HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Highlights from Kaiser/HMA 50-State Medicaid Director Survey

- California Medi-Cal Members Can Now Fill Prescriptions at Costco

- Florida Healthcare Groups File Challenge to $15 Minimum Wage Budget Provision

- Hawaii Works With HMA to Develop Medicaid Social Determinants of Health Initiative

- Massachusetts Home Health Care Workforce Decreases by 13 Percent from 2019 to 2022

- Nebraska Says Protest of Medicaid Managed Care Contracts Will Not Delay Implementation

- New Hampshire Executive Council Approves Medicaid Dental Contract

- Pennsylvania Receives Federal Approval to Extend Postpartum Medicaid Coverage to 12 Months

- South Dakota Voters Approve Medicaid Expansion

- Virginia Projects ‘Tiny’ Increase in Fiscal 2024 State Medicaid Costs

- Medicaid FFS More Likely to Cover Opioid Use Disorder Treatment than Medicaid Managed Care

- Medicaid Plans Report Barriers to Telehealth Access

- 19 States Have Implemented Strategies to Increase Direct Care Worker Wages, Report Finds

- CNSI, Kepro to Merge; Apax Partners to Exit

- Walgreens’ VillageMD to Acquire Summit Health

- Clover Health to Reduce Medicare ACO REACH Population by Two-Thirds in 2023

In Focus
Highlights from Kaiser/HMA 50-State Medicaid Director Survey
This week, our In Focus section reviews highlights and shares key takeaways from the 22nd annual Medicaid Budget Survey conducted by The Kaiser Family Foundation (KFF) and Health Management Associates (HMA). Survey results were released on October 25, 2022, in two new reports: How the Pandemic Continues to Shape Medicaid Priorities: Results from an Annual Medicaid Budget Survey for State Fiscal Years 2022 and 2023 and Medicaid Enrollment & Spending Growth: FY 2022 & 2023. The report was prepared by Elizabeth Hinton, Madeline Guth, Jada Raphael, Sweta Haldar, and Robin Rudowitz from the Kaiser Family Foundation and by Kathleen Gifford, Aimee Lashbrook, and Matt Wimmer from HMA; and Mike Nardone. The survey was conducted in collaboration with the National Association of Medicaid Directors (NAMD).
This survey reports on policies in place or planned for FY 2022 and FY 2023, including state experiences with policies adopted in response to the COVID-19 pandemic. The conclusions are based on information provided by the nation’s state Medicaid Directors.
Key Report Highlights
In the following sections, we highlight a few of the major findings from the reports. This is a fraction of what is covered in the 50-state survey reports, which include significant detail and findings on policy changes and initiatives related to delivery systems, health equity, benefits, telehealth, provider rates and taxes, and pharmacy. The reports also look at the opportunities, challenges, and priorities facing Medicaid programs.
Medicaid Enrollment and Spending Growth
The COVID-19 pandemic created significant implications for Medicaid. During this time, Medicaid enrollment has reached record highs due to the Families First Coronavirus Response Act (FFCRA), enacted in March 2020, which authorized a 6.2 percentage point increase in the federal match rate, or Federal Medical Assistance Percentage (FMAP), retroactive to January 1, 2020, and until the Public Health Emergency (PHE) ends. The increase was available to states that meet certain “maintenance of eligibility” (MOE) requirements. Since the survey, the PHE was extended to mid-January 2023, somewhat delaying the anticipated effects described in survey.
Medicaid enrollment growth slowed to 8.4 percent in FY 2022, after a sharp increase in FY 2021 (11.2 percent). Almost all responding states reported that the MOE continuous enrollment requirement was the most significant factor driving FY 2022 enrollment growth. Responding states expect Medicaid enrollment growth to decline (-0.4 percent) in FY 2023, based largely on the assumption that the PHE and the related MOE requirements would end by mid-FY 2023. States anticipate larger declines as Medicaid redeterminations and renewals resume.
In FY 2022, total Medicaid spending is expected to reach a peak growth of 12.5 percent, with enrollment growth as the primary driver. For FY 2023, total spending growth is expected to slow to 4.2 percent, assuming slower enrollment growth after the unwinding of the PHE. State Medicaid spending grew by 9.9 percent in FY 2022 and is projected to increase by 16.3 percent in FY 2023 once enhanced federal fiscal relief expires. If the PHE is extended, state spending increases and enrollment decreases that states anticipated for FY 2023 could occur later.
Figure 1 – Percent Change in Medicaid Spending and Enrollment, FY 1998-23
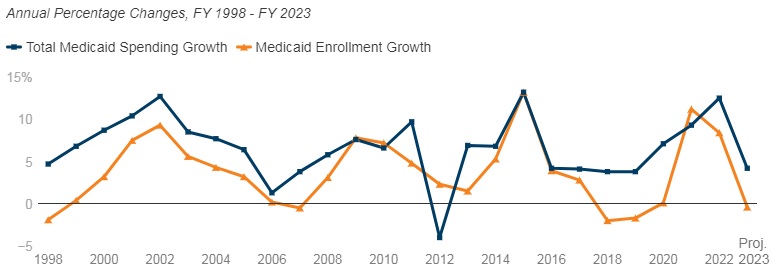
SOURCE: FY 2022-2023 spending data and FY 2023 enrollment data are derived from the KFF survey of Medicaid officials in 50 states and DC conducted by Health Management Associates, October 2022. 49 states submitted survey responses by Oct. 2022; state response rates varied across questions. Historic data reflects growth across all 50 states and DC and comes from various sources.
Delivery Systems
- Capitated managed care remains the predominant delivery system for Medicaid in most states. Forty-six states operated some form of Medicaid managed care (managed care organizations (MCOs) and/or primary care case management (PCCM)). Forty-one states contracted with risk-based MCOs. Of these, only Colorado and Nevada did not offer MCOs statewide. Only five states – Alaska, Connecticut, Maine, Vermont, and Wyoming – lacked a comprehensive Medicaid managed care model.
- Thirty-four states, including District of Columbia, operate MCOs only, five states operate PCCM programs only, and seven states operate both MCOs and a PCCM program.
- Twenty-seven states contracted with one or more PHPs to provide Medicaid benefits, including behavioral health care, dental care, vision care, non-emergency medical transportation (NEMT), and long-term services and supports (LTSS).
- Of the forty-one states that contracted with MCOs, 35 reported that 75 percent or more of their Medicaid beneficiaries were enrolled in MCOs as of July 1, 2022.
Figure 2 – MCO Managed Care Penetration Rates for Select Groups of Medicaid Beneficiaries as of July 1, 2022
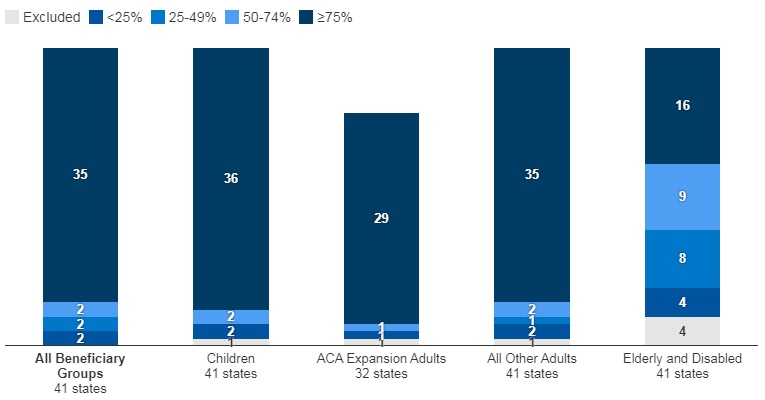
SOURCE: KFF survey of Medicaid officials in 50 states and DC conducted by HMA, October 2022.
Medicaid Managed Care and Delivery System Changes
- California, Missouri, Nevada, New Jersey, and New York reported expanding mandatory MCO enrollment for targeted populations.
- Missouri and Ohio reported introducing specialized managed care programs for children with complex needs.
- California, Nevada, and Tennessee indicated that they were carving in certain long-term services and supports (LTSS) into their managed care programs.
- California and Ohio reported carving out pharmacy services in FY 2022 or FY 2023, respectively. The District of Columbia carved out emergency medical transportation from its MCO contracts in FY 2022.
- Maine, North Carolina, Oregon, and Washington reported changes to their PCCM programs.
- Virginia plans to implement Cardinal Care in FY 2023, merging the state’s two existing managed care programs: Medallion 4.0 (serving children, pregnant individuals, and adults) and Commonwealth Coordinated Care Plus (CCC Plus) (serving seniors, children and adults with disabilities, and individuals who require LTSS).
- Forty-one states reported at least one specified delivery system and payment reform initiative (e.g. Patient-Centered Medical Home (PCMH), ACA Health Homes, Accountable Care Organization (ACO), Episode of Care Initiatives, All-Payer Claims Database (APCD)).
Health Equity
- Twenty-five states reported using at least one specified strategy to improve race, ethnicity, and language (REL) data completeness. Of the 45 responding states, 16 states reported requiring MCOs and other applicable contractors to collect REL data, 12 states reported that eligibility, renewal materials, and/or applications explain how REL data will be used and/or why reporting these data are important, nine states reported linking Medicaid enrollment data with public health department vital records data, and eight states reported partnering with one or more health information exchanges (HIEs) to obtain additional REL data for Medicaid enrollees.
- Twelve of 44 responding states reported at least one financial incentive tied to health equity in place in FY 2022. The vast majority of these incentives were in place in managed care arrangements (11 of 13). Within managed care arrangements, states most commonly reported linking or planning to link capitation withholds, pay for performance incentives, and/or state-directed provider payments to health equity-related quality measures. Only two states (Connecticut and Minnesota), reported a FFS financial incentive in FY 2022. Five additional states report plans to implement financial incentives linked to health equity in FY 2023.
- Sixteen of 37 responding MCO states reported at least one specified health equity MCO requirement in place in FY 2022. The number of MCO states with at least one specified health equity MCO requirement in place is expected to grow significantly in FY 2023, from 16 to 25 states. Examples of MCO requirements to address health equity include having a health equity plan, designating a Health Equity Officer, and staff training on health equity and/or implicit bias.
Figure 3 – MCO Requirements to Address Health Equity, FYs 2022-23
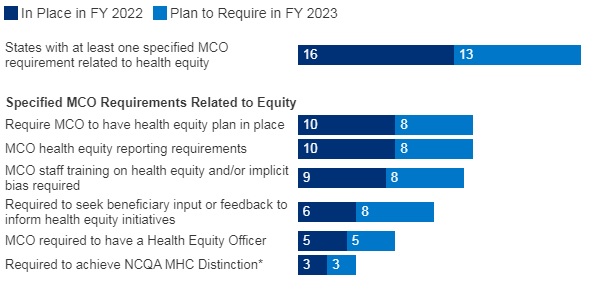
SOURCE: KFF survey of Medicaid officials conducted by HMA, October 2022; n=37 states.
Benefits
- Thirty-three states reported new or enhanced benefits in FY 2022 and 34 states are adding or enhancing benefits in FY 2023. Two states reported benefit cuts or limitations in FY 2022 and no states reported cuts or limitations in FY 2023.
Figure 4 – Select Categories of Benefit Enhancements or Additions, FYs 2022-23

SOURCE: KFF survey of Medicaid officials conducted by HMA, October 2022; Arkansas and Georgia did not respond.
- Behavioral Health Services. States reported service expansions across the behavioral health care continuum, including institutional, intensive, outpatient, home and community-based, and crisis services. States reported addressing SUD outcomes, including coverage of opioid treatment programs, peer supports, and enhanced care management. At least ten states are expanding coverage of crisis services, which aim to connect Medicaid enrollees experiencing behavioral health crises to appropriate community-based care, including mobile crisis response services and crisis stabilization centers.
- Pregnancy and Postpartum Services. In April 2022, a temporary option under ARPA to extend Medicaid postpartum coverage from 60 days to 12 months took effect. In addition to the states that took advantage of this eligibility change, some states are enhancing coverage of pregnancy and post-partum services. Nine states (California, District of Columbia, Illinois, Maryland, Michigan, New Mexico, Nevada, Rhode Island, and Virginia) are adding coverage of services provided by doulas and seven states (Alabama, Delaware, Illinois, Maryland, Ohio, Oregon, and Vermont) are investing in the implementation or expansion of home visiting programs.
- Preventive Services. Sixteen states reported expansions of preventive care in FY 2022 or FY 2023. For example, seven states are expanding services to prevent and/or manage diabetes, such as continuous glucose monitoring. Other reported preventive benefit enhancements relate to asthma services, vaccinations, and genetic testing and/or counseling.
- Services Targeting Social Determinants of Health. Many states reported new and expanded benefits targeting social determinants of health. Twelve states reported new or expanded housing-related supports, as well as other services and programs tailored for individuals experiencing homelessness or at risk of being homeless.
- Dental Services. Nine states are adding comprehensive adult dental coverage, while additional states report expanding specific dental services for adults.
Telehealth
- Most states have or plan to adopt permanent Medicaid FFS telehealth expansions that will remain in place even after the pandemic, though some are considering guardrails on such policies. Nearly all responding states that contract MCOs reported that changes to FFS telehealth policies would also apply to MCOs.
Figure 5 – Changes to FFS Medicaid Telehealth Policy, FY 2022 or FY 2023
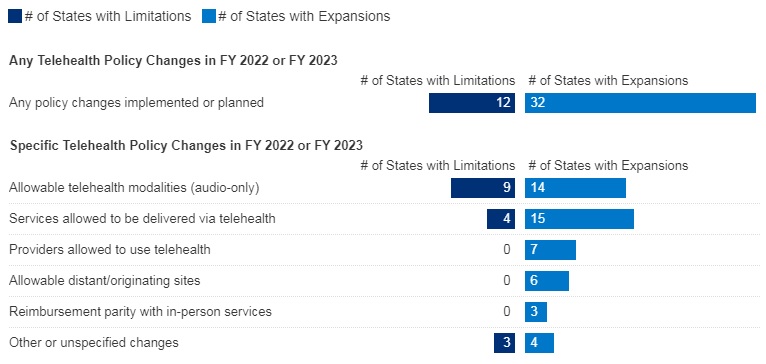
SOURCE: KFF survey of Medicaid officials conducted by HMA, October 2022; n=48 states.
- Nearly all responding states added or expanded audio-only telehealth coverage in Medicaid in response to the COVID-19 pandemic. Twenty-eight states reported that they newly added audio-only coverage while 19 states expanded existing coverage. Nearly all states reported audio-only coverage of mental health and substance use disorder (SUD) services. States least frequently reported audio-only coverage of home and community-based services (HCBS) and dental services. Two states (Mississippi and Wyoming) reported no coverage of audio-only telehealth for the services in question.
- Telehealth utilization by Medicaid enrollees has been high during the pandemic but has decreased and/or leveled off more recently. States noted that telehealth utilization trends over time correspond to COVID-19 outbreaks, with higher utilization during COVID-19 surges and lower utilization when case counts are lower. In general, states reported that telehealth utilization was projected to continue at higher levels than before the pandemic, at least for some service categories.
- Thirty-seven states (out of 47 responding) reported that behavioral health services were among those with the highest utilization. Additionally, a majority of states reported high utilization of evaluation and management (E/M) services and/or other physician/qualified health care professional office/outpatient services, including primary care.
- States reported ACA expansion adults as one of the groups most likely to use telehealth (about one-third of responding states), followed by children and individuals with disabilities (each identified by about one-sixth of responding states).
- Concerns regarding services delivered via telehealth included the quality of diagnoses, whether audio-only telehealth may be less effective, and inadequate access.
- Key issues that may influence future Medicaid telehealth policy decisions include analysis of data, state legislation and federal guidance, and cost concerns.
Provider Rates and Taxes
- In FY 2022, all 49 responding states reported implementing rate increases for at least one category of provider and 19 states reported implementing rate restrictions. In FY 2023, 48 states reported at least one planned rate increase and the number of states planning to restrict rates increased to 25 states.
- States reported rate increases for nursing facilities and home and community-based services (HCBS) providers more often than other provider categories. The survey also found an increased focus on dental rates with about half of reporting states (20 in FY 2022 and 25 in FY 2023) reporting implementing or plans to implement a dental rate increase.
Figure 6 – FFS Provider Rate Changes Implemented in FY 2022 and Adopted for FY 2023
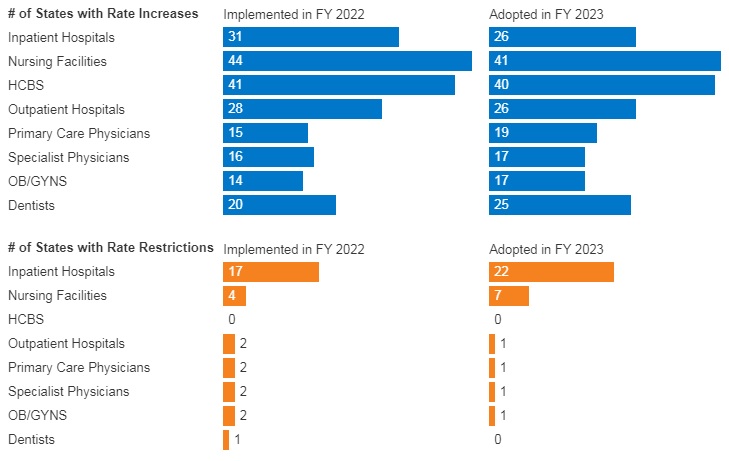
SOURCE: KFF survey of Medicaid officials in 50 states and DC conducted by HMA, October 2022.
- States continue to rely on provider taxes and fees to fund a portion of the non-federal share of Medicaid costs. All states but Alaska have at least one provider tax or fee in place. Thirty-eight states had three or more provider taxes in place in FY 2022 and eight other states had two provider taxes in place.
- The most common Medicaid provider taxes in place in FY 2022 were taxes on nursing facilities (46 states), followed by taxes on hospitals (44 states), intermediate care facilities for individuals with intellectual disabilities (33 states), and MCOs (18 states).
- Three states (Alabama, Mississippi, and Wyoming) reported plans to add new ambulance taxes in FY 2023.
Pharmacy
- Most states that contract with MCOs report that the pharmacy benefit is carved into managed care (34 out of 41 states that contract with MCOs). Six states (California, Missouri, North Dakota, Tennessee, Wisconsin, and West Virginia) report that pharmacy benefits are carved out of MCO contracts as of July 1, 2022. California was the latest to carve out pharmacy benefits as of January 1, 2022. Two states (New York and Ohio) report plans to carve out pharmacy from MCO contracts in state FY 2023 or later.
- In FY 2022, Kentucky began contracting with a single PBM for the managed care population. Louisiana and Mississippi report that they will require MCOs to contract with a single PBM designated by the state in FY 2023 and FY 2024, respectively.
- Seven states (Alabama, Arizona, Colorado, Massachusetts, Michigan, Oklahoma, and Washington) have value-based arrangements (VBAs) in place with one or more drug manufacturers.
- More than half of responding states reported newly implementing or expanding at least one initiative to contain prescription drug costs in FY 2022 or FY 2023.
- Six states (Florida, Kentucky, Massachusetts, Maryland, Nebraska, Nevada) reported recently implemented or planned policies to prohibit spread pricing or require pass through pricing in MCO contracts with PBMs.
Key Opportunities, Challenges, and Priorities in FY 2023 and Beyond
When asked to identify the top challenges for FY 2023 and beyond, Medicaid directors listed the following:
- The unwinding of PHE emergency measures and the resumption of redeterminations.
- Expiration of emergency authorities.
- Lasting focus on COVID-19, including vaccinations, long-COVID, decreased utilization of preventive care services, and future emergency preparedness.
Medicaid directors stated that future priorities shaped by COVID-19 include:
- Health equity.
- Specific populations and service categories, including behavioral health, long-term services and supports, and maternal and child health.
- Health care workforce challenges.
- Payment and delivery system initiatives and operations.
- IT system modernization.
- Social determinants of health.
Medicaid directors note that COVID-19 has presented both new opportunities and challenges and has also shifted and shaped ongoing Medicaid priorities.
Links to Kaiser/HMA 50-State Survey Reports
HMA Roundup
Arkansas
Arkansas Offers Grants to CBOs that Help With PHE Unwinding. The Arkansas Department of Human Services (DHS) announced on November 7, 2022, the availability of grants for community-based organizations (CBOs) that assist with Medicaid member outreach ahead of the public health emergency (PHE) unwinding. CBOs, which will be required to complete an application, may be eligible for one-time stipends of $500 or $5,000 based on participation level. Read More
California
California Medi-Cal Members Can Now Fill Prescriptions at Costco. The California Department of Health Care Services announced on November 3, 2022, that Medi-Cal members can now fill prescriptions at 122 Costco pharmacies without a Costco membership. The state projects that more than 50,000 Medi-Cal prescriptions will be filled per month at Costco. Read More
Florida
Florida Healthcare Groups File Challenge to $15 Minimum Wage Budget Provision. WMNF/The News Service of Florida reported on November 4, 2022, that the Florida Assisted Living Association, the Florida Ambulance Association, and the Home Care Association of Florida filed challenges to a state budget provision that would require Medicaid providers to increase the minimum wage for direct care providers to $15 per hour. The challenges say the state did not undergo proper rule making processes to define direct care workers. The groups also filed a lawsuit in September 2022 to prevent a provision that would allow employees to sue providers that do not meet the $15 minimum wage requirement. Read More
Hawaii
Hawaii Medicaid Fraud Unit Had Low Conviction Rate in 2020. Hawaii News Now reported on November 4, 2022, that the Hawaii Medicaid Fraud Control Unit charged only two people and convicted one with fraud out of 600 cases in 2020. Other states with similar caseloads charged significantly more, including Pennsylvania, with 115 charges out of 569 cases, and Mississippi, with 104 charges out of 600 cases. According to Deputy Attorney General Landon Murata, who heads the unit, COVID-19, lack of cooperation from federal law enforcement agencies, and new processes and regulations contributed to the low conviction rate. Read More
Hawaii Works With HMA to Develop Medicaid Social Determinants of Health Initiative. State of Reform reported on November 2, 2022, that Hawaii is working with Health Management Associates (HMA) to develop a Medicaid social determinants of health initiative. The project, initiated by the state’s Department of Human Services’ Med-QUEST Division, would aim to identify, evaluate, and reduce health disparities based on factors including age, race, ethnicity, gender, primary language, and disability status. Read More
Massachusetts
Massachusetts Home Health Care Workforce Decreases by 13 Percent from 2019 to 2022. WBUR reported on November 2, 2022, that employment in home health care services in Massachusetts decreased by 13 percent from 2019 to 2022, according to figures presented at the Massachusetts Health Policy Commission’s annual cost trends hearing. Employment at nursing care and skilled nursing facilities decreased by 24 percent. A recent report from the Massachusetts Health and Hospital Association also estimated that hospitals are short by about 19,000 full-time workers. Read More
Maryland
Maryland Behavioral Health ASO Made $223.5 Million in Improper Payments, Audit Finds. Health Payer Specialist reported on October 31, 2022, that Maryland’s contracted behavioral health administrative services organization (ASO) made $223.5 million in improper payments to providers, according to a report from the state Department of Legislative Services. The report blamed lax oversight by the state of the ASO vendor, which is UnitedHealth Group’s Optum. Read More
Minnesota
Minnesota-Based UCare Faces Lawsuit Over Plan to Expand Board. The Star Tribune reported on November 7, 2022, that the University of Minnesota (UM) filed a state lawsuit opposing an effort to increase the number of seats on the UCare health plan board of directors. UM says it would lose its board majority and be left out of key decisions concerning the not-for-profit health plan, which it created decades ago. Read More
Nebraska
Nebraska Says Protest of Medicaid Managed Care Contracts Will Not Delay Implementation. The Omaha World-Herald reported on November 6, 2022, that incumbent Elevance/Healthy Blue’s protest of the Nebraska Medicaid managed care awards is not expected to delay the January 1, 2024, planned implementation. Contracts were awarded to incumbents UnitedHealthcare and Centene/Nebraska Total Care, as well as new entrant Molina. Healthy Blue initially ranked third out of five bidders but was moved to fourth place after an oral interview component was added to the procurement process. Read More
New Hampshire
New Hampshire Executive Council Approves Medicaid Dental Contract. InDepthNH reported on November 2, 2022, that the New Hampshire Executive Council approved a contract with Delta Dental to provide dental coverage to 88,000 adult Medicaid enrollees. The state is also increasing payments to incentivize dental providers to take on the new patients. Read More
Pennsylvania
Pennsylvania Receives Federal Approval to Extend Postpartum Medicaid Coverage From 60 Days to 12 Months. Pennsylvania Department of Human Services Acting Secretary Meg Snead announced on November 3, 2022, federal approval to extend postpartum Medicaid coverage from 60 days to 12 months. Medicaid covers three in 10 births in Pennsylvania. Read More
South Dakota
South Dakota Voters Approve Medicaid Expansion. Politico reported on November 9, 2022, that South Dakota voters passed a constitutional amendment to implement Medicaid expansion. The measure, which passed with 56 percent support, would cover about 40,000 adults. Read More
Texas
Texas Recovers $490 Million in Health, Human Services Programs Fraud, Waste in Fiscal 2022. The Texas Office of the Inspector General (OIG) reported on October 6, 2022, that it recovered more than $490 million in fiscal 2022 related to fraud, waste and abuse in the expenditure of funds in the state’s health and human services programs. The OIG Quarterly Report also found nearly $877 million in potential future recoveries and another $166 million in cost avoidance. Read More
Virginia
Virginia Projects ‘Tiny’ Increase in Fiscal 2024 State Medicaid Costs. The Richmond Times-Dispatch reported on November 3, 2022, that Virginia is projecting a “tiny” increase of $12.3 million in state Medicaid funds in fiscal 2024. Program finances have been buoyed by enhanced federal funds during the pandemic and a hospital assessment. Overall costs for the Virginia Medicaid program are projected to increase 3.1 percent in fiscal 2024 and 2.9 percent in fiscal 2025. Read More
National
Medicaid FFS Is More Likely to Cover Opioid Use Disorder Treatment than Medicaid Managed Care, Study Finds. Health Payer Intelligence reported on November 8, 2022, that Medicaid fee-for-service (FFS) programs are more likely to cover treatments for opioid use disorder (OUD) than Medicaid managed care plans; however, FFS programs also impose more prior authorization requirements, according to a study published in JAMA Health Forum. Medicaid covers approximately 40 percent of Americans with OUD. The study looked at Medicaid managed care and FFS programs from 2018 in 38 states and the District of Columbia, which covered about 70 million beneficiaries. Read More
Supreme Court Hears Arguments in Case Concerning Medicaid Enrollee Rights. Fierce Healthcare reported on November 8, 2022, that the U.S. Supreme Court heard arguments in a lawsuit that could decide whether Medicaid beneficiaries can sue the federal government to enforce their rights. The case involves a lawsuit against a nursing home in Marion County, IN, over whether it violated the rights of a now-deceased nursing home patient. The court’s decision is expected in June. Read More
CMMI Eyes Population-Based Models Aimed at Increasing Primary, Specialty Care Coordination. Fierce Healthcare reported on November 7, 2022, that the Center for Medicare and Medicaid Innovation (CMMI) is eyeing population-based payment models aimed at increasing care coordination between primary care physicians and specialists, according to its updated strategic vision for value-based care. Other initiatives include accountable care organization (ACO) models that increase primary care access for Medicaid members, specialty-focused models, and improved ways to measure ACO results. Read More
Majority of States Have Implemented SUPPORT Act Provisions, CMS Report Finds. The Centers for Medicare & Medicaid Services (CMS) announced on November 7, 2022, that the majority of state managed care entities have implemented, or have plans to implement, the provisions of the Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act (SUPPORT Act), according to CMS’s 2020 annual drug review report to Congress. The provisions include claims review process and safety edits for opioid fills, processes to identify potential fraud or abuse of controlled substances, and automated processes to monitor concurrent prescriptions of opioids and benzodiazepines. Read More
Medicaid Plans Report Barriers to Telehealth Access. Health Payer Specialist reported on November 7, 2022, that Medicaid managed care plans reported barriers to telehealth access, according to a survey from the Institute for Medicaid Innovation. Plans said that barriers include a lack of broadband access among members and provider information technology issues that disrupt telehealth sessions. The study surveyed both state and national Medicaid managed care plans, including for-profit and not-for-profit. Read More
Uninsured Rate Is Lower In States With State-based Exchanges, Study Finds. Health Payer Specialist reported on November 7, 2022, that the 17 states that operate their own Exchange have an average uninsured rate of 10 percent, which is lower than the 15 percent rate for states that use Healthcare.gov, according to a study from the Commonwealth Fund. The study found that state-based Exchanges spend more on outreach and advertising. Read More
Supreme Court to Decide if Individuals Can Sue Medicaid Over Rights Violations. NPR reported on November 6, 2022, that the U.S. Supreme Court will hear oral arguments in a case that will decide whether individuals on programs that receive federal funding, including Medicaid, can sue states over rights violations. The initial case was filed in 2019 against a nursing facility and its owner Health and Hospital Corporation of Marion County, IN, for allegedly violating a man’s rights while he was being treated for dementia. Read More
19 States Have Implemented Strategies to Increase Direct Care Worker Wages, Report Finds. McKnight’s Long-Term Care News reported on November 4, 2022, that at least 19 states have implemented strategies to increase direct care worker wages through Medicaid provider rate increases and minimum wage policies, according to a report from the National Governors Association Center for Best Practices. The report also found that benefits such as health insurance, paid time off, childcare, and transportation can be important recruiting and retention tools. Read More
Medicaid Plans Adjust Data Collection Tools That Are Found to Be Biased, Survey Finds. Modern Healthcare reported on November 4, 2022, that 88 percent of Medicaid health plans changed or stopped using algorithms, policies, or models that were found to be biased against people of color in the past year, according to a survey by the Institute for Medicaid Innovation. A majority of survey respondents collect data on languages spoken, sex, race, and ethnicity to help identify and address health disparities. Read More
Most Metro Areas Have Highly Concentrated Medicare Advantage Markets, AMA Study Finds. Health Payer Intelligence reported on November 4, 2022, that about 80 percent of metropolitan statistical areas (MSAs) had highly concentrated Medicare Advantage (MA) markets, according to a study from the American Medical Association (AMA). The study also found that over a third of MA markets had one insurer with a share of 50 percent or more. The study looked at health insurance markets in 380 MSAs as of January 1, 2021. Read More
Industry News
CNSI, Kepro to Merge; Apax Partners to Exit. Carlyle-backed health information technology company CNSI announced on November 9, 2022, an agreement to merge with Kepro, which offers care management, quality oversight, and clinical assessment services. Kepro is a portfolio company of Apax Partners, which will not be an investor in the combined entity following the transaction. CNSI chief executive Todd Stottlemyer will lead the combined company, while Kepro chief executive Susan Weaver, MD, will become president. Read More
Acadia Healthcare Acquires Four Opioid Comprehensive Treatment Centers in Georgia. Acadia Healthcare announced on November 8, 2022, its acquisition of four opioid comprehensive treatment centers (CTCs) in the Atlanta suburbs from Brand New Start Treatment Centers. Acadia Healthcare now operates 148 medication-assisted treatment facilities in Georgia. Read More
InnovaCare Health Acquires Pak Medical Group. InnovaCare Health announced on November 8, 2022, the acquisition of Pak Medical Group, a physician-led medical group in Texas. Pak has 29 clinicians in seven locations. Read More
Oscar Health to Exit Medicare Advantage Markets in New York, Texas; Exchanges in Arkansas, Colorado. Modern Healthcare reported on November 8, 2022, that Oscar Health will no longer offer Medicare Advantage (MA) plans in New York and Texas in 2023. The company’s sole MA plan for 2023 is being jointly marketed with hospital systems in Broward County, FL. Oscar will also exit the Arkansas and Colorado Exchanges in 2023. Read More
Clover Health to Reduce Medicare ACO REACH Population by Two-Thirds in 2023. Modern Healthcare reported on November 7, 2022, that Medicare plan Clover Health expects a two-thirds reduction in the number of patients it manages through the Medicare ACO Realizing Equity, Access, and Community Health (REACH) program in 2023; instead, seeking to participate in the Medicare Shared-Savings Program. The ACO REACH model is the name of the newly redesigned Global and Professional Direct Contracting model. Clover had expected to generate more than half of company revenues from direct contracting in 2022. Read More
Ensign Group Agrees to Acquire 20 SNFs from Sabra Health Care. The Ensign Group announced on November 7, 2022, an agreement to acquire 20 skilled nursing facilities (SNFs) in California from Sabra Health Care REIT. The transaction is expected to close in February 2023. Read More
Friday Health Plans to Exit TX, NM Marketplaces for 2023. Becker’s Payer Issues reported on November 7, 2022, that Friday Health Plans will not offer Exchange plans in Texas and New Mexico in 2023. Friday indicated that it hopes to reenter the Texas market in 2024. Read More
Walgreens’ VillageMD to Acquire Summit Health. Walgreens Boots Alliance’s VillageMD announced on November 7, 2022, a definitive agreement to acquire Summit Health-CityMD, a primary, specialty, and urgent care provider. Walgreens will invest $3.5 billion in debt and equity to support the acquisition and will remain the largest shareholder in VillageMD, with a 53 percent stake. Cigna Corp. also invested in the deal and will become a minority owner in VillageMD. Read More
WindRose Health Investors Completes Acquisition of Bank’s Apothecary. WindRose Health Investors announced on November 3, 2022, that it has completed its acquisition of Bank’s Apothecary, which provides medication distribution and adherence services to patients suffering from severe and persistent mental illness, substance use disorders, and intellectual and developmental disabilities. The combined company will serve more than 22,000 patients across 23 states through seven closed-door pharmacies. Read More
Companions and Homemakers Sells Medicaid, Private Pay Divisions. AccordCare announced on November 2, 2022, its acquisition of the Medicaid division of Companions and Homemakers, an in-home personal care provider in Connecticut. TheKey has acquired the private pay division of Companions and Homemakers. Read More
CVS Health Considers Sale of Omnicare After $2.5 Billion in Losses. Becker’s Hospital Review reported on November 2, 2022, that CVS Health is considering the sale of Omnicare, a long-term care pharmacy services provider, after the organization lost $2.5 billion in the third quarter of fiscal 2022. CVS also announced in October 2022 plans to sell benefits technology company Bswift to Francisco Partners. Read More
Acadia Healthcare Adds 600 Comprehensive Treatment Center Beds in 2022. Behavioral Health Business reported on November 1, 2022, that Acadia Healthcare added 600 comprehensive treatment center (CTC) beds in 2022 through mergers, acquisitions, joint ventures, and internal growth. Arcadia is also on track to open six new CTCs in 2022. Acadia has 239 behavioral health facilities with 10,600 beds in 39 states. Read More
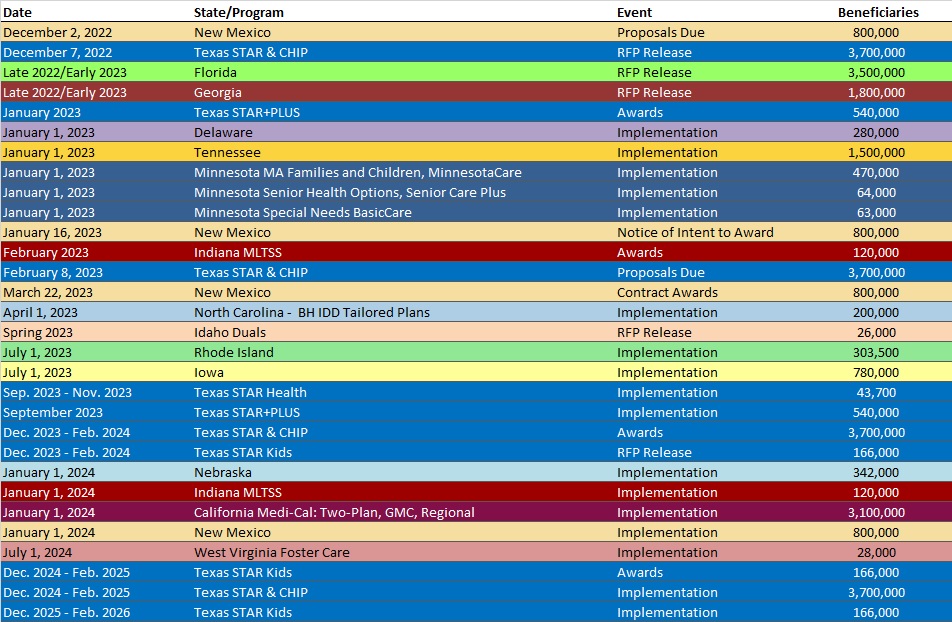
RFP Calendar
HMA News & Events
WAKELY, AN HMA COMPANY, WHITE PAPER
