This week's roundup:
- In Focus: CMS Releases Medicaid LTSS Expenditures Report for FY 2020
- Arizona Releases Fee-For-Service Pharmacy Benefits Management Services RFP
- Arkansas Releases Medicaid Enterprise Systems Independent Verification, Validation Services RFP
- Arkansas Releases Medicaid Dental Services RFP
- California Enacts Bills to Improve Treatment of Individuals with Mental, Behavioral Health Disorders
- Colorado Individual Plan Rates to Rise 9.7 Percent in 2024
- Florida Announces List of Bidders for Statewide Medicaid Managed Care ITN
- Florida Releases ITNs for 6 Behavioral Health Managing Entity Regions
- Georgia Pathways to Coverage Medicaid Expansion Enrollment is 1,343 Through September
- Medicaid Eligibility Redeterminations News: Iowa, Kentucky, Louisiana, Maryland, Michigan, Pennsylvania, South Dakota
- Maryland Cannot Document Receipt of Federal Funds, Shows $1.1 Billion Deficit in Medicaid Clearing Account, Audit Shows
- New Jersey Enacts Medicaid Rate Increase for Reproductive Health Care Providers
- New Mexico Releases Closed Loop Referral Service RFQ
- Pennsylvania Expands List of Medicaid Providers Eligible to Provide Street Medicine Services
- Previous Direct Contracting ACO Model Saved Medicare $371.5 Million in 2022
- UPMC, Washington Health System Sign Merger Agreement
In Focus
CMS Releases Medicaid LTSS Expenditures Report for FY 2020
This week, our In Focus section summarizes the Medicaid Long-Term Services and Supports (LTSS) Annual Expenditures Report, which the Centers for Medicare & Medicaid Services (CMS) released on October 17, 2023. The report includes detailed information about Medicaid LTSS expenditures for federal fiscal year (FY) 2020, which runs from October 1, 2019, through September 30, 2020. During this time, LTSS spending grew 20 percent to $199.4 billion from the previous year.
Medicaid LTSS Expenditures
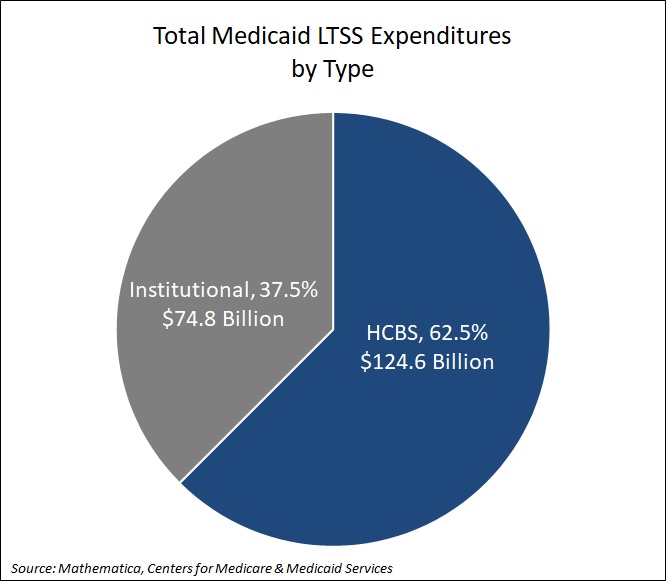
Medicaid LTSS expenditures cover home and community-based services (HCBS), which includes personal care and home health, as well as institutional care, which includes services provided in nursing facilities, intermediate care facilities (ICF) for individuals with intellectual or developmental disabilities (IDD), and mental health facilities. HCBS accounted for 62.5 percent ($124.6 billion) of LTSS expenditures. The remaining 37.5 percent, or $74.8 billion, was directed toward institutional care (see Figure 1).
Figure 1. Medicaid LTSS Expenditures by Type
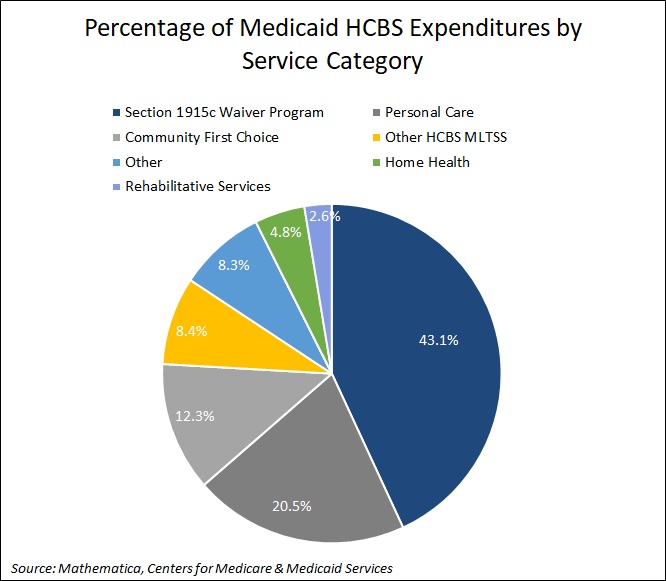
In addition, Section 1915c waiver program spending accounted for 43.1 percent of HCBS expenditures, followed by personal care at 20.5 percent. See Figure 2 for additional breakouts.
Figure 2. Percentage of Medicaid HCBS Expenditures by Service Category
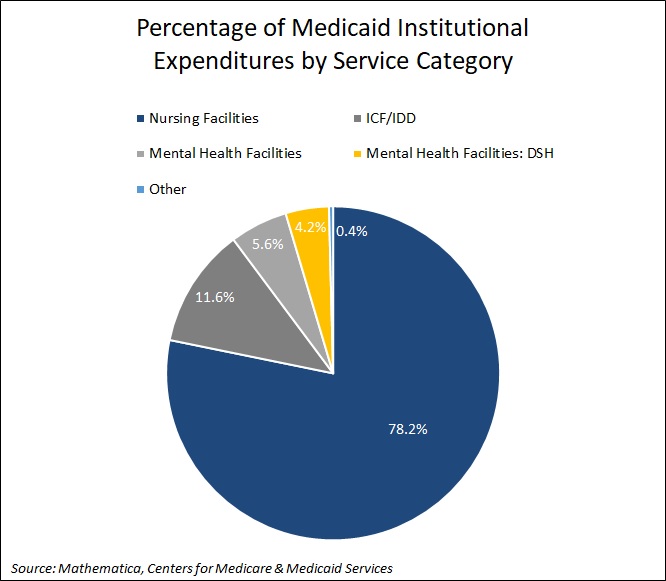
Nursing facilities accounted for the largest percentage (78.2 percent) of institutional care spending. See Figure 3 for additional breakouts.
Figure 3. Percentage of Medicaid Institutional Expenditures by Service Category
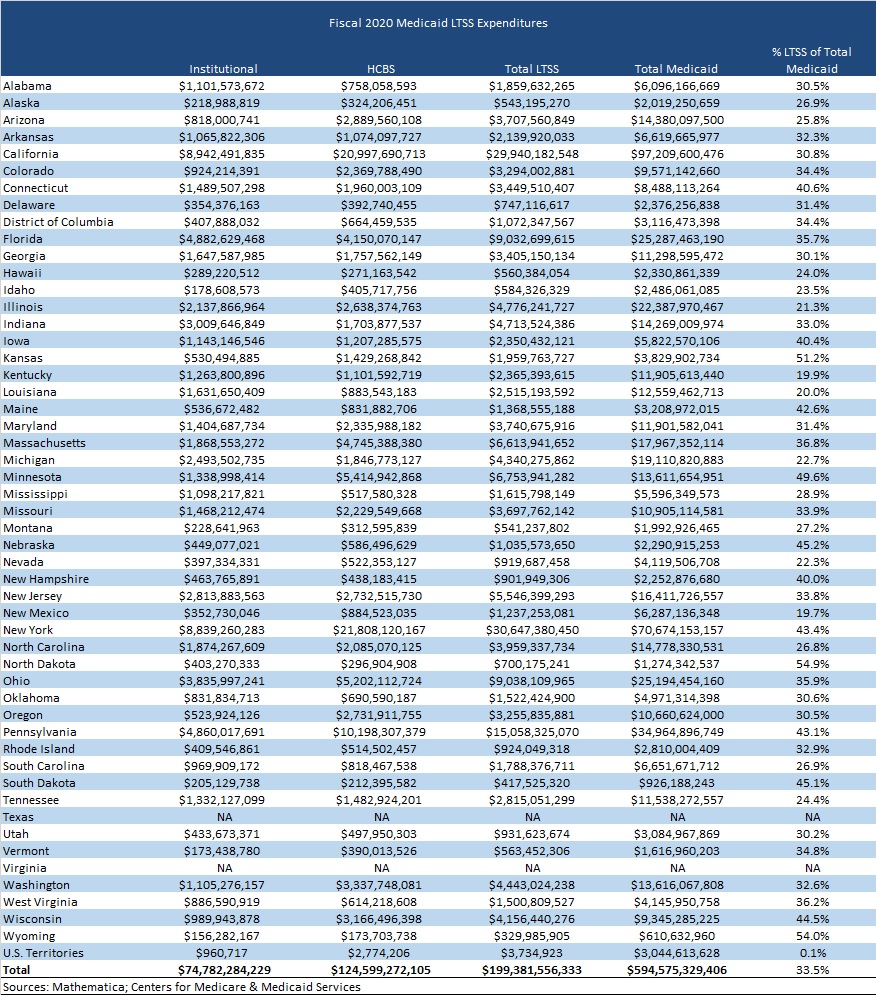
Medicaid LTSS spending accounted for 33.5 percent of total Medicaid spending in FY 2020. States with the highest LTSS as a percentage of total Medicaid spending were North Dakota at 54.9 percent, Wyoming at 54 percent, Kansas at 51.2 percent, Minnesota at 49.6 percent, and Nebraska at 45.2 percent. Texas and Virginia did not report spending for Medicaid LTSS programs, which comprise a substantial share of total LTSS expenditures in those two states (see Table 1).
Table 1. Medicaid LTSS Expenditures by State
LTSS spending per resident also varied from state to state. On average, states spent $679 Medicaid LTSS dollars per state resident in FY 2020. Utah had the lowest Medicaid LTSS expenditures per state resident at $284, whereas the District of Columbia had the highest at $1,554 per resident.
Medicaid MLTSS Expenditures
Medicaid managed long-term services and supports (MLTSS) spending totaled $57 billion in FY 2020. HCBS accounted for $35.7 billion and institutional care accounted for $21.3 billion. As more states adopted and extended their Medicaid managed care programs, MLTSS spending grew 750 percent from FY 2008.
In FY 2020, 25 states had operational MLTSS programs. Of these, nine were Financial Alignment Initiative (FAI) capitated model demonstrations for dual eligible members. New York, Pennsylvania, Florida, and California accounted for 58 percent of total MLTSS spending nationally, with New York representing 23 percent of total national MLTSS expenditures. Three states—Idaho, Texas, and Virginia—did not report MLTSS spending (see Figure 4).
Figure 4. States with MLTSS programs, FY 2020
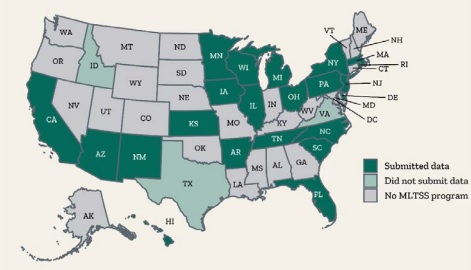
Iowa had the highest share of MLTSS expenditures as a percentage of total Medicaid LTSS expenses in FY 2020 at 95 percent. Arizona and Kansas followed at 94 percent and Hawaii at 74 percent. The national average was 29 percent. At the lowest end were South Carolina at 4 percent and Rhode Island at 12 percent, both of which are fee-for-service states. Michigan followed at 14 percent.
Contributing Factors to LTSS Expenditures
The COVID-19 public health emergency, which includes the first six months of the pandemic that started in March 2020, had a major effect on LTSS expenditures in FY 2020. Many residents in long term care facilities are covered by Medicaid and disproportionately experienced the most COVID-19 deaths. States began to implement various policies to address the impact of COVID-19 among Medicaid LTSS users. This includes modifying utilization limits for covered services and increasing payment rates for certain institutional services and HCBS.
As mentioned earlier, Texas and Virginia did not report Medicaid LTSS expenditures, which undercut the national total. Other factors that affect the reliability of Medicaid LTSS data include changes in state MLTSS expenditure reporting methods, and changes in state Medicaid LTSS policies and programs.
Note: CMS hired Mathematica to conduct the research, which used CMS-64 Medicaid expenditure report data, state-reported MLTSS data, Money Follows the Person (MFP) worksheets for proposed budgets, CMS 372 data on section 1915(c) waiver program population groups, and U.S. Census data to compile the report.
HMA Roundup
Alabama
Alabama Owes Federal Government Nearly $15 Million Over Failure to Invoice Medicaid Drug Rebates, OIG Finds. The Black Chronicle reported on October 19, 2023, that Alabama owes the federal government nearly $15 million because the state did not invoice rebates from manufacturers for prescription drugs covered by Medicaid between 2016 and 2019, according to a report conducted by the U.S. Office of Inspector General (OIG). OIG recommends that Alabama pay back the funds, examine potential funds owed for years following 2019, and strengthen its system to ensure the invoice of rebates. The state has indicated that it will comply with recommendations but will need additional time to refund the owed rebates. Read More
Arizona
Arizona Releases Fee-For-Service Pharmacy Benefits Management Services RFP. The Arizona Health Care Cost Containment System released on October 24, 2023, a pharmacy benefit manager request for proposals (RFP) for the state’s fee-for-service Medicaid populations. The current incumbent is United/OptumRX. AHCCCS will award one, three-year contract with two one-year renewal options. Notices of intent to bid are due November 24, and proposals are due by December 7. The anticipated start date is October 1, 2024. Read More
Arkansas
Arkansas Releases Medicaid Enterprise Systems Independent Verification, Validation Services RFP. The Arkansas Department of Human Services released on October 18, 2023, a request for proposals (RFP) to procure a new vendor for Independent Verification and Validation services for the new Arkansas Medicaid Enterprise System (MES). Arkansas will award one contract, to run for three years, with four one-year contract extensions. Proposals are due November 22, 2023, with awards expected on January 26, 2024. The anticipated contract start date is July 1, 2024. The first system to be implemented under the new Arkansas MES will be the Arkansas Medicaid Pharmacy Program in June 2024, with awards to be announced on January 5, 2024. Read More
Arkansas Releases Medicaid Dental Services RFP. The Arkansas Department of Human Services (DHS) released on September 20, 2023, a request for proposals (RFP) to procure a new vendor to provide Medicaid dental managed care services. Arkansas will award at least two to three one-year contracts, with six one-year contract extensions. Current incumbents are Delta Dental of Arkansas and Managed Care of North America (MCNA). Proposals are due November 9, 2023, with awards expected on December 8, 2023. The anticipated implementation date is set for April 1, 2024. Read More
California
California Medicaid Program Spending Is Projected to Hit $152 Billion in Fiscal 2024. The California Legislative Analyst’s Office reported on October 23, 2023, that spending on Medi-Cal, the state’s Medicaid program, is projected to be $152 billion in fiscal 2024, a 12 percent increase from fiscal 2023. The figure includes $90.5 billion in federal funds, $37.5 billion in state general funds, and $23.8 billion from other sources. Spending includes $6 million to begin implementing the proposed BH-CONNECT Medi-Cal demonstration waiver and $250 million to support the CalAIM Behavioral Health Payment Reform initiative. Read More
California Submits BH-CONNECT Waiver Amendment to Support Individuals with Serious Behavioral Needs. Governor Gavin Newsom announced on October 20, 2023, that California has submitted for federal approval a Medicaid Section 1115 waiver amendment to implement the state’s Behavioral Health Community-Based Organized Networks of Equitable Care and Treatment (BH-CONNECT) demonstration aimed at better supporting individuals with serious behavioral health needs. The demonstration contains approaches specifically designed for high-need children and youth. The amendment to the state’s California Advancing and Innovating Medi-Cal (CalAIM) waiver would also offer temporary rent assistance for individuals who are homeless or at risk and increase flexibility for counties to use federal funds for behavioral health beds. Read More
California Enacts Bills to Improve Treatment of Individuals with Mental, Behavioral Health Disorders. California Governor Newsom signed on October 12, 2023, two bills aimed at improving treatment of individuals with mental health and substance use disorder. Senate Bill 326 will reform the Mental Health Services Act for the first time in two decades. The second bill, Assembly Bill 531, authorizes a $6.38 billion bond for 11,150 new behavioral health treatment beds, housing resources, and 26,700 outpatient treatment settings. Read More
Colorado
Colorado Individual Plan Rates to Rise 9.7 Percent in 2024. The Colorado Sun reported on October 24, 2023, that Colorado individual health plan rates are expected to rise 9.7 percent in 2024, which is slightly lower than the 10 percent increase originally requested by insurers. Colorado is one of a few states with a public option, Colorado Option, which requires health plans to offer public option plans wherever they offer individual or small-employer plans. Read More
Florida
Florida Announces List of Bidders for Statewide Medicaid Managed Care ITN. The Florida Agency for Health Care Administration announced on October 25, 2023, the list of bidders for its Statewide Medicaid Managed Care invitation to negotiate (ITN). The bidders are AmeriHealth Caritas, CVS/Aetna, Florida Community Care, Humana, ImagineCare, Molina, Sentara Care Alliance, Simply Healthcare Plans, South Florida Community Care Network/Community Care Plan, Centene/Sunshine State Health Plan, and UnitedHealthcare. Healthcare providers will have the opportunity to comment on respondents from October 27 to November 9. Awards are anticipated to be announced February 23, 2024.
Florida Releases ITNs for 6 Behavioral Health Managing Entity Regions. The Florida Department of Children and Families released on September 25, 2023, invitations to negotiate (ITNs) to rebid behavioral health managing entity contracts across six regions: Northeast, Central, Northwest, Southern, Suncoast, and Southeast. Proposal due dates range from January 9 through January 18, 2024. Awards are anticipated for March 6, 2024. Contracts will begin July 1, 2024, and last for five years. The incumbents are Big Bend Community Based Care, Broward Behavioral Health Coalition, Central Florida Behavioral Health Network, Central Florida Cares Health System, Lutheran Services Florida, South Florida Behavioral Network, and Southeast Florida Behavioral Health Network.
Florida Legislative Committee Kicks Off With Briefings from Medicaid Agency, Healthy Kids. Health News Florida reported on October 19, 2023, that the first meeting of Florida’s new Select Committee on Health Innovation included briefings from the state Agency for Health Care Administration and Florida Healthy Kids. The committee was formed in September to focus on healthcare access and affordability during the 2024 legislative session, which begins in January. Read More
Georgia
Georgia Pathways to Coverage Medicaid Expansion Enrollment is 1,343 Through September. The Associated Press reported on October 20, 2023, that enrollment in the Georgia Pathways to Coverage Medicaid expansion program was 1,343 through September. The program, which launched in July, is expected to eventually attract about 100,000 members, according to the Georgia Department of Community Health. The program includes work requirements and limits coverage to adults earning up to 100 percent of poverty. Read More
Hawaii
Hawaii Submits Five-year Medicaid Section 1115 Waiver Extension Application. State of Reform reported on October 23, 2023, that the Hawaii Department of Human Services has applied for a five-year extension of its Medicaid Section 1115 waiver. The extension seeks to add housing related services such as rental assistance, Medicaid coverage to incarcerated individuals 90 days prior to release, nutritional supports, Native Hawaiian traditional healing practices, a contingency management pilot, and initiatives to address health-related social needs. The public comment period will remain open through November 16. Read More
Illinois
Illinois Puts Temporary Enrollment Pause on Health Benefits for Immigrant Seniors Program. The Illinois Department of Healthcare and Family Services (HFS) announced on October 19, 2023, that new enrollments will be temporarily paused for the state’s Health Benefits for Immigrant Seniors (HBIS) program beginning November 6, as enrollment nears the cap of 16,500 individuals. HBIS provides Medicaid-like health care coverage to non-citizen individuals aged 65 and older. HFS will not be removing any current enrollees who remain eligible for HBIS coverage. Read More
Indiana
Indiana Receives Federal Approval of HCBS Waiver Rate Increases. WBIW reported on October 23, 2023, that the Centers for Medicare & Medicaid Services has approved the Indiana Division of Aging’s proposed home and community-based services (HCBS) waiver rate increases. The new rates are retroactive to July 1. Read More
Iowa
Iowa Disenrolls 5,649 Medicaid Beneficiaries During September Redeterminations. The Iowa Department of Health and Human Services reported on October 6, 2023, the disenrollment of 5,649 Medicaid beneficiaries during September redeterminations, including 952 for procedural reasons. The state renewed coverage for 38,341 beneficiaries.
Kentucky
Kentucky Health Plans Join Hospital Initiative to Streamline Medicaid Managed Care Provider Credentialing. Louisville Public Media announced on October 23, 2023, that three of Kentucky’s six Medicaid managed care organizations (MCOs) are participating in a program spearheaded by the Kentucky Hospital Association (KHA) to streamline provider credentialing. Providers in the Kentucky Health Alliance program will need to fill out one application for review by all three participating MCOs. KHA is working to enlist the state’s other three Medicaid plans as well, according to president Nancy Galvagni. Read More
Kentucky Disenrolls 16,468 Medicaid Beneficiaries During September Redeterminations. The Kentucky Department for Public Health (DPH) disenrolled 16,468 Medicaid beneficiaries during September redeterminations, including 882 for procedural reasons. The state renewed coverage for 80,417 beneficiaries.
Louisiana
Louisiana Medicaid Plans Face Criticism on Behavioral Health During Legislative Panel Hearing. The Louisiana Illuminator reported on October 18, 2023, that Louisiana Medicaid managed care plans faced criticism concerning behavioral health prior authorization practices during a hearing of the state’s House Subcommittee on Mental Health. Criticism centered on care denials, long wait times, low rates of follow-up visits, and a decrease in the share of funds spent on behavioral health. Read More
Louisiana Disenrolls 54,553 Medicaid Beneficiaries During August Redeterminations. The Louisiana Department of Health disenrolled 54,553 Medicaid beneficiaries during August redeterminations, including 40,508 for procedural reasons. The state has disenrolled a total of more than 160,000 Medicaid members since redeterminations began in April.
Maryland
Maryland Cannot Document Receipt of Federal Funds, Shows $1.1 Billion Deficit in Medicaid Clearing Account, Audit Shows. The Baltimore Sun reported on October 24, 2023, that the Maryland Department of Health (MDH) is unable to document receipt of $1.4 billion in fiscal 2022 federal funds, according to a state audit. The audit found a $1.1 billion deficit in the state Medicaid clearing account as of June 30, 2022, indicating the state allocated more funds than it received. The audit also shows MDH has failed to comply with state procurement laws and regulations. The state legislature will hold a hearing on the findings in November, and MDH indicated that it has hired an outside accounting firm to improve management of federal funds. Read More
Maryland Disenrolls 12,870 Medicaid Beneficiaries Following September Redeterminations. Maryland Matters reported on October 23, 2023, that the Maryland Department of Health disenrolled 12,870 Medicaid beneficiaries following September redeterminations. The figure does not include procedural disenrollments, which have been paused until November pending changes to ex parte renewal systems. Read More
Michigan
Michigan Governor Codifies Affordable Care Act Provisions into State Law. The Associated Press reported on October 20, 2023, that Michigan Governor Gretchen Whitmer signed legislation to codify Affordable Care Act (ACA) provisions into state law, requiring insurers to cover no-cost essential services, preventing care denials for preexisting conditions or sexual orientation, prohibiting coverage caps, and allowing parents to keep dependent children on their policies until age 26. Read More
Michigan Disenrolls 14,267 Medicaid Beneficiaries During September Redeterminations. The Michigan Department of Health and Human Services (MDHHS) announced on October 19, 2023, that the state disenrolled 14,267 Medicaid beneficiaries during September redeterminations, including 2,775 for procedural reasons. The state renewed coverage for 150,577 beneficiaries. Read More
Montana
Montana Health Officials Report on Progress of Effort to Move Certain Mental Health Patients to Community Settings. KTVH reported on October 24, 2023, that officials from the Montana Department of Public Health and Human Services (PHHS) updated a special committee on its progress in implementing a law to transfer individuals with certain mental health diagnoses from the state hospital to community-based settings. The diagnoses include Alzheimer’s, dementia, and traumatic brain injury. The Transition Review Committee, which is tasked with monitoring PHHS’s progress in implementing the law, is comprised of lawmakers, providers, patient advocates, and others. Read More
Nebraska
Nebraska Submits Request to Extend Substance Use Disorder Section 1115 Waiver. The Centers for Medicare & Medicaid Services (CMS) announced on October 20, 2023, that Nebraska submitted a request to extend the current Nebraska Substance Use Disorder (SUD) Medicaid Section 1115 demonstration, which authorizes the use of federal Medicaid matching dollars for reimbursement of services delivered to individuals with SUD that are residing in Institutions for Mental Diseases, for an additional five years with no changes. The waiver is currently set to expire June 30, 2024. The public comment period is open through November 19, 2023. Read More
New Jersey
New Jersey Enacts Medicaid Rate Increase for Reproductive Health Care Providers. New Jersey Governor Phil Murphy signed on October 24, 2023, a bill increasing Medicaid rates for reproductive health care providers, effective on October 1. The law also allocates $5 million to help create the New Jersey Reproductive Training and Education Initiative. Read More
New Mexico
New Mexico Releases Closed Loop Referral Service RFQ. The New Mexico Human Services Department issued on October 18, 2023, a request for quotes (RFQ) for a state-wide Closed Loop Referral Service for fiscal 2024. The RFQ is seeking one vendor to help coordinate care and referrals among healthcare and social service providers serving beneficiaries in several programs, including Medicaid, Temporary Assistance for Needy Families, Supplemental Nutrition Assistance Program, Child Support Program, and several behavioral health services. Applications will be accepted through November 10, and the award is expected to be announced December 1. The contract start date will be January 1, 2024. Read More
New York
New York Enacts Legislation Allowing Medicaid Reimbursement for Violence Prevention. New York Governor Kathy Hochul enacted on October 18, 2023, legislation allowing Medicaid reimbursement for community violence prevention programs. The legislation will also require violence specialists to complete at least six months training in prevention or youth development services; complete a violence prevention certification program through the New York State Department of Health; and complete four hours of continuing education annually. Read More
North Carolina
North Carolina Grants Health and Human Services Department Increased Regulatory Oversight of Behavioral Health Management Companies. NC Health News reported on October 18, 2023, that North Carolina legislators have granted the state Department of Health and Human Services greater oversight of the state’s six behavioral health management companies, known as Local Management Entities-Managed Care Organizations (LME-MCOs). Legislators indicated several potential areas of improvement, including altering the size and number of LME-MCOs, hastening the rollout of delayed tailored plans for individuals with severe mental health conditions or intellectual and developmental disabilities, and working to develop a Medicaid plan to improve services for children in the foster care system. Read More
Ohio
Ohio Medicaid Estate Recovery Sometimes Charges More than Services Used. The Dayton Daily News reported on October 25, 2023, that Ohio sometimes charges the estates of deceased Medicaid recipients a value greater than the cost of services received. The state relies on capitated costs in charging estates, rather than the cost actual services utilized, which is contrary to Medicaid and CHIP Payment and Access Commission (MACPAC) recommendations. Read More
Pennsylvania
Pennsylvania Hospital to Receive $86 Million From 340B Drug Pricing Program Settlement. Becker’s Hospital Review reported on October 24, 2023, that the Hospital of the University of Pennsylvania will receive $86 million from a legal settlement related to the federal 340B Drug Pricing Program, according to an article published in the Philadelphia Inquirer. The settlement addresses prior reductions in payments. Read More
Pennsylvania Struggles to Determine Number of Medicaid Beneficiaries Incorrectly Disenrolled. Spotlight PA reported on October 23, 2023, that Pennsylvania is struggling to determine which Medicaid beneficiaries were incorrectly disenrolled during the Medicaid eligibility redeterminations. The state, which faces technical difficulties and staffing shortages, owes federal officials a tally by the end of November. Read More
Pennsylvania Expands List of Medicaid Providers Eligible to Provide Street Medicine Services. The Pennsylvania Department of Human Services announced on October 23, 2023, that it has expanded the list of Medicaid providers eligible to provide “street medicine,” or care outside of a clinical setting for individuals who are homeless. The expansion includes dentists, federally qualified health centers, rural health clinics, various mental health services providers, substance use disorder service providers, and podiatrists. The expansion went into effect this month. Read More
Pennsylvania Raises Medicaid Rates for Ambulance Services, Reauthorizes Hospital Assessment. The Altoona Mirror reported on October 19, 2023, that Pennsylvania Governor Josh Shapiro will sign legislation that will raise Medicaid reimbursements for ambulance services by approximately $126 million a year, including increasing rates at least to Medicare levels. The bill also reauthorizes the hospital assessment program, which is expected to generate $1.4 billion in federal Medicaid matching dollars this year. Read More
South Dakota
South Dakota Interim Committee to Present 12 Proposals Aimed at Improving Long-term Care. Dakota News Now reported on October 19, 2023, that a South Dakota interim committee studying long-term care (LTC) services has drafted 12 proposals intended to improve LTC in the state, which include reimbursement for palliative care and in-home services, a $5 million technology grant to promote in-home care, a feasibility study for the Program of All-Inclusive Care for the Elderly, funding for patient monitoring, increased allowances for beneficiaries, and efforts to strengthen the provider workforce. Proposals will be presented before the legislative Executive Board in November. Read More
South Dakota Enrolls 7,500 Medicaid Beneficiaries in Medicaid Expansion Program. Dakota News Now reported on October 18, 2023, that South Dakota has enrolled nearly 7,500 individuals in its Medicaid expansion program, which began in July. Approximately 52,000 residents are eligible. Read More
Virginia
Virginia to Launch State-based Health Insurance Exchange on November 1. ABC 8 News/WRIC reported on October 20, 2023, that Virginia will launch its state-based health insurance Exchange on November 1, replacing the federal Healthcare.gov Exchange. Open enrollment is from November 1 through January 15. Read More
Wisconsin
Wisconsin Legislature Considers Bill Requiring Long-term Care Facilities to Provide Residents 90-day Eviction Notice. Wisconsin Public Radio reported on October 19, 2023, that the Wisconsin legislature is considering a bill to require nursing homes and assisted living facilities to give residents a 90-day written notice of eviction or relocation, or if they stop participating in the state’s Medicaid program. Wisconsin’s long-term care services are primarily served through the state’s Medicaid program. The bill still needs a committee hearing in the Assembly. Read More
National
Previous Direct Contracting ACO Model Saved Medicare $371.5 Million in 2022. Modern Healthcare reported on October 23, 2023, that the Global and Professional Direct Contracting Model, predecessor to the new Accountable Care Organization Reimagined to Achieve Equity and Community Health model (ACO REACH), saved Medicare approximately $371.5 million in 2022, up five-fold from 2021, according to the Centers for Medicare & Medicaid Services (CMS). CMS attributed the improvement to increases in the number of ACOs, experience, and more time on care management. Read More
Medicare Advantage Plans Cut Costs to Compensate for Lower Rates. Modern Healthcare reported on October 25, 2023, that Medicare Advantage insurers are making workforce reductions and trimming benefits for 2024 in response to a base rate reduction, a new risk-adjustment model, and a higher bar for quality bonuses. Benefit reductions include scaling back over-the-counter product allowances and increasing cost-sharing. Read More
2.3 Million More Uninsured Would Gain Coverage If Final 10 States Fully Implemented Medicaid Expansion, Report Finds. The Robert Wood Johnson Foundation reported on October 23, 2023, that 2.3 million additional people would gain healthcare coverage in 2024 if the remaining 10 states fully implemented Medicaid expansion, according to an analysis from the Urban Institute. Texas accounts for the most uninsured with 802,000 individuals, followed by Florida with 514,000 individuals. The uninsured rate would drop 25 percent for the whole population; 43.2 percent for non-Hispanic Black adults; 32.4 percent for young adults ages 19 to 24; 31 percent for women of reproductive age; and 51.3 percent for non-Hispanic Black women of reproductive age. Findings also suggest that expansion spending is outweighed by long-term savings and additional federal funding. The 10 states are Alabama, Florida, Georgia, Kansas, Mississippi, South Carolina, Tennessee, Texas, Wisconsin, and Wyoming. Read More
Medicare Shared Savings Program Is Non-factor in Federal Healthcare Spending Showing, CBO Reports. Healthcare Innovation reported on October 20, 2023, that the Medicare Shared Savings Program and other alternative payment models have not contributed to the unexpected deceleration in federal healthcare spending, according to written testimony by the Congressional Budget Office (CBO). CBO attributed the Medicare spending deceleration to slower-than-expected prescription drug cost growth and Medicaid spending to lower-than-expected long-term services and supports spending. Read More
CMS Approves Use of Medicaid Funds for Healthcare Delivered to Homeless on Streets. KFF Health News reported on October 19, 2023, that the Centers for Medicare & Medicaid Services (CMS) has begun permitting health insurers, including Medicaid and Medicare plans, to reimburse providers for “street medicine,” which is health care delivered to individuals who are homeless in any location or environment. The change, which was effective October 1, is the first time federal regulators have recognized the streets as a legitimate place to provide health care. Read More
Telehealth Increased Treatment Retention for Medicaid Patients with Opioid Use Disorder, Study Finds. mHealth Intelligence reported on October 19, 2023, that Medicaid patients who utilized telehealth for opioid use disorder treatment had higher treatment retention rates than those who did not utilize telehealth, according to a recent study published in JAMA Network Open. The study, which examines claims and enrollment data for adults in Kentucky and Ohio from November 1, 2019, to December 31, 2020, found that initiating buprenorphine treatment through telehealth was associated with better odds of 90-day retention in treatment in both states. Odds of retention lowered when adjusted for Black individuals compared to white counterparts or men versus women. The study was supported by the National Institute on Drug Abuse and conducted in partnership with the Substance Abuse and Mental Health Services Administration. Read More
Senate Finance Committee Hearing Addresses Deceptive Medicare Advantage Broker Practices. Modern Healthcare reported on October 18, 2023, that the Senate Finance Committee held a hearing to address deceptive Medicare Advantage brokerage practices aimed at boosting broker compensation through false information, harassment, and switching individuals out of plans without consent. The hearing mostly focused on brokers who steer individuals to Medicare plans with the biggest market share. The committee is urging federal regulators to better align broker compensation with the interests of beneficiaries and take action against brokers who harass people and who have repeated complaints lodged against them. Read More
Industry News
UPMC, Washington Health System Sign Merger Agreement. Modern Healthcare reported on October 24, 2023, that the University of Pittsburgh Medical Center (UPMC) and Washington Health System (WHS) have signed a definitive merger agreement. According to the agreement, WHS would be renamed UPMC Washington, and a third of its board would join the two-hospital system’s board. The deal still requires regulatory approval. Read More
MITRE Wins Contract to Operate CMS Alliance to Modernize Healthcare. MITRE announced on October 24, 2023, that it won a five-year contract to operate the Centers for Medicare & Medicaid Services (CMS) Alliance to Modernize Healthcare, a research and development center known as the Health FFRDC. Read More
Autism Therapy Provider BlueSprig Pediatrics Acquires Trumpet Behavioral Health. Behavioral Health Business reported on October 19, 2023, that autism therapy provider BlueSprig Pediatrics has acquired Colorado-based Trumpet Behavioral Health from WindRose Health Investors. Trumpet has 37 locations in seven states, including its Therapeutic Pathways and the Behavior Center brands. BlueSprig is backed by KKR. Terms of the deal were not disclosed. Read More
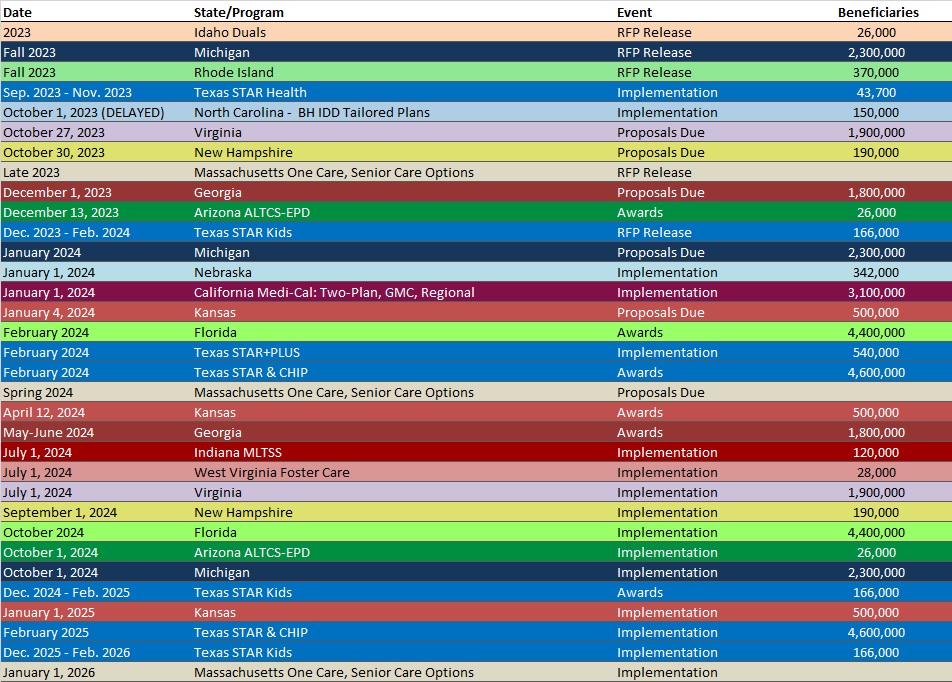
RFP Calendar
HMA News & Events
Upcoming HMA Webinar:
Opportunities for State Regulators to Shape Policy and Regulation of Treatment for Substance Use Disorder. Thursday, November 2, 2023, 12 p.m. ET. Rescheduled from June 20, 2023. Health Management Associates (HMA) is offering a 3-part series of webinars looking at the effect of proposed regulations on delivery of opioid treatment services to the population facing addiction issues. In this third and final webinar, HMA consultants will highlight opportunities for state regulators to shape policy and regulation of SUD treatment. New federal regulations encourage significant changes to how opioid treatment is provided, with the goal of expanding access and improving patient-centered care. State regulators will need to adapt their regulatory practices and work closely with Medicaid agencies and treatment providers so the new regulations can achieve their intended goals. This webinar will discuss how State Opioid Treatment Authorities (SOTAs), licensing entities, and state Medicaid agencies will need to work together to craft updated regulations, facility licensing, and reimbursement practices that advance person-centered care. Click here to register.
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Florida Medicaid Managed Care Enrollment is Down 2.5%, May-23 Data
- Florida Medicaid Managed Care Enrollment is Up 2.4%, Apr-23 Data
- Louisiana Medicaid Managed Care Enrollment is Down 6.8%, Sep-23 Data
- Michigan Medicaid Managed Care Enrollment is Down 0.7%, Aug-23 Data
- Michigan Dual Demo Enrollment is Down 7%, Aug-23 Data
- North Dakota Medicaid Expansion Enrollment is Down 12.2%, Sep-23 Data
- Tennessee Medicaid Managed Care Enrollment is Down 0.5%, Sep-23 Data
- Washington Medicaid Managed Care Enrollment is Down 3.2%, Jun-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Arizona Pharmacy Benefits Management (PBM) Services RFP, Oct-23
- Arkansas Medicaid Enterprise Systems (MES) Independent Verification, Validation (IVV) Services RFP, Oct-23
- Arkansas Dental Medicaid Managed Care RFP, Sep-23
- Colorado Medicare Advantage D-SNP Contracts, FY 2024
- Florida Behavioral Health Services Managing Entity ITNs, Sep-23
- New Mexico Closed Loop Referral Service RFQ, Oct-23
Medicaid Program Reports, Data, and Updates:
- Arkansas PHE Medicaid Redeterminations Monthly Reports to CMS, Sep-23
- Iowa PHE Medicaid Redeterminations Monthly Report to CMS, Sep-23
- Kentucky PHE Medicaid Redeterminations Monthly Report to CMS, Sep-23
- Louisiana Medicaid Managed Care Quality Strategy Evaluation Reports, FY 2020-23
- Louisiana PHE Medicaid Redeterminations Monthly Report to CMS, Aug-23
- Maine PHE Medicaid Redeterminations Monthly Report to CMS, Aug-23
- Maryland PHE Medicaid Unwinding Report, Sep-23
- Michigan PHE Medicaid Redeterminations Monthly Reports to CMS, Sep-23
- New York Comptroller’s Monthly Report on State Funds, Sep-23
- Rhode Island 2021 EQR Annual Technical Reports, Apr-23
- Rhode Island Medicaid Expenditure Reports SFY 2020-21
- Vermont Medicaid Program Enrollment and Expenditures Reports, SFY 2018-23
- Vermont Medicaid PMPM Reports, SFY 2019-22
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio at [email protected].