reported on March 5, 2023, that U.S. House Democrats say they will oppose potential Medicaid funding cuts by Republicans when crafting the federal fiscal 2024 budget. Republican leaders are seeking to cut Medicaid to reduce the deficit and are supportive of proposals that include capping spending and imposing work requirements. Read More
CMS Releases State Timelines for Initiating Medicaid Unwinding Renewals. The Centers for Medicare & Medicaid Services (CMS) published on March 2, 2023, the anticipated state timelines for initiating Medicaid unwinding-related renewals. The chart shows the expected first month for each state’s unwinding-related renewals, as well as the anticipated effective date for the first procedural terminations. Read More
Medicare Part D Plans Improperly Authorized $86 Million in Opioid Prescriptions, Audit Finds. STAT News reported on March 2, 2023, that Medicare Part D plans improperly authorized $86 million worth of opioid prescriptions between July 2015 and December 2019, according to an audit by the U.S. Office of Inspector General. The audit found that the prior authorization process used by the plans was not robust enough to catch the prescription errors. Read More
Medicaid, CHIP Enrollment Grows by 23.3 Million During the Pandemic, Study Finds. Kaiser Family Foundation reported on March 2, 2023, that Medicaid and Children’s Health Insurance Program (CHIP) will have grown by 23.3 million enrollees from February 2020 to March 31, 2023, when the continuous enrollment period ends. Oklahoma saw the largest growth at 81 percent, while Connecticut saw the smallest at 22 percent. Read More
U.S. House Committee Probes PBMs for Documents Regarding Anti-Competitive Tactics. Fierce Healthcare reported on March 1, 2023, that the U.S. House Oversight Committee demanded that CVS Caremark, Express Scripts, and OptumRx release documents on potential anti-competitive tactics among pharmacy benefit managers (PBMs), including spread pricing and rebates. The request also covers topics like preferred drug lists and direct and indirect remuneration fees. Read More
Industry News
VillageMD Acquires CT-based Multispecialty Group Starling Physicians. VillageMD announced on March 3, 2023, that it has acquired Starling Physicians, a Connecticut-based multispecialty group providing primary and specialty care, effective March 1. Terms of the transaction were not disclosed. Read More
Presbyterian Healthcare Services, UnityPoint Health to Merge. Modern Healthcare reported on March 2, 2023, that Presbyterian Healthcare Services and UnityPoint Health announced that they would be merging to create an organization with approximately $11 billion in annual revenues. The combined organization will have 48 hospitals, a health insurance plan offered through Presbyterian, and 40,000 employees. Read More
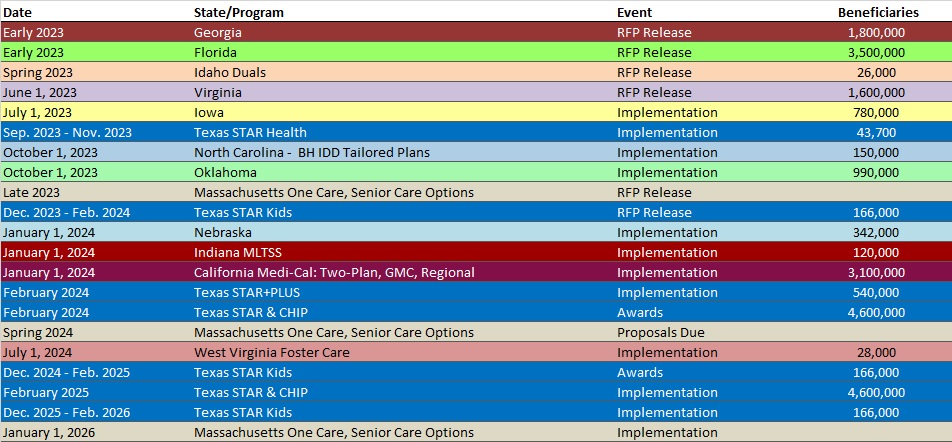
RFP Calendar
HMA News & Events
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Arizona Medicaid Managed Care Enrollment is Up 7.1%, 2022 Data
- Georgia Medicaid Managed Care Enrollment is Up 1.4%, Mar-23 Data
- Indiana Medicaid Managed Care Enrollment Is Up 10.3%, 2022 Data
- Iowa Medicaid Managed Care Enrollment is Up 1.4%, Jan-23 Data
- Michigan Medicaid Managed Care Enrollment is Up 4.3%, 2022 Data
- Michigan Dual Demo Enrollment is Up 8.1%, 2022 Data
- Mississippi Medicaid Managed Care Enrollment is Down 2%, Jan-23 Data
- North Dakota Medicaid Expansion Enrollment is Up 1.4%, Jan-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Massachusetts Comprehensive Care Coordination, Care Management Services Program Contractor RFR, Mar-23
- Minnesota Targeted Opioid Use and Misuse Prevention and Treatment Services RFP, Mar-23
- Mississippi Medicaid FFS Non-Emergency Transportation Brokerage Services IFB and Related Documents, 2023
- Mississippi Utilization Management/Quality Improvement Organization IFB, Mar-23
Medicaid Program Reports, Data, and Updates:
- Delaware Plan for Unwinding from the COVID-19 PHE, Feb-23
- Florida Medicaid Overview Presentation, Feb-23
- Florida Statewide Medicaid Managed Care Long Term Care Program Presentation, Feb-23
- Iowa Continuous Coverage Unwind Plan, Feb-23
- Kansas Continuous Enrollment Unwinding Plan, Feb-23
- New Hampshire Prescription Drug Affordability Board Meeting Materials, Jan-23
- Oregon Prescription Drug Affordability Board Meeting Materials, Feb-23
- South Dakota Medicaid Continuous Coverage Unwinding Plan, Feb-23
- Vermont Medicaid Continuous Coverage Unwinding Plan, Jan-23
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
