HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Takeaways from the Early Medicaid Unwinding Actions

- In Focus: HMA: What We're Watching

- Medicaid Redeterminations New: Arizona, California, Colorado, Idaho, Indiana, Iowa, Kentucky, Louisiana, Michigan, Nevada, North Carolina, North Dakota. Texas, West Virginia, Wyoming

- Arkansas Submits Request for Medicaid Expansion Work Requirements

- Georgia Cancels RFQC for Medicaid Managed Care Plans

- Iowa Enacts Legislation Tightening Medicaid Eligibility Verification

- Nevada Medicaid Drug Spending Rose 126 Percent from 2017 to 2022

- New Mexico to Extend Medicaid Managed Care Contracts Additional 6 Months

- New Mexico to Expand Access to Medicaid Payments for Medical, Behavioral Health Services in Schools

- Pennsylvania Seeks to Implement Selective Contracting for IDD Residential, Supports Coordination Services

- South Dakota Receives Federal Approval to Implement Medicaid Expansion in July

- Elevance Health Names Natalie Cooper President of Amerigroup Tennessee

- Texas Names Emily Zalkovsky as State Medicaid Director

- Merck Seeks Injunction to Block Medicare Drug Negotiation Program

- UnitedHealth/Optum Makes Unsolicited $3.26 Billion Bid for Amedisys

In Focus
Takeaways from the Early Medicaid Unwinding Actions
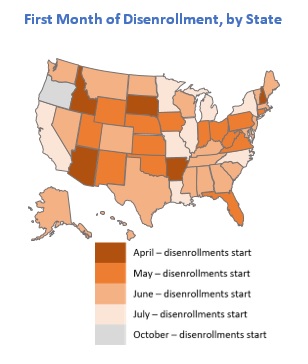
This week, our In Focus checks in on the Medicaid unwinding work and key issues HMA experts are watching as more states resume their normal policies and processes for determining eligibility. A total of 19 states started disenrollments effective for April or May coverage, and 22 additional states plan to start ending coverage this month. States are scheduled to submit the next monthly report by June 8, 2023.
Background
As explained in earlier In Focus articles, (here, here and here) federal COVID-19 relief laws allowed states to receive higher federal funding for Medicaid as long as the state did not terminate Medicaid coverage for anyone enrolled in Medicaid during the public health emergency (PHE). One result of the continuous coverage policy was sustained growth in Medicaid enrollment; more than 21 million additional individuals were continuously enrolled in Medicaid for up to three years between February 2020 and March 2023. In December 2022, Congress ended the Medicaid continuous coverage policy after March 31, 2023. States were allowed to begin processing redeterminations as early as February 2023 and start disenrolling ineligible individuals as early as April 2023.
Preparations for the Medicaid unwinding have been under way for well over two years. The Centers for Medicare & Medicaid Services (CMS), states, Medicaid health plans, providers, beneficiary advocates, and other interested stakeholders have been working to ensure that the policies, outreach, and assistance are in place to support this massive eligibility renewal and redetermination initiative.
What Do We Know… Or Not Know?
Most of the available forecasts project between 10-15 million enrollees will lose Medicaid coverage. The Health Management Associates (HMA) insurance mix model projects that more than 10 million of the approximately 90 million Medicaid enrollees are at risk for disenrollment. HMA’s model illustrates the variety in state approaches to managing the resumption of eligibility redeterminations as well as key insights related to the differential impact by Medicaid eligibility categories.
 Based on published information, the number of individuals who were disenrolled from Medicaid in April through May is likely to approach 500,000. In these early days of the unwinding period, HMA experts are closely reviewing the reports and engaging with key stakeholders in individual states. Several issues already are garnering more attention, such as the impact on child enrollment, churn and experiences in states using the extended reconsideration period flexibility, among others. Stakeholders will want to monitor how these and other program nuances evolve over the next year.
Based on published information, the number of individuals who were disenrolled from Medicaid in April through May is likely to approach 500,000. In these early days of the unwinding period, HMA experts are closely reviewing the reports and engaging with key stakeholders in individual states. Several issues already are garnering more attention, such as the impact on child enrollment, churn and experiences in states using the extended reconsideration period flexibility, among others. Stakeholders will want to monitor how these and other program nuances evolve over the next year.- We do not yet have robust or consistent data from the states that have resumed their normal processes for determining eligibility. States must submit disenrollment reports to CMS each month, and CMS must publish this information. The states are not, however, required to publish this information on their website. While some states have chosen to publish the data or plan to do so, there is no consistent approach to the specific data states post. For example, while most states publishing a state data dashboard are sharing the number of renewals they are processing each month, only slightly more than half also are sharing the number of renewals resulting in coverage terminations.
CMS is not expected to publish the state data before the end of June. Once this information is available, the state unwinding reports may provide a more comprehensive and consistent picture of enrollment over the next year.
In addition, the total number of “procedural terminations” currently is difficult to determine. Lack of consistent public reporting creates gaps in the data about the number of individuals disenrolled because they did not provide a timely response to the state’s request for more information (or for other procedural reasons). As Medicaid stakeholders know, the procedural disenrollment number is critical because these individuals could still be eligible for the program.
- Early disenrollment numbers should be analyzed carefully and in the context of the state. As noted earlier, the full eligibility renewal and disenrollment reports are unavailable at this time. We do know, however, that the available data is best analyzed in the context of the state’s unwinding plan (e.g., how the state is sequencing its eligibility reviews). The sequencing, pace, staffing, messaging consistency, partner outreach and assistance, and other factors will result in variation in state experiences. States are actively analyzing the data as the information is released and considering course corrections that may be needed, which could affect enrollment.
- Ongoing federal and state collaboration is improving preparations and allowing partners to address concerns as they arise. CMS and states have been transparent about the magnitude of the Medicaid unwinding and the fact that challenges will be inevitable throughout this process. The experiences reported by the first tranche of states to begin their unwinding period reinforce those points. They also provide important lessons for states that are or will shortly resume normal eligibility operations.
What to Watch
HMA’s experts are working with states, Medicaid health plans and their partners, providers, and advocacy organizations to identify and implement solutions to some of the known challenges. We also are looking ahead to forthcoming data, qualitative input, and other important developments that may inform federal and state policies and operations beyond the unwinding period.
- Unwinding trends. Though it is too early to definitively identify trends, HMA experts are monitoring the early state data, and we are prepared to analyze the CMS reports once they are published. We anticipate the CMS published data could be more instructive regarding the impact of the unwinding on enrollment, including states or regions that could benefit from additional outreach and assistance strategies, disproportionate impacts on certain demographic groups, new flexibilities that states may want to consider, and steps that health plans, hospitals and health systems, providers, and other partners could advance.
- State operational plans. As of late May, CMS officials reported they have not asked any state Medicaid agency to develop a corrective action plan related to the unwinding; however, this does not mean that federal officials do not have concerns about the experiences and data being reported out of certain states. States, their business partners, and advocates will all benefit from monitoring shifts in state plans, potential future CMS resources and direction to states such as additional reporting or modifying eligibility processes.
- Coverage Program Transitions. Significant attention has been appropriately placed on the Medicaid disenrollment numbers. HMA experts also are closely watching for new data on the number of individuals who successfully transition and enroll in qualified health plans offered in the Health Insurance Marketplaces. In the short term, the Medicaid unwinding could have a notable impact on total enrollment in Marketplace plans as well as provider payer mix. This could affect longer-term policy, strategy, and operational decisions for officials at the federal and state levels, managed care organizations, providers, and other stakeholders. For example:
- Health insurers should assess the opportunity to participate in the Marketplace program. Other insurers may need to develop new strategies to remain competitive in the Marketplace.
- Providers have similar assessments to conduct related to changes in the number of uninsured people to whom they deliver care, as well as their payer mix and the Marketplace plan networks in which they participate.
- Policymakers may revisit Marketplace regulations and standards in response to enrollment growth, enrollee demographics, and acuity of enrollees in Marketplace plans.
Medicaid agencies, health plans, all types of Medicaid providers, and advocacy organizations should continue to analyze their immediate needs during the Medicaid unwinding. They should also be planning to identify and incorporate lessons from this transition period, as well as preparing for policy and operations changes in the post-unwinding environment.
Please contact HMA experts Jane Longo, Andrea Maresca, and Lora Saunders.
HMA: What We're Watching
On June 8, 2023, the Health Care Payment Learning & Action Network (LAN) will hold a virtual meeting focused on accountable primary care. The LAN — an initiative supported by the Centers for Medicare & Medicaid Services (CMS) Innovation Center — is a group of public and private health care leaders that provide thought leadership, strategic direction, and ongoing support to accelerate our care system’s adoption of alternative payment models (APMs). During the session, CMS Administrator Chiquita Brooks-LaSure and the Innovation Center’s Deputy Administrator and Director Liz Fowler will share their vision for accountable primary care.
Over the past several months CMS leaders have discussed their intent to accelerate the transition to value-based care and more accountable primary care. They have identified key principals and hinted at certain components of a potential new primary care model. Additionally, the Innovation Centers’ earlier strategy documents have highlighted the imperative to include payers beyond Medicare, importantly Medicaid and commercial insurers, in models to achieve person-centered accountable and equitable care.
This meeting is notable because the Innovation Center’s models can drive transformational shifts in health care delivery and payment across public and private payers at the system and practice levels. Providers, health systems, insurers, and other interested stakeholders will want to closely monitor the LAN discussion for more information about CMS’ evolving thinking and future opportunities related to a potential model for accountable primary care. HMA experts are available to work with health care organizations and stakeholders to interpret and respond to developments flowing from the LAN session.
LAN meeting registration and information is available here.
HMA Roundup
Arizona
Arizona Disenrolls 19,600 Medicaid Beneficiaries During April Redeterminations. The Arizona Health Care Cost Containment System announced on May 8, 2023, that more than 19,600 Medicaid beneficiaries were disenrolled during April redeterminations. The state renewed coverage for almost 162,700 beneficiaries.
Arkansas
Arkansas Submits Request for Medicaid Expansion Work Requirements. The Arkansas Democrat Gazette reported on June 4, 2023, that the Arkansas Department of Human Services submitted a proposed amendment to its Medicaid expansion program, ARHOME, to implement work requirements. The proposal would require beneficiaries to work, volunteer, or enroll in training or classes. Failure to do so would not result in a loss of coverage; instead, members would be shifted from Medicaid-funded private health coverage to traditional Medicaid fee-for-service. In May 2023, ARHOME covered nearly 313,000 beneficiaries. Read More
Connecticut
Connecticut Budget Includes $3 Million to Extend HUSKY Coverage to Undocumented Children Up to Age 15. Connecticut Governor Ned Lamont announced on June 5, 2023, an agreement to budget $3 million over fiscal years 2024 and 2025 to extend HUSKY Medicaid coverage to undocumented children from age 12 to 15. The budget also raises income eligibility for the HUSKY C Medicaid programs for individuals who are aged, blind, or disabled to 105 percent of poverty. Other budgeted items include $3 million to evaluate Medicaid rates, $32 million for Federally Qualified Health Centers, and $10 million to provide two months of premium payments for individuals who are eligible for Exchange subsidies. The General Assembly is expected to vote on the agreement before midnight on June 7. Read More
Georgia
Georgia Cancels RFQC for Medicaid Managed Care Plans. The Georgia Department of Community Health announced on June 2, 2023, the cancellation of its request for qualified contractors (RFQCs) from Medicaid managed care plans for the Georgia Families and Georgia Families 360 program. The state plans on releasing a request for proposals for Georgia Families and Georgia Families 360 in the coming months, which will address qualification requirements. Read More
Illinois
Illinois Legislature Approves Medicaid Rate Increase for Supportive Living, FQHCs. Illinois Radio Network reported on June 2, 2023, that the Illinois legislature passed a state budget bill that includes $317 million to increase Medicaid reimbursement rates for supportive living facilities, federally qualified health centers, and care for medically fragile technologically dependent children and their full-time nurses. The budget also funds the Health Benefits for Immigrant Seniors and Adults program, which provides healthcare to individuals not eligible for Medicaid due to citizenship status. Read More
Iowa
Iowa Enacts Legislation Tightening Medicaid Eligibility Verification. The Des Moines Register reported on June 1, 2023, that Iowa Governor Kim Reynolds signed a bill (Senate File 494) that directs the state Department of Health and Human Services to create a computerized income, asset, and eligibility verification system for public assistance programs, including Medicaid. The system would check additional sources to determine eligibility and would also require Medicaid beneficiaries to verify their identity online, in-person or by phone. Read More
Louisiana
Louisiana April Medicaid Redeterminations Reveal 55 Percent of Beneficiaries Must Update Eligibility Information. The Louisiana Illuminator reported on June 6, 2023, that Louisiana conducted Medicaid eligibility redeterminations on 162,000 beneficiaries in April, with 45 percent renewed and 55 percent sent notices seeking updated information. Those found ineligible will lose coverage in July. Read More
Maine
Maine Addresses COVID-19 Disparities Using Grant Funds. The Maine Department of Health and Human Services released on May 31, 2023, a progress update on efforts to advance health equity in communities at higher risk of COVID-19 and address systemic health inequities revealed during the pandemic. Efforts, which were funded by $32 million in federal grants, included investment in tribal communities and community-based organizations, addressing the end of the Medicaid continuous coverage requirement, bolstering EMS community paramedicine and systems of care, expanding COVID testing, and other initiatives. Read More
Michigan
Michigan Initiated 30,000 Medicaid Renewals During April Redeterminations. The Michigan Department of Health and Human Services submitted on May 9, 2023, its April report to the Centers for Medicare & Medicaid Services on the Medicaid redeterminations process, which said more than 30,000 beneficiaries had a renewal initiated in April. The state will not begin disenrolling beneficiaries until July.
Nevada
Nevada Medicaid Drug Spending Rose 126 Percent from 2017 to 2022. The Nevada Current reported on June 7, 2023, that Nevada’s Medicaid drug spending increased 126 percent to $967.4 million between 2017 and 2022, according to the state Department of Health and Human Services’ annual drug transparency report. The number of claims increased by 59.2 percent to more than 8 million, during the same period. Read More
New Mexico
New Mexico to Extend Medicaid Managed Care Contracts Additional 6 Months. The Santa Fe New Mexican reported on June 4, 2023, that the New Mexico Human Services Department will extend the current Medicaid managed care contracts, which are currently set to expire at the end of 2023, for an additional six months. The state cancelled its request for proposals in January and has not issued a new one yet. Current incumbents are Centene/Western Sky Community Care, Blue Cross and Blue Shield of New Mexico, and Presbyterian Health Plan. Read More
New Mexico to Expand Access to Medicaid Payments for Medical, Behavioral Health Services in Schools. The Santa Fe New Mexican reported on June 4, 2023, that New Mexico will expand access to Medicaid payments for medical and especially behavioral health services in schools, after receiving federal approval to serve students beyond those with an Individualized Education Program (IEP). An IEP is a federally required plan for special education students. There are nearly 245,000 Medicaid covered school-age children in the state that schools will now be able to serve. Read More
North Dakota
North Dakota Disenrolls 4,400 Medicaid Beneficiaries During May Redeterminations. North Dakota Health and Human Services announced on June 5, 2023, the disenrollment of about 4,400 Medicaid beneficiaries during May redeterminations. According to the state, of the 13,100 beneficiaries who were due for renewal, only about 33 percent returned the appropriate forms. The state is urging beneficiaries to return their renewal forms within 30 days to retain coverage. Read More
North Dakota Seeks Comments on Plan to Increase Access to Waiver Services for Medically Fragile Children. The North Dakota Health and Human Services announced on June 1, 2023, that it is seeking public comments on a draft amendment for its 1915c waiver for medically fragile children to increase the number of slots by 25 and to raise the funding cap to $25,300 per fiscal year. Public comments will be accepted until June 30. The state is planning for an effective date of October 1. Read More
Oklahoma
OK Seeks Public Comments on 1915c HCBS ADvantage Waiver Amendment. The Oklahoma Health Care Authority (OHCA) announced on June 6, 2023, that it is seeking an amendment to its Section 1915c HCBS ADvantage Waiver, which provides alternatives to nursing homes for SoonerCare-eligible beneficiaries who are 65 and older or disabled. The amendment will increase reimbursement rates for remote support services to match corresponding rates of other Oklahoma 1915c waivers, lower the eligibility age from 21 to 19 years of age, and increase home delivered meals to two per day. Public comments are open until July 5, 2023. Read More
Pennsylvania
Pennsylvania Eliminates Medicaid Provider Application Backlog. Go Erie reported June 7, 2023, that the Pennsylvania Department of Human Services (DHS) has eliminated a backlog of Medicaid provider applications. DHS is required to revalidate Medicaid providers every five years. As of January, there was still a backlog of more than 35,000 applications. Read More
Pennsylvania Seeks to Implement Selective Contracting for IDD Residential, Supports Coordination Services. The Pennsylvania Office of Developmental Programs (ODP) announced on May 24, 2023, that it is seeking public comments on a plan to implement selective contracting for intellectual and developmental disabilities providers for residential services and behavioral supports coordination. The proposal would implement two statewide 1915b waivers eliminating the requirement that Pennsylvania must contract with any “willing and qualified” provider. The public comment period is open through July 10.
South Dakota
South Dakota Receives Federal Approval to Implement Medicaid Expansion in July. The Centers for Medicare & Medicaid Services (CMS) announced on May 23, 2023, approval of a state plan amendment that will allow South Dakota to implement Medicaid expansion on July 1. South Dakota is the 39th state to expand Medicaid. Read More
Tennessee
Tennessee Supreme Court Voids $50 Medicaid Payment Cap for Emergency Room Doctors. The Tennessee Lookout reported on June 6, 2023, that the Tennessee Supreme Court ruled that a $50 cap on Medicaid payments to emergency room doctors who treat patients for non-emergency conditions is void. According to the ruling, TennCare failed to follow the rules in setting the cap. Read More
Elevance Health Names Natalie Cooper President of Amerigroup Tennessee. Elevance Health announced on June 1, 2023, that Natalie Cooper has been named president of the company’s Amerigroup Tennessee health plan. She has been with Elevance for nine years and previously served with the Department of Defense. Read More
Texas
Texas Names Emily Zalkovsky as State Medicaid Director. The Texas Health and Human Services Commission announced on June 1, 2023, that Emily Zalkovsky would be the next state Medicaid director, effective July 1. Zalkovsky, who is currently deputy Medicaid director, will replace Stephanie Stephens. Read More
Legislature Approves $900 Million to Increase Medicaid Reimbursement Rates for Nursing Homes. Skilled Nursing News reported on May 31, 2023, that the Texas House and Senate passed a bill allocating $900 million to increase Medicaid reimbursement rates for nursing homes. The bill now goes to Governor Greg Abbott for his signature. Read More
Utah
Utah Requests Section 1115 Medicaid Waiver Amendment to Extend Postpartum Medicaid Coverage. The Centers for Medicare & Medicaid Services announced on June 2, 2023, that Utah proposed an amendment to its Section 1115 Medicaid waiver to extend postpartum Medicaid coverage from 60 days to 12 months. The comment period is open until July 2. Read More
Washington
Washington to Request Medicaid Coverage for Former Foster Youth From Out of State. The Washington Health Care Authority announced on June 6, 2023, plans to submit to federal regulators an amendment to the state’s Section 1115 Medicaid Transformation Project waiver to provide Medicaid coverage for former foster youth from other states who turned 18 before January 1, 2023. The amendment, which will be submitted for approval to the Centers for Medicare & Medicaid Services, will also provide continuous enrollment for children enrolled in the Children’s Health Insurance Program up to age six. The public comment period ended on May 22, and the state is using the feedback to refine the application before submitting. Read More
Washington Receives Federal Approval to Provide Continuous Medicaid Coverage to Children Up to Age 6. The Washington Health Care Authority announced on June 6, 2023, federal approval of an amendment to the state’s Section 1115 Medicaid Transformation Project waiver, allowing continuous Medicaid coverage for children until the age of six. Read More
Wyoming
Wyoming Disenrolls 70 Medicaid Beneficiaries During April Redeterminations. The Wyoming Department of Health submitted on May 8, 2023, its April report to the Centers for Medicare & Medicaid Services on the Medicaid redeterminations process, which showed that 70 Medicaid beneficiaries were disenrolled and transferred to the Exchange. No one was disenrolled for procedural reasons.
National
April Medicaid Redeterminations Update: Arkansas, California, Colorado, Idaho, Indiana, Iowa, Kentucky, Nevada, North Carolina, Texas, and West Virginia. States have begun to release April redeterminations reports, including Arkansas, California, Colorado, Idaho, Indiana, Iowa, Kentucky, Nevada, North Carolina, Texas, and West Virginia.
• Arkansas disenrolled nearly 63,000 Medicaid beneficiaries during the April redeterminations period. The state also renewed coverage for more than 61,200 beneficiaries.
• California renewed coverage for nearly 1.1 million Medicaid beneficiaries during the April redeterminations period. The state did not disenroll anyone due to its continuous coverage requirements.
• Colorado renewed coverage for 127,475 Medicaid beneficiaries during the April redeterminations period. The state did not disenroll anyone.
• Idaho renewed coverage for 17,345 Medicaid beneficiaries during the April redeterminations period. The state found 10,798 beneficiaries ineligible and transferred them to the Exchange.
• Indiana disenrolled nearly 53,000 Medicaid beneficiaries during the April redeterminations period. The state renewed coverage for more than 65,000.
• Iowa disenrolled more than 11,000 Medicaid beneficiaries during the April redeterminations period. The state renewed coverage for 35,500.
• Kentucky initiated renewals for nearly 61,000 Medicaid beneficiaries during the April redeterminations period. The state has not begun disenrolling or renewing coverage yet.
• Nevada renewed coverage for almost 54,000 Medicaid beneficiaries during the April redeterminations period. The state has not begun disenrolling beneficiaries yet.
• North Carolina initiated renewals for nearly 134,300 Medicaid beneficiaries during the April redeterminations period. The state will begin renewing and disenrolling beneficiaries in July.
• Texas initiated renewals for more than 1 million Medicaid beneficiaries during the April redeterminations period. The state will begin renewing and disenrolling beneficiaries in August.
• West Virginia disenrolled almost 17,600 Medicaid beneficiaries during the April redeterminations period. The state renewed coverage for almost 30,000.
Merck Seeks Injunction to Block Medicare Drug Negotiation Program. Politico reported on June 6, 2023 that New Jersey-based pharmaceutical company Merck is seeking a federal injunction to block the Medicare drug price negotiation program. The lawsuit, which claims the program is unconstitutional, was filed in U.S. District Court in Washington, DC, against the U.S. Department of Health and Human Services and the Centers for Medicare & Medicaid Services. Read More
Hospitals Fear Loss of 340B Discounts for Patients Seen at Some Off-Site Clinics. Modern Healthcare reported on June 6, 2023, that hospital outpatient clinics may lose 340b drug discounts for patients prescribed medications before the clinics were registered with the Office of Pharmacy Affairs Information System and listed on a Medicare cost report. Last month, the Health Resources and Services Administration removed guidance from its website allowing the discounts. Read More
CMS Proposes Steps to Prevent Duplicate 340B Drug Discounts on Medicaid Plan Claims. JD Supra reported on June 6, 2023, that the Centers for Medicare & Medicaid Services (CMS) proposed steps to help prevent duplicate 340B drug discounts on Medicaid managed care organization claims. The proposed change to the Medicaid Drug Rebate Program would modify health plan contracts to require the use of unique, Medicaid-specific codes and group numbers on beneficiary insurance cards. Read More
Federal Appeals Court to Hear Arguments on Exchange Preventative Services Coverage Mandate. The Hill reported on June 5, 2023, that a federal appeals court will hear arguments on whether to continue to pause a Texas court ruling that Exchange plans do not have to cover preventive services. The U.S. Court of Appeals temporarily paused the decision in May until a panel could hear oral arguments. Read More
States Utilize Technology Solutions During Medicaid Redeterminations. Modern Healthcare reported on June 5, 2023, that many states are working with technology vendors during Medicaid redeterminations to improve the process. For example, Arizona has a web-based chat bot that answers 30 frequently asked questions, Arkansas and Nevada are using a mobile digital platform for Medicaid agencies from Gainwell technologies, and Delaware and New York are in the process of implementing the platform. Read More
CMS Establishes Managed Care Group. The Centers for Medicare & Medicaid Services (CMS) announced on June 2, 2023, that the Center for Medicaid and CHIP Services is establishing a Managed Care Group in an effort to better support managed care monitoring and oversight. The Division of Managed Care Policy and the Division of Managed Care Operations will be moved to the new group. Read More
U.S. Senate Passes Debt Ceiling Agreement. Politico reported on June 1, 2023, that the U.S. Senate passed the debt ceiling agreement. There were 11 amendment votes, none of which passed, including one from Senator Rand Paul (R-KY) to cut federal spending by five percent in each of the next two years, which would have impacted funding for Medicaid, Medicare, and the Exchange. The bill now goes to President Biden for his signature. Read More
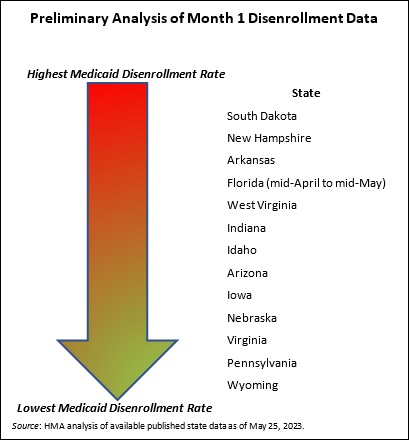
600,000 Medicaid Beneficiaries Are Disenrolled Since Redeterminations Began in April. KFF Health News reported on June 1, 2023, that about 600,000 Medicaid beneficiaries have been disenrolled nationwide since redeterminations began on April 1, mostly for procedural reasons. As of May, the median disenrollment rate by state is 24 percent, with Florida the highest at 54 percent and Virginia and Pennsylvania the lowest at 10 percent, according to a Kaiser Family Foundation report. Five states began disenrolling in April, and another 14 began in May. The rest of the states will begin in June, July, or October. Read More
8 States Seek Federal Approval for Postpartum Medicaid Extension in 2023. KFF Health News reported on June 1, 2023, that eight states have sought federal approval to extend postpartum Medicaid coverage from 60 days to 12 months in 2023. The Centers for Medicare & Medicaid Services had approved extended coverage for 33 states and Washington, DC, as of May 30. Lawmakers in Nebraska, Nevada, New Hampshire, and Wisconsin are currently considering a coverage extension, while Iowa, Idaho, and Arkansas failed to pass legislation. Read More
U.S. House Passes Debt Ceiling Agreement. The Washington Post reported on May 31, 2023 that the U.S. House passed a debt ceiling agreement. The bill now heads to the Senate. U.S. Senator Rand Paul (R-KY) plans to add an amendment that would cut federal spending by five percent in each of the next two years and could impact funding for Medicaid, Medicare, and the Exchange. Read More
Industry News
UnitedHealth/Optum Makes Unsolicited $3.26 Billion Bid for Amedisys. Health Payer Specialist reported on June 5, 2023, that UnitedHealth’s Optum subsidiary made an unsolicited, all-cash bid of $3.26 billion ($100 per share) to acquire Amedisys. Amedisys has already accepted an all-stock offer from Option Care Health valued at $97.38 per share. Read More
The Rise Fund Invests in Banyan Treatment Centers. TPG Capital’s Rise Fund announced on June 2, 2023, an investment in Banyan Treatment Centers, a provider of substance use disorder and mental health services. Terms of the investment were not disclosed. Read More
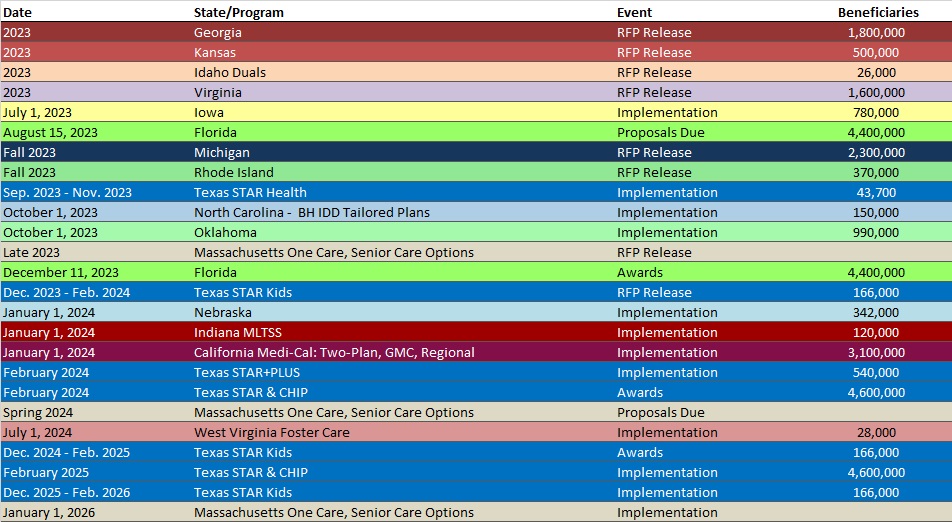
RFP Calendar
Company Announcements
Leaders from University Hospitals and MCG to Speak at Ohio Hospital Association Annual Meeting: MCG interoperability expert, Daniel Cawood, will co-present with University Hospitals’ Director of Clinical Documentation Integrity & Utilization Management, Kelly Skorepa, BSN, RN, CCDS, at the Ohio Hospital Association’s (OHA) 108th Annual Meeting & Education Summit happening June 12-14, 2023, at the Hilton Columbus at Easton in Columbus, Ohio. Ms. Skorepa and Mr. Cawood will present the session, “Fostering Payer-Provider Collaboration to Reduce Administrative Burden,” on Tuesday, June 13, from 9:45 a.m. to 10:45 a.m. ET. Read More
HMA News & Events
Upcoming HMA Conference:
Medicaid Directors to Discuss Challenges, Opportunities at HMA Conference in Chicago
Medicaid directors from California, Illinois, Mississippi, and Nevada will address key opportunities and challenges facing state Medicaid programs during HMA’s 2023 annual conference, October 30-31, at the Fairmont Chicago Millennium Park. The theme of this year’s event is Innovations in Publicly Sponsored Health Care: How Medicaid, Medicare, and Marketplaces Are Driving Value, Equity, and Growth.
Speakers will include Jacey Cooper, State Medicaid Director, Chief Deputy Director for Health Care Programs, California Department of Health Care Services; Kelly Cunningham, Medicaid Administrator, Division of Medical Programs, Illinois Department of Healthcare and Family Services; Drew Snyder, Executive Director, Mississippi Division of Medicaid; Stacie Weeks, Administrator/Medicaid Director, Nevada Department of Health and Human Services Division of Health Care Financing and Policy.
Early bird registration ends July 31. For additional information, visit the conference website at https://conference.healthmanagement.com/ or contact Carl Mercurio. Group rates, government discounts, and sponsorships are available.
Upcoming HMA Webinars:
Youth Mental Health Access: School-Based Intervention Strategies. The youth behavioral health crisis has resulted in a cascade of federal funding, advisories, and overall opportunities to improve resources to help kids. This webinar will present the Dialectical Behavioral Therapy (DBT) STEPS for Adolescents model, which is a low cost, high impact approach that empowers schools to intervene and support well-being and resiliency before students are in crisis, self-harming, or suicidal. Wednesday, June 14, 2023, 1 pm ET. Click here to register.
1115 Justice Waivers: Connecting Community Partners to Improve Transitions of Care. Part 3 of HMA’s webinar series, 1115 Medicaid Justice Demonstration Waivers: Bridging Healthcare, will focus on optimizing key partnerships before, during and after transition from a carceral setting into the community to ensure the best outcomes for individuals eligible for 1115 approved waiver services. Thursday, June 15, 2 pm ET. Click here to register.
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- District of Columbia SNP Membership at 14,255, Mar-23 Data
- Georgia SNP Membership at 270,782, Mar-23 Data
- Hawaii SNP Membership at 33,541, Mar-23 Data
- Massachusetts SNP Membership at 67,967, Mar-23 Data
- Minnesota Medicaid Managed Care Enrollment is Up 2.8%, Apr-23 Data
- Nevada SNP Membership at 30,489, Mar-23 Data
- New Mexico SNP Membership at 31,909, Mar-23 Data
- New Mexico Medicaid Managed Care Enrollment is Up 1.4%, Apr-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Georgia Families Care Management Organization Qualifications RFQC and Cancellation Notice, 2023
- New Hampshire Electronic Visit Verification RFP, Jun-23
- Texas STAR Health Foster Care RFP, Scoring, and Response, Oct-22
Medicaid Program Reports, Data, and Updates:
- Arizona PHE Medicaid Unwinding Monthly Report to CMS, Apr-23
- Arkansas PHE Medicaid Unwinding Monthly Report to CMS, Apr-23
- California PHE Medicaid Unwinding Monthly Report to CMS, Apr-23
- Colorado PHE Medicaid Unwinding Monthly Report to CMS, Apr-23
- Idaho PHE Medicaid Unwinding Monthly Report to CMS, Apr-23
- Indiana PHE Medicaid Unwinding Monthly Report to CMS, Apr-23
- Iowa PHE Medicaid Unwinding Monthly Report to CMS, Apr-23
- Kentucky PHE Medicaid Unwinding Monthly Report to CMS, Apr-23
- Michigan Medicaid Capitation Rate Certification Reports, CY 2019-23
- Michigan PHE Medicaid Unwinding Monthly Report to CMS, Apr-23
- Nevada PHE Medicaid Unwinding Monthly Report to CMS, May-23
- Nevada DHHS Drug Transparency Report, Jun-23
- North Carolina PHE Medicaid Unwinding Monthly Report to CMS, Apr-23
- Texas PHE Medicaid Unwinding Monthly Report to CMS, Apr-23
- Virginia PHE Medicaid Unwinding Monthly Report to CMS, Apr-23
- West Virginia PHE Medicaid Unwinding Monthly Report to CMS, Apr-23
- Wyoming PHE Medicaid Unwinding Monthly Report to CMS, Apr-23
