HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: How Will CMS’s Proposed Rule Shift Standards for Medicaid Enrollee Access to Services?

- Arizona Legislature Approves $3.4 Billion for Fiscal 2023 Medicaid Managed Care Payments

- Arkansas Disenrolls Almost 73,000 Medicaid Beneficiaries During April Redeterminations

- Georgia Community Health Commissioner to Step Down Summer 2023

- Idaho Finds 29,000 Ineligible Medicaid Beneficiaries During Redeterminations Healthy Blue

- Kansas Hires President Ahead of Bid on Medicaid Contract

- HAP, CareSource Form Partnership to Serve Michigan Medicaid Beneficiaries

- Rhode Island Senate Passes Bill to Use Medicaid Funds to Help Homeless Beneficiaries Find Housing

- Virginia Plan to Cut Medicaid Payments for Preventable ER Visits Is Vacated by Federal Judge

- 1.7 Million Medicaid Beneficiaries Could Lose Coverage if Work Requirements are Implemented, KFF Projects

- Option Health Care To Acquire Amedisys

- Cano Health Looks to Sell Non-core Assets, Focus on Medicare Advantage

In Focus
How Will CMS’s Proposed Rule Shift Standards for Medicaid Enrollee Access to Services?
This week’s In Focus is the second in a two-part look at the Centers for Medicare & Medicaid Services’ (CMS’s) recently proposed changes to the Medicaid program. Last week we covered CMS’s proposed changes to the federal Medicaid managed care regulations (CMS-2439-P). This week we review the Medicaid Access to Care proposed rule (CMS-2442-P).
As we discussed last week, the managed care and access to care rules include significant changes to core structural and financing aspects of the Medicaid program. Though state agencies, providers, health plans, consumer groups, and other stakeholders will want to understand the distinct requirements and expectations in each rule that apply to them, the proposed changes cannot be viewed in isolation.
The Access to Care rule addresses a range of challenges that shape the experience of Medicaid enrollees, regardless of whether they are in managed care programs or traditional fee-for-service (FFS). The proposed policy changes also are designed to create an updated federal framework for Medicaid’s home and community-based services (HCBS) programs. These proposals come at a pivotal time, as states are facing workforce shortages, particularly among HCBS direct care workers (DCWs).
The remainder of this In Focus delves into notable components of the proposed changes and includes analysis of the implications of these policies for stakeholders. CMS will benefit from stakeholder input; the deadline for submitting comments is July 3, 2023.
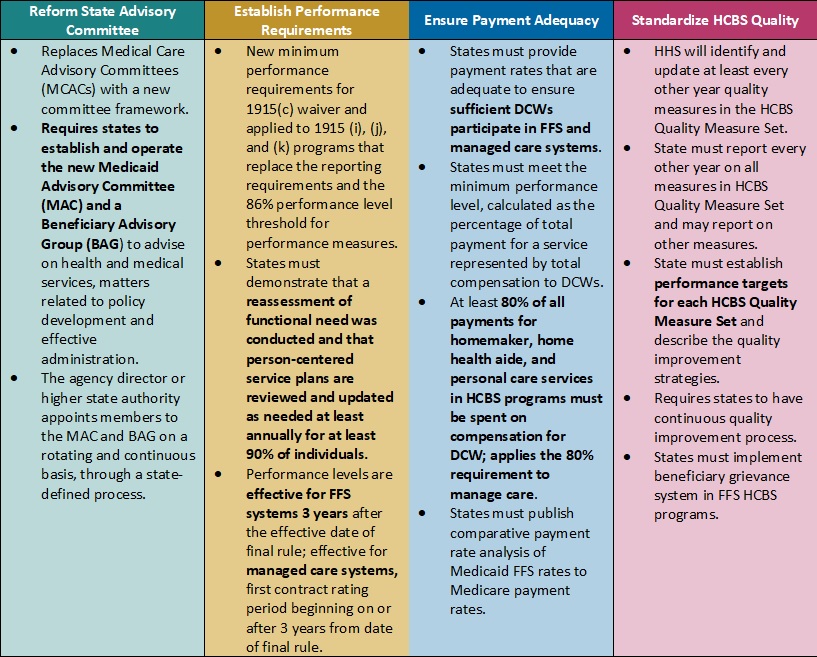
Table 1. Access to Care Regulations: Overview of Proposed Changes
Key Themes and Considerations
Ensuring Payment Adequacy for Key HCBS Services Experiencing Workforce Shortages. One of the most notable proposed changes that would directly impact DCWs is a requirement that at least 80 percent of Medicaid payments be spent on compensation. The proposed rule would apply to homemaker, home health aide, and personal care services, as they represent a large portion of HCBS services that DCWs provide. The proposal is based on feedback from states that have implemented similar provisions, which have ranged from 75 to 90 percent compensation requirements.
CMS specifically seeks stakeholder feedback on the percentage that should be adopted. This policy provision also is important from an equity perspective, given that 90 percent of DCWs are women and 60 percent are members of racial or ethnic minority populations. However, increased or mandated DCW rates may make it difficult for HCBS providers to sustain their businesses as they manage the increased administrative pressures of electronic visit verification, the complexity of filing claims for managed long-term services and supports (MLTSS), and the additional work that HCBS quality measurement may create. Smaller HCBS providers, some of which may have deep cultural expertise, may struggle to sustain themselves and meet these requirements.
Table 2. Access to Care Regulations: Snapshot of Proposed Rate, Access, and Payment Changes
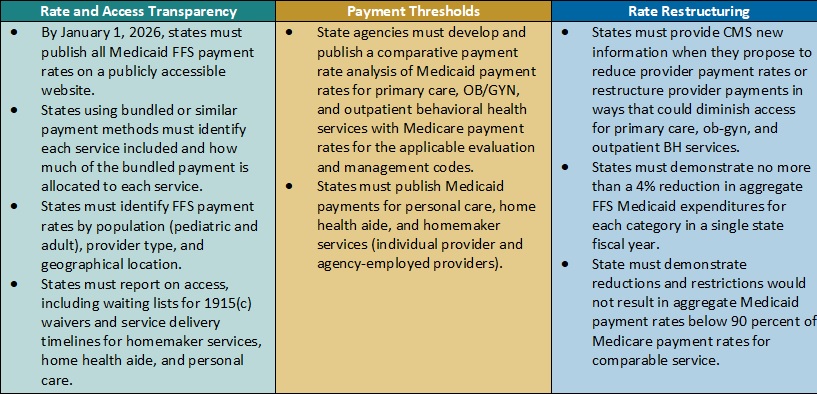
Payment Alignment. CMS is seeking to align access to care strategies and payment rate transparency more closely across the FFS and managed care delivery systems. The proposed rule includes several changes that CMS has developed achieve this goal. For example:
- CMS plans to require that states publish more detailed rate information in a consistent format. States, health plans, providers, and other interested stakeholders will want to consider the implications by delivery system. Additional transparency requirements could create a new opportunity to understand rates across payers and states and use this information in addressing access challenges for services.
- The proposed rule also would require extensive comparative analysis of Medicaid FFS rates and Medicare rates. CMS proposes to use Medicare non-facility payment rates as a benchmark to determine if states are meeting federal Medicaid access State analyses will be vital to CMS oversight as well as advocacy efforts within states to monitor and update FFS rates as needed.
Strengthening the Focus on Quality in State HCBS Programs. Over the last several decades, states and Medicaid stakeholders have made significant progress toward increasing participation in HCBS programs and community integration initiatives to counter Medicaid’s institutional bias. CMS is proposing more consistency in the expectations and reporting for HCBS quality measures to further the impact and create a consistent foundation for the recently mandated HCBS quality initiatives starting to take root.
In the short-term, the proposed changes will require states, and likely downstream providers and Medicaid agencies, to immediately change their quality reporting policies and systems. States and their stakeholders will want to map out processes for cyclical updates to HCBS quality measures, including cross-walking the future measures with existing ones, making systems changes, and updating dashboards. Targeted attention and focus will be needed to identify realistic HCBS performance targets that yield successful improvement strategies in the midst of a workforce crisis. Longer term, it will be necessary to map out when updates and reporting will be required to strengthen the rigor and accountability for state performance in the HCBS quality measure set, as well as reinforce the information available to make policy, clinical, and operational improvements to Medicaid programs.
HCBS Access Measurement. CMS is proposing new FFS HCBS payment and access transparency requirements to ensure compliance with Medicaid provider payment rules that require payments to be adequate to enlist at least the same number of providers that the overall geographic population can access. Because the targeted HCBS services do not have a comparable Medicare rate, CMS proposes implementation of a payment rate disclosure approach that would standardize data and monitoring across service delivery systems, with the goal of improving access. In addition to proposed payment transparency changes, CMS proposed new reporting on HCBS waiver waiting lists and timelines for the start of related services once authorized.
These new reporting requirements will provide stakeholders with more information to benchmark their state’s experience with other providers across the nation. This information could be influential to policymakers and legislators and help uncover some of the core contributors to our nation’s HCBS workforce shortage.
Improving Health Equity with Medicaid Beneficiary Input. CMS proposes overhauling the scope and membership of the state Medical Care Advisory Committee. The new Medicaid Advisory Committee (MAC) would continue to advise the state on health and medical matters and play an expanded advisory role on matters of policy development and effective administration of the program. CMS also plans to require that states establish a Beneficiary Advisory Group (BAG) composed of current or past Medicaid beneficiaries. A subset of BAG members would serve on the MAC to ensure their perspectives are integrated into the committee’s recommendations to states.
Under the new federal requirements, MAC representatives could have greater relative input and influence on policies and actions each state Medicaid agency advances. Medicaid stakeholders will want to ensure the MAC’s minimum federal requirements support effective structures and processes in states.
What’s Next
CMS plans to reframe Medicaid access as one of three parts of the continuum of care, along with enrollment and maintenance of coverage. The proposals in the Access to Care rule would have a meaningful impact on the volume and type of data available to evaluate the relationship between Medicaid payment rates and access across all delivery systems.
States, managed care organizations, providers, Medicaid enrollee advocacy organizations, and other interested stakeholders should analyze the proposals and consider submitting comments to CMS on the feasibility, potential impact, and, where applicable, alternatives to the proposed changes. They also can use this time to begin planning and determine which resources and tools they may need to prepare for implementation of changes across delivery systems in the Medicaid program.
HMA’s experts are taking a wholistic approach to reviewing the Access to Care and Managed Care proposed rules in tandem and identifying key points of intersection.
For more information on the access to care proposed rule, contact HMA’s team of experts, Susan McGeehan and Andrea Maresca.
HMA Roundup
Alaska
Alaska Legislature Passes Bill to Extend Postpartum Medicaid Coverage. The Anchorage Daily News reported on May 5, 2023, that the Alaska legislature passed a bill (Senate Bill 58) to extend postpartum Medicaid coverage from 60 days to 12 months. About 51 percent of births in Alaska are covered by Medicaid. The bill now goes to Governor Mike Dunleavy, who is expected to sign it. Read More
Arizona
Arizona Legislature Approves $3.4 Billion for Fiscal 2023 Medicaid Managed Care Payments. Capitol Media Services reported on May 3, 2023, that the Arizona legislature approved $3.36 billion in funding for the Arizona Health Care Cost Containment System to continue making capitated payments to Medicaid managed care plans through the end of fiscal 2023. Read More
Arkansas
Arkansas Disenrolls Almost 73,000 Medicaid Beneficiaries During April Redeterminations. The Arkansas Department of Human Services announced on May 8, 2023, that approximately 72,800 Medicaid beneficiaries were disenrolled during April redeterminations. That includes nearly 45,000 whose coverage was only extended due to the public health emergency. Read More
Colorado
Colorado Restarts Prior-authorization Process for In-home Nursing Care for Children Covered by Medicaid. The Colorado Sun reported on May 10, 2023, that Colorado restarted its prior-authorization process for in-home nursing care for children covered by Medicaid. The state froze the process during 2020 when COVID-19 began, resumed it in November 2021, and then froze it again in October 2022. Read More
Connecticut
Connecticut House Committee Proposes Increasing Medicaid Reimbursement Rates for Physician Services. The Connecticut Mirror reported on May 9, 2023, that the Connecticut House Appropriations Committee is proposing $9.2 million for fiscal 2024 and $18.3 million for fiscal 2025 to increase Medicaid reimbursement rates for physician services. The increase would put rates at 65 percent of Medicare in 2024. Separately, the Senate Appropriations Committee advanced a bill (Senate Bill 10) to allow Medicaid to pay for services provided by community health workers. Read More
Florida
Florida Legislature Passes Bill to Increase Income Threshold for KidCare Coverage. News Service of Florida reported on May 4, 2023, that the Florida House and Senate passed a bill (HB 121) to increase the threshold for KidCare coverage to 300 percent of the federal poverty level. KidCare includes the Florida Children’s Health Insurance Program. The bill now goes to Governor Ron DeSantis for his signature. Read More
Georgia
Georgia Community Health Commissioner to Step Down Summer 2023. The Atlanta Journal-Constitution reported on May 5, 2023, that Caylee Noggle will step down from her current position as the commissioner of the Georgia Department of Community Health (DCH) in summer 2023. Noggle will take over as president and chief executive of the Georgia Hospital Association. Read More
Georgia Enacts Legislation to Provide Remote Monitoring for Pregnant Medicaid Beneficiaries. AllOnGeorgia reported on May 4, 2023, that Georgia Governor Brian Kemp signed a bill (SB 106) to provide a three-year pilot program to provide remote patient monitoring for pregnant Medicaid beneficiaries. The program will begin in fiscal 2024. Read More
Idaho
Idaho Finds 29,000 Ineligible Medicaid Beneficiaries During Redeterminations. KTVB reported on May 9, 2023, that Idaho has found approximately 29,000 ineligible Medicaid beneficiaries so far in its redeterminations process. The state has processed 48,000 re-evaluations since beginning the process in February. Read More
Illinois
Illinois Legislature Considers Bill to Create State-based Insurance Exchange. Modern Healthcare reported on May 3, 2023, that the Illinois legislature is considering a bill (House Bill 579) that would allow the state to create a state-based health insurance Exchange. Governor J.B. Pritzker included $10 million in his budget proposal to fund the development cost. Read More
Iowa
Iowa Lawmakers Approve $28 Million to Increase Medicaid Reimbursement Rates in Fiscal 2024. The Iowa Capital Dispatch reported on May 8, 2023, that Iowa lawmakers approved a fiscal 2024 budget that includes an additional $15 million to increase Medicaid reimbursement rates for nursing homes and $13 million to increase rates for mental health and substance use disorder treatment centers. Republican lawmakers voted down a $5.6 million amendment to extend postpartum Medicaid coverage from 60 days to 12 months but said they would consider the extension in 2024. Read More
Kansas
Healthy Blue Kansas Hires President Ahead of Bid on Medicaid Contract. Health Payer Specialist reported on May 8, 2023, that Healthy Blue Kansas, which last year announced its intention to bid on the upcoming Kansas Medicaid managed care procurement, has named Bryan Baier president. Baier previously served stints at Aetna and WellCare, now part of Centene. Healthy Blue Kansas is a joint venture between Blue Cross Blue Shield of Kansas, BCBS of Kansas City, and Elevance Health subsidiary Anthem Partnership Holding. Read More
Kansas Lawmakers Will Not Consider Medicaid Expansion Until 2024. WIBW reported on May 4, 2023, that Kansas lawmakers are not expected to take up Medicaid expansion until 2024, after ending the current legislative session without an expansion bill. Expansion could impact 150,000 individuals in the state. Read More
Massachusetts
Massachusetts to Implement Cost Limits on High-cost Medicaid Drugs. The Eagle Tribune reported on May 8, 2023, that MassHealth will implement drug cost limits through its 340B Drug Pricing Program, effective November 15. According to a report to the legislature’s Joint Committee on Health Care Financing, Medicaid will stop covering 11 drugs that have been estimated to cost more than $100,000 per year, including high-cost drugs to treat cancer, neurological disorders, and other illnesses. Read More
Michigan
HAP, CareSource Form Partnership to Serve Michigan Medicaid Beneficiaries. Health Alliance Plan (HAP) and CareSource announced on May 4, 2023, a definitive agreement to form a joint venture serving Medicaid, dual eligible, and Exchange members. The deal is expected to close in the third quarter of 2023, pending regulatory approval. HAP currently provides Medicaid coverage to 43,000 individuals through its HAP Empowered business. Read More
Missouri
Missouri Legislature Passes Bill to Extend Postpartum Medicaid Coverage. The Associated Press reported on May 5, 2023, that the Missouri legislature passed a bill to extend postpartum Medicaid coverage from 60 days to 12 months. The bill now goes to Governor Mike Parson for his signature. Read More
Nevada
Nevada Senate Considers Bill to Implement Hospital Provider Tax to Increase Medicaid Reimbursement Rates. The Nevada Independent reported on May 10, 2023, that the Nevada Senate is considering a bill (Senate Bill 435) to implement a hospital provider tax of no more than six percent, with the funds being used for supplemental Medicaid payments and increased behavioral health reimbursement rates. State health officials believe the tax could generate $100 million, including federal matching funds. Read More
Rhode Island
Rhode Island Senate Passes Bill to Use Medicaid Funds to Help Homeless Beneficiaries Find Housing. WLNE reported on May 3, 2023, that the Rhode Island Senate passed a bill that would allow the state to use Medicaid funds to help beneficiaries who are homeless find housing. The bill would also create a pilot program to help individuals recover from illness, injury, or medical treatment. The bill now goes to the House for debate. Read More
Rhode Island Awards $85,000 in Grants to Community-based Organizations to Help Medicaid Members Retain Coverage During Redeterminations. The Rhode Island Executive Office of Health and Human Services announced on May 3, 2023, more than $85,000 in grants to 21 community-based organizations to support Medicaid renewals. The organizations will use the funds on outreach, technology, training, and language and cultural competency. Grant applications will continue to be accepted until May 19. Read More
Tennessee
Tennessee Legislature Renews Funding for Medicaid Fraud Unit. WPLN reported on May 8, 2023, that the Tennessee legislature renewed funding for TennCare’s Medicaid fraud unit in its fiscal 2024 budget. Since the unit was created in 2005, it has brought in just under $10 million, far less than the cost of running the unit. Read More
Texas
Texas Senate Passes Bill to Implement Direct Care Spending Requirements for Nursing Homes. State of Reform reported on May 8, 2023, that the Texas Senate passed a bill (Senate Bill 1629) that would require nursing facilities to spend at least 80 percent of medical assistance reimbursements on direct care. The House Human Services Committee will hold a hearing on the bill on May 9. Read More
Virginia
Plan to Cut Medicaid Payments for Preventable ER Visits Is Vacated by Federal Judge. The Richmond Times-Dispatch reported on May 4, 2023, that a federal judge has blocked Virginia from implementing a plan to halve Medicaid payments for hospital emergency room visits that were preventable. The plan, which had received federal regulatory approval, was opposed in a lawsuit filed by Virginia hospitals and physicians. Read More
West Virginia
West Virginia Receives $68 Million in Opioid Settlement with Pharmacy Chain. The Associated Press reported on May 4, 2023, that West Virginia received $68 million in a settlement with pharmacy chain Kroger concerning opioid distribution in the state. Kroger was the last defendant in a lawsuit, which also involved Walmart, Walgreens, CVS, and Rite Aid. West Virginia has received more than $1 billion from lawsuits involving opioids. Read More
National
Behavioral Providers Improperly Billed Medicare $580 Million During First Year of COVID, OIG Finds. The Department of Health and Human Services (HHS) Office of Inspector General (OIG) published in May 2023, an audit that found Medicare improperly paid behavioral providers $580 million for psychotherapy services in the first year of the pandemic from March 2020 through February 2021. Improper payments included $348 million for telehealth services and $232 million for non-telehealth services. Read More
Standardized Plan Design Requirements Increase Number of Exchange Plan Options, KFF Finds. The Kaiser Family Foundation (KFF) reported on May 8, 2023, that the Centers for Medicare & Medicaid Services’ (CMS) requirement that federal Exchange insurers offer standardized plan design (SPD) options has increased the number of plan options available. To decrease the number of options, CMS will limit insurers to no more than four non-standardized plan options for each SPD in 2024 and no more than two for 2025. State Exchanges are not required to offer SPD options, but 10 out of 18 did for 2023. Read More
1.7 Million Medicaid Beneficiaries Could Lose Coverage if Work Requirements are Implemented, KFF Projects. The Kaiser Family Foundation (KFF) reported on May 5, 2023, that 1.7 million Medicaid beneficiaries would potentially lose coverage in 2024 if work requirements are implemented. States could still provide those beneficiaries with coverage but would not receive federal matching funds. The U.S. House passed a bill in April that includes Medicaid work requirements, but it is not expected to pass the Senate. Read More
Industry News
Cano Health Looks to Sell Non-core Assets, Focus on Medicare Advantage. Modern Healthcare reported on May 9, 2023, that Cano Health is looking to sell its non-core assets and focus on its Medicare Advantage (MA) business. The company serves almost 400,000 members, with more than 140,000 in MA plans. Read More
The Pennant Group Acquires Benefit Home Healthcare, Benefit By Your Side. The Pennant Group announced on May 4, 2023, the acquisition of the assets of Colorado-based Benefit Home Healthcare and Benefit By Your Side, which provides home health, private duty, and community health services. Read More
Humana, Longevity Health Partner to Provide SNPs to Medicare Beneficiaries. Longevity Health Plan and Humana announced on May 4, 2023, a partnership to provide Special Needs Plans (SNPs) to Medicare beneficiaries in skilled nursing and senior living facilities. The partnership will launch in South Carolina and Georgia in 2023, with plans to expand to five more states in 2024 and additional states in 2025. Read More
Option Health Care to Acquire Amedisys. Modern Healthcare reported on May 3, 2023, that Option Health Care will acquire Amedisys, a home care and hospice provider, for $3.6 billion. The combined company will generate approximately $6.2 billion in annual revenues and deliver in-home services in 46 states. Read More
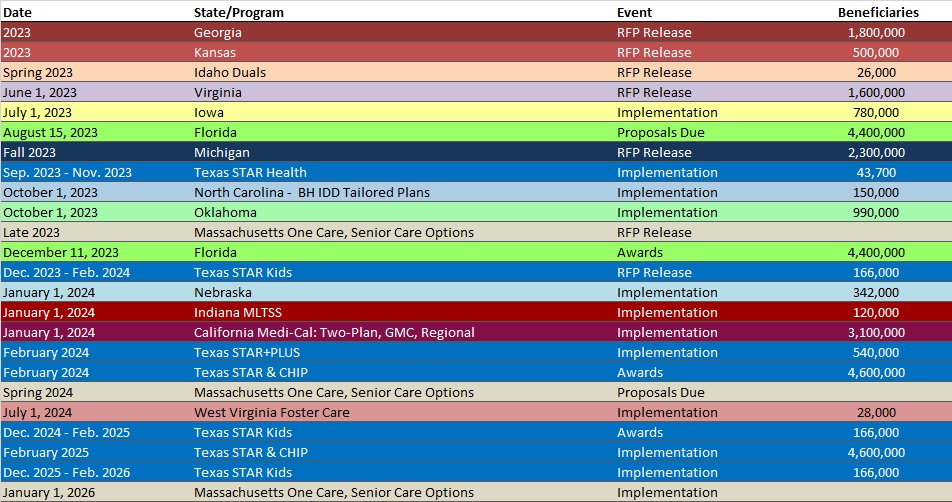
RFP Calendar
HMA News & Events
Upcoming HMA Webinar:
Using 1115 Justice Waivers to Improve Carceral Healthcare Delivery Information. HMA’s 4-part webinar series on 1115 Justice Waivers: Building Bridges of Health for Persons Leaving Carceral Settings, is designed to help plans and other stakeholders improve the long-term health outcomes of individuals. Part 2 will focus on the carceral settings operational healthcare practices, including intake screenings to aid in risk assignment and facilitate community re-entry. Thursday, May 18, 2023, 2 PM ET/11 AM PT. Click here to register.
Opportunities for Opioid Treatment Providers to Improve Patient Outcomes. HMA’s 3-part webinar series on New Rules in Treatment of Opioid Addiction is aimed at helping stakeholders prepare for new federal rules that will change how medications are delivered to persons with opioid use disorders. Part 1 addresses changes in clinical and business practices and payment structures that will enable providers to implement new treatment programs and other flexibilities to improve patient outcomes. Tues. May 23, 2023, 3pm ET. Click here to register.
Highlights from HMA’s 2023 quality conference:
Watch our recap of HMA’s 2023 quality conference to learn key insights and takeaways from leading industry experts here.
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Kentucky Medicaid Managed Care Enrollment is Up 1.1%, May-23 Data
- Minnesota Medicaid Managed Care Enrollment is Up 2.1%, Mar-23 Data
- Mississippi Medicaid Managed Care Enrollment is Up 0.8%, Apr-23 Data
- Missouri Medicaid Managed Care Enrollment is Up 5.4%, Mar-23 Data
- Ohio Medicaid Managed Care Enrollment is Flat, Jan-23 Data
- Oregon Medicaid Managed Care Enrollment is Up 2.1%, Apr-23 Data
- West Virginia Medicaid Managed Care Enrollment is Up 1.1%, Feb-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Mississippi Utilization Management/Quality Improvement Organization IFB and Related Documents, 2023
Medicaid Program Reports, Data, and Updates:
- Hawaii DHS Financial Audit Reports, FY 2017-22
- Iowa External Quality Review Technical Reports, CY 2016-22
- Kentucky Medicaid Managed Care Rate Certifications, FY 2015-22
- Massachusetts MassHealth MCO EQR Technical Reports, 2017-22
- Ohio Medicaid Budget Variance Reports, 2022
- Ohio Medicaid Budget Variance Reports, 2023
- Ohio OBM Monthly Financial Reports, 2022
- Ohio OBM Monthly Financial Reports, 2023
- Ohio Program Integrity Report, 2021
- Vermont Medicaid Program Enrollment and Expenditures Reports, SFY 2018-23
- Washington Apple Health Adult Medicaid CAHPS Reports, 2020-22
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
