HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Health Management Associates Selected as CalAIM Technical Assistance Vendor

- Arizona Delays Implementation of Housing, Health Opportunities Waiver to October 2024

- California Individual Mandate Generates $1.1 Billion in Fines Since 2020

- Georgia Disenrolls 2,200 Medicaid Beneficiaries During April Redeterminations

- Indiana Disenrolls 53,000 Medicaid Beneficiaries During First Month of Redeterminations

- Kentucky Subcommittee Again Finds Deficiencies in Rules Extending Dental, Vision, Hearing Benefits to Medicaid Beneficiaries

- Minnesota Enacts Legislation to Provide Comprehensive Dental Benefits to All Medicaid Beneficiaries

- Missouri Uses Ex Parte Renewal Process for 47 Percent of April Medicaid Eligibility Redeterminations

- Oregon to Disenroll 8,000 Medicaid Beneficiaries Following April Redeterminations

- Rhode Island Releases Medicaid Managed Care RFI; New Procurement Expected Fall 2023

- Wisconsin Could Disenroll Up to 300,000 Medicaid Beneficiaries During Redeterminations, Report Finds

- Medicaid Disenrollments to Date Are Largely for Administrative Reasons, CMS Says

- Medicaid Enrollment to Decrease by More Than 12 Million by 2025, CBO Projects

- CVS/Oak Street Health to Expand Into Arkansas, Iowa, Kansas, Virginia

- AHIP President, CEO to Step Down in October

- Medicaid Directors to Discuss Challenges, Opportunities at HMA Conference in Chicago

In Focus
Health Management Associates Selected as CalAIM Technical Assistance Vendor
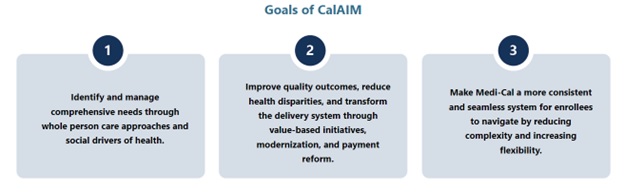
This week, our In Focus section describes a new collaboration between Health Management Associates and the California Department of Health Care Services (DHCS). DHCS has developed a multi-year initiative designed to improve healthcare outcomes and quality through broad delivery, payment, and program reforms known as California Advancing and Innovating Medi-Cal (CalAIM). The plan calls for introducing new programs and making changes to existing programs over the span of five years. CalAIM further expands upon prior initiatives, such as Whole Person Care, the Health Homes Program, and the Coordinated Care Initiative, and strives to integrate California’s delivery systems to better facilitate the Medi-Cal program.
With the rollout of these programs and the vast requirements associated with them, DHCS and California’s Medi-Cal managed care plans now are tasked with the challenge of implementing CalAIM and enabling the participation of community providers and partners in these opportunities. To support these partners, DHCS developed a funding initiative, known as Providing Access and Transforming Health (PATH), to aid in strengthening the capacity and infrastructure of community-based organizations (CBOs), public hospitals, county agencies, and other entities to support CalAIM. This five-year, $1.85 billion initiative includes the creation of a virtual Technical Assistance (TA) Vendor Marketplace that organizations can use to request resources and support from approved vendors through services that the state fully funds.
Health Management Associates (HMA) is recognized as a valued partner to payers, CBOs, public hospitals, and county agencies and has deep expertise in CalAIM policy, operations and implementation. Recognized for our extensive capabilities in the field, HMA is one of only two firms out of 46 vendors that received state approval to serve as a TA vendor for the PATH Technical Assistance Marketplace in all seven domains:
- Domain 1: Building Data Capacity: Data Collection, Management, Sharing, and Use
- Domain 2: Community Supports: Strengthening Services that Address the Social Drivers of Health
- Domain 3: Engaging in CalAIM through Medi-Cal Managed Care
- Domain 4: Enhanced Care Management (ECM): Strengthening Care for ECM Population of Focus
- Domain 5: Promoting Health Equity
- Domain 6: Supporting Cross-Sector Partnerships
- Domain 7: Workforce
HMA also has expertise in and hands-on experience with addressing the unique challenges facing providers and partner agencies in rural communities. Please visit the PATH Technical Assistance Marketplace to access TA resources that can help strengthen capacity to provide high-quality ECM and community supports services for Medi-Cal members.
For more information, contact: Jonathan Freedman, Regional Vice President.
HMA Roundup
Arizona
Arizona Delays Implementation of Housing, Health Opportunities Waiver to October 2024. The Arizona Health Care Cost Containment System announced on May 24, 2023, that it is delaying implementation of its Housing and Health Opportunities Section 1115 waiver demonstration to October 1, 2024. The program will address health-related social needs for beneficiaries with a serious mental illness who are leaving a carceral setting or have additional chronic health conditions. Once implemented, the state will reimburse providers for up to six months of medically necessary transitional housing and services. Read More
California
California Individual Mandate Generates $1.1 Billion in Fines Since 2020. KFF Health News reported on May 30, 2023, that California’s individual mandate has generated an estimated $1.1 billion in fines since it began in 2020, according to Governor Gavin Newsom. The mandate is projected to bring in another $700 million over the next two years. State lawmakers want the funds to offset out-of-pocket costs for Californians purchasing coverage on the state Exchange. However, the Newsom administration has the money going to the state’s general fund. Read More
Colorado
Colorado Enacts Law Increasing Flexibility in Setting Medicaid Rates for Nursing Facilities. Heart of the Rockies Radio reported on May 30, 2023, that Colorado Lieutenant Governor Dianne Primavera signed a bill (House Bill 23-1228) aimed at increasing flexibility in setting Medicaid rates for nursing facilities. Under the law, nursing facility reimbursement rate methodology will be regulated by the Department of Health Care Policy & Financing, instead of set by state statute. Read More
District of Columbia
District of Columbia Council Considers Bill to Reform Prior Authorization Process. The Washington Post reported on May 28, 2023, that the D.C. Council is considering a bill (Council Bill 250124) that would set deadlines for insurers to respond to prior authorization requests and appeals, allow denials only by a District-licensed physician with the same specialty as the patient’s doctor, make approvals last at least a year, and honor approvals for 60 days when a patient changes plans. The legislation is supported by the American Medical Association. Read More
Georgia
Georgia Disenrolls 2,200 Medicaid Beneficiaries During April Redeterminations. The Georgia Department of Community Health submitted on May 8, 2023, its April report to the Centers for Medicare & Medicaid Services on the Medicaid unwinding process, which showed that 2,244 Medicaid beneficiaries were disenrolled. The vast majority were disenrolled for procedural reasons, including failure to respond. About ten were determined ineligible and transferred to the Exchange. More than 66,100 beneficiaries had their coverage renewed in April.
Illinois
Illinois Governor to Sign Legislation Creating State-based Insurance Exchange. Health News Illinois reported on May 30, 2023, that Illinois Governor JB Pritzker is expected to sign House Bill 579 to create a state-based health insurance Exchange. Under the plan, an initial version would be operational on the federal platform by plan year 2025, with a final version on a state-based platform ready for the 2026 plan year. Read More
General Assembly Approves $50 Million to Increase Medicaid Reimbursement Rates. Health News Illinois reported on May 30, 2023, that the Illinois General Assembly approved a $50.6 billion budget that includes $50 million to increase Medicaid reimbursement rates. The budget also includes $550 million to fund the Health Benefits for Immigrant Seniors and Adults program, which provides healthcare to individuals not eligible for Medicaid due to citizenship status. Governor JB Pritzker is expected to sign the budget into law. Read More
Indiana
Indiana Medicaid Beneficiaries Are Less Satisfied with Quality of Care Compared to National Average, Report Finds. The Indiana Capital Chronicle reported on May 31, 2023, that approximately 62 percent of Indiana Medicaid beneficiaries are mostly or completely satisfied with the quality of care they receive, compared to about 72 percent nationally, according to a report from the Center for Popular Democracy, Make the Road New York, and People’s Action Institute. The report also found that 48 percent of beneficiaries found applying for coverage to be challenging, and 43 percent had difficulty renewing coverage. The report surveyed nearly 3,000 Medicaid beneficiaries between September 2022 and February 2023. Read More
Indiana Disenrolls 53,000 Medicaid Beneficiaries During First Month of Redeterminations. The Indiana Capital Chronicle reported on May 25, 2023, that Indiana disenrolled nearly 53,000 beneficiaries during the first month of eligibility redeterminations. Of these, 6,089 were disenrolled due to ineligibility and 46,896 for procedural reasons. The redeterminations period will continue until April 2024. An estimated 300,000 to 400,000 beneficiaries are projected to lose coverage. Read More
Kentucky
Kentucky Subcommittee Again Finds Deficiencies in Rules Extending Dental, Vision, Hearing Benefits to Medicaid Beneficiaries. Kentucky Health News reported on May 29, 2023, that the Kentucky legislature’s Administrative Regulation Review Subcommittee again found deficiencies in proposed regulations aimed at extending dental, vision, and hearing benefits to Medicaid beneficiaries. The benefits, which impact 900,000 Medicaid beneficiaries, will remain in place until the next legislative session. Public comments are being accepted until May 31. Read More
Minnesota
Minnesota Lawmakers Pass Bill to Review Health Care Cost Growth. Politico reported on May 30, 2023, that Minnesota lawmakers passed a bill that requires state health officials to review health care cost growth. An earlier version proposed fines for out-of-control cost growth. Lawmakers scaled down the bill after Mayo Clinic said they would pull $4 billion in new hospital investments. Read More
Minnesota Enacts Legislation to Provide Comprehensive Dental Benefits to All Medicaid Beneficiaries. The Minnesota Dental Association announced on May 24, 2023, that Minnesota Governor Tim Walz signed a bill to provide comprehensive dental benefits to Medicaid beneficiaries, regardless of age, effective 2024. The bill is part of the state’s fiscal 2025 budget. Read More
Missouri
Missouri Uses Ex Parte Renewal Process for 47 Percent of April Medicaid Eligibility Redeterminations. The Missouri Independent reported on May 25, 2023, that Missouri used an ex parte renewal process for 47 percent of April Medicaid redeterminations, compared to 10 percent pre-COVID. State officials project that 200,000 Missourians could lose coverage during redeterminations. Read More
New Hampshire
New Hampshire Senate Committee Adds Clause to Budget Bill to Reauthorize Medicaid Expansion for 7 Years. NH Journal reported on May 30, 2023, that the New Hampshire Senate Finance Committee added a clause to Senate Bill 263 that would reauthorize Medicaid expansion for seven years. The bill is part of the overall fiscal 2025 budget bill. Currently, Medicaid expansion is set to end in 2024 if it is not reauthorized. The bill now heads to the House Finance Committee. Read More
Oregon
Oregon to Disenroll 8,000 Medicaid Beneficiaries Following April Redeterminations. The Lund Report reported on May 25, 2023, that Oregon identified 8,000 Medicaid beneficiaries who are no longer eligible for coverage following April redeterminations. Another 47,000 were asked to provide additional information. The state renewed coverage for more than 133,000 beneficiaries and sent renewal packets to another 13,000. As for May, approximately two-thirds of beneficiaries reviewed to date will keep their coverage. Overall, the state expects about 300,000 Medicaid beneficiaries to lose coverage during determinations. Read More
Rhode Island
Rhode Island Releases Medicaid Managed Care RFI; New Procurement Expected Fall 2023. The Rhode Island Executive Office of Health and Human Services released on May 30, 2023, a request for information (RFI) for its Medicaid managed care program. The RFI is seeking feedback on new elements of the program, including the inclusion of integrated dual eligible special needs plans and the inclusion of long-term services and supports as an in-plan benefit for all beneficiaries. The state initially released a request for qualifications (RFQ) in November 2021, but it was cancelled. The new RFQ will be released in fall 2023. Current incumbents are Neighborhood Health Plan of Rhode Island, Tufts Health Public Plan, and UnitedHealthcare Community Plan. Responses are due on June 27. Read More
Wisconsin
Wisconsin Could Disenroll Up to 300,000 Medicaid Beneficiaries During Redeterminations, Report Finds. The Milwaukee Journal Sentinel reported on May 24, 2023, Wisconsin could disenroll an estimated 300,000 Medicaid beneficiaries during redeterminations, according to a report from the Robert Wood Johnson Foundation and Urban Institute. Wisconsin will begin reviewing renewal applications in June 2023. Read More
National
U.S. Representative Reintroduces Bill to Provide Medicaid Coverage to Eligible Individuals Being Detained Pretrial. The Dayton Daily News reported on May 30, 2023, that U.S. Representative Mike Turner (R-OH) reintroduced the Due Process Continuity of Care Act that would allow eligible individuals who are being detained pretrial to keep their Medicaid coverage. The bill would also authorize $50 million in planning grant funding to be distributed to state, county, and local jails to implement the new policy and improve the quality of care provided. Read More
Most Medicaid Beneficiaries Losing Coverage During Redeterminations Will Transition to Employer Plans, Report Says. InsuranceNewsNet reported on May 30, 2023, that the majority of individuals losing coverage following Medicaid redeterminations will transition to employer-sponsored coverage, according to a report from AHIP and NORC. The report says that 3.8 million Medicaid beneficiaries (or about 21 percent of those who lose Medicaid coverage during redeterminations) will end up uninsured. Read More
Medicaid Disenrollments to Date Are Largely for Administrative Reasons, CMS Says. Modern Healthcare reported on May 30, 2023, that about eight in 10 Medicaid disenrollments following eligibility redeterminations are for administrative reasons, according to the Centers for Medicare & Medicaid Services (CMS). The figure is based on the state redeterminations data to date. Administrative reasons include beneficiaries not responding to state outreach efforts. Read More
80 Percent of Americans Will Be Unable to Cover Long-term Care Costs, Report Finds. WUSF Public Media reported on May 30, 2023, that 80 percent of Americans will be unable to cover the cost of two years of long-term care, including nursing homes, according to a February issue brief from the National Council on Aging. The report also found that about half of adults over 65 will require long-term care. Read More
Medicaid, CHIP Enrollment is Nearly 93.4 Million in February 2023. The Centers for Medicare & Medicaid Services (CMS) announced on May 30, 2023, that enrollment in Medicaid and the Children’s Health Insurance Program (CHIP) was nearly 93.4 million in February 2023, an increase of almost 403,000 from January 2023. Medicare enrollment was more than 65.6 million, up more than 99,000 from January 2023, including nearly 31.7 million in Medicare Advantage plans. More than 12 million Medicare-Medicaid dual eligibles are counted in both programs. Read More
Debt Ceiling Agreement Does Not Include Medicaid Work Requirements. The New York Times reported on May 29, 2023, that the debt ceiling deal reached by President Biden and U.S. House Speaker Kevin McCarthy (R-CA) does not include Medicaid work requirements. The deal still needs to pass in the House. Read More
Medicaid Enrollment to Decrease by More Than 12 Million by 2025, CBO Projects. Forbes reported on May 25, 2023, that Medicaid enrollment will decrease by more than 12 million by 2025, according to estimates from the Congressional Budget Office (CBO). About 15.5 million will lose coverage following redeterminations, offset slightly by new enrollees. CBO also estimates that if enhanced Exchange subsidies expire in 2025, then 4.9 million fewer people will enroll in coverage. Read More
KFF Releases Results from Behavioral Health Survey of State Medicaid Programs. The Kaiser Family Foundation (KFF) released on May 25, 2023, the findings from its Behavioral Health Survey of state Medicaid programs, which was a supplement to the 22nd annual budget survey of Medicaid officials. The findings focused on how states administer their behavioral health programs, what managed care arrangements they use, how they promote the delivery of integrated behavioral and physical health care, and how they are monitoring behavioral health data. Read More
States Face Obstacles to Implementing Crisis Service Coverage, Report Finds. The Kaiser Family Foundation (KFF) reported on May 25, 2023, that most states are experiencing or expect to experience at least one obstacle to implementing crisis services, according to a survey. The survey also found that most states do not cover all three of the core crisis services for adults (crisis hotlines, mobile crisis units, and crisis stabilization) under fee-for-service Medicaid, but most states cover at least one. Read More
CMS Reports to Congress on State Use of SUD Planning Grants. The Centers for Medicare & Medicaid Services (CMS) reported to Congress on May 25, 2023, that states are using funds from substance use disorder (SUD) planning grants to better understand of SUD prevalence, enhance provider capacity, expand medication-assisted treatment (MAT) and other best practices, improve reimbursements, and enhance integration and care coordination. The fifteen states selected to receive planning grants were Alabama, Connecticut, Delaware, the District of Columbia, Illinois, Indiana, Kentucky, Maine, Michigan, Nevada, New Mexico, Rhode Island, Virginia, Washington, and West Virginia. The findings are based on data from September 30, 2019 to October 31, 2020. Read More
Medicaid Telehealth Coverage Requirements Increase Access to Services for Beneficiaries, Study Finds. MHealth Intelligence reported on May 25, 2023, that Medicaid telehealth coverage requirements led to increases in same-day appointments and access to needed care, according to a study from Health Services Research. The study analyzed survey data from the 2013-19 Association of American Medical Colleges Consumer Survey of Health Care Access, including 4,492 Medicaid beneficiaries and 15,581 privately insured adults under 65. Read More
65 Percent of Medicaid Beneficiaries Are Unsure Whether States Can Disenroll Ineligible Individuals During Redeterminations, KFF Finds. The Kaiser Family Foundation (KFF) reported on May 24, 2023, that 65 percent of Medicaid beneficiaries were unsure whether states could disenroll people who are no longer eligible or did not complete the renewal process, according to a KFF survey. The survey also found that 47 percent of beneficiaries have never been through the renewal process, and 33 percent said they have not provided updated contact information to their state Medicaid agency in the past year. Additionally, 85 percent indicated that it would be helpful to have a navigator help with the process. Read More
Industry News
CVS/Oak Street Health to Expand Into Arkansas, Iowa, Kansas, Virginia. Health Payer Specialist reported on May 31, 2023, that primary care clinic operator Oak Street Health, a CVS Health company, will expand into Arkansas, Iowa, Kansas, and Virginia. After the expansion, Oak Street Health will operate in 25 states. The new clinics are scheduled to open in summer 2023. Read More
AHIP President, CEO to Step Down in October. Modern Healthcare reported on May 24, 2023, that Matt Eyles, AHIP president and chief executive, will step down on October 2, 2023. Eyles has held the position for five years. The AHIP board will launch a search for his replacement. Read More
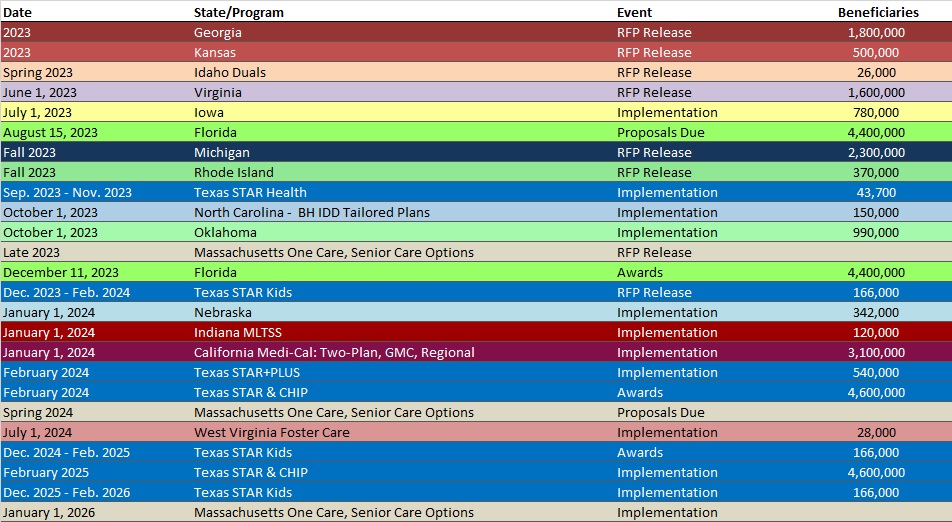
RFP Calendar
HMA News & Events
Upcoming HMA Conference:
Medicaid Directors to Discuss Challenges, Opportunities at HMA Conference in Chicago
Medicaid directors from California, Illinois, Mississippi, and Nevada will address key opportunities and challenges facing state Medicaid programs during HMA’s 2023 annual conference, October 30-31, at the Fairmont Chicago Millennium Park. The theme of this year’s event is Innovations in Publicly Sponsored Health Care: How Medicaid, Medicare, and Marketplaces Are Driving Value, Equity, and Growth.
Speakers will include Jacey Cooper, State Medicaid Director, Chief Deputy Director for Health Care Programs, California Department of Health Care Services; Kelly Cunningham, Medicaid Administrator, Division of Medical Programs, Illinois Department of Healthcare and Family Services; Drew Snyder, Executive Director, Mississippi Division of Medicaid; Stacie Weeks, Administrator/Medicaid Director, Nevada Department of Health and Human Services Division of Health Care Financing and Policy.
Early bird registration ends July 31. For additional information, visit the conference website at https://conference.healthmanagement.com/ or contact Carl Mercurio at [email protected]. Group rates, government discounts, and sponsorships are available.
Upcoming HMA Webinars:
Opportunities for State Payers to Improve & Align Incentives for Treatment of Substance Use Disorder. HMA’s 3-part webinar series on New Rules in Treatment of Opioid Addiction is aimed at helping stakeholders prepare for new federal rules that will change how medications are delivered to persons with opioid use disorders. Part 2 highlights Opportunities for State Payers to Improve & Align Incentives so providers can expand access to treatment enabled by new federal regulations that encourage patient-centered care. Tuesday, June 6, 2023, 3pm ET. Click here to register.
Youth Mental Health Access: School-Based Intervention Strategies. The youth behavioral health crisis has resulted in a cascade of federal funding, advisories, and overall opportunities to improve resources to help kids. This webinar will present the Dialectical Behavioral Therapy (DBT) STEPS for Adolescents model, which is a low cost, high impact approach that empowers schools to intervene and support well-being and resiliency before students are in crisis, self-harming, or suicidal. Wednesday, June 14, 2023, 1 pm ET. Click here to register.
1115 Justice Waivers: Connecting Community Partners to Improve Transitions of Care. Part 3 of HMA’s webinar series, 1115 Medicaid Justice Demonstration Waivers: Bridging Healthcare, will focus on optimizing key partnerships before, during and after transition from a carceral setting into the community to ensure the best outcomes for individuals eligible for 1115 approved waiver services. Thursday, June 15, 2 pm ET. Click here to register.
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Alabama SNP Membership at 135,117, Mar-23 Data
- Arizona SNP Membership at 144,459, Mar-23 Data
- Arkansas SNP Membership at 90,381, Mar-23 Data
- Connecticut SNP Membership at 96,597, Mar-23 Data
- Delaware SNP Membership at 20,623, Mar-23 Data
- Michigan Medicaid Managed Care Enrollment is Flat, Mar-23 Data
- Michigan Dual Demo Enrollment is Down 7.3%, Mar-23 Data
- Virginia Medicaid Managed Care Enrollment is Up 3.5%, Apr-23 Data
- Virginia Medicaid MLTSS Enrollment is Up 1.3%, Apr-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Pennsylvania Community HealthChoices RFI and Responses, 2023
- Rhode Island Medicaid Managed Care RFI, May-23
Medicaid Program Reports, Data, and Updates:
- Arizona Medicaid Managed Care Capitation Rates and Actuarial Certification, 2023
- Georgia PHE Medicaid Unwinding Monthly Report to CMS, Apr-23
- HMAIS Medicaid Managed Care Rate Certifications Inventory
- Iowa Medicaid Managed Care Rate Certification and Appendices, FY 2023
- Iowa Medical Assistance Advisory Council Meeting Materials, Mar-23
- New Hampshire External Quality Review Organization (EQRO) Technical Reports, SFY 2018-22
- Pennsylvania Medical Assistance Advisory Committee (MAAC) Meeting Materials, May-23
- Texas Medicaid Managed Care and CHIP External Quality Review Reports, 2016-22
- Texas Quarterly Reports from the HHS Ombudsman Managed Care Assistance Team, FY 2019-23
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio at [email protected].
