This week's roundup:
- In Focus: Rural Health Transformation Program Represents a One-Time Opportunity to Reshape Rural Care
- In Focus: MAHA Children's Health Strategy Report: Driving a New Era for Child Health Policy
- HMA Conference: Important Insights, Facilitated Introductions, Real Impact
- Georgia Rural Hospital to Close Labor, Delivery Unit Due to Medicaid Cuts
- Idaho Seeks $60 Million Supplemental Medicaid Funding Amid Rising Costs
- Illinois Releases HealthChoice Medicaid Managed Care RFP
- Louisiana Issues PACE RFI
- North Carolina to Expand Mobile Crisis Clinics
- House Stopgap Bill Extends Health Programs, Omits ACA Subsidies
- Lawmakers Submit Letter Urging HHS to Scrap 340B Pilot Rebate Plan
In Focus
Rural Health Transformation Program Represents a One-Time Opportunity to Reshape Rural Care
The Centers for Medicare & Medicaid Services (CMS) has officially opened the application window for the Rural Health Transformation Program (RHTP)—a $50 billion federal initiative designed to stabilize and transform rural health systems across the country. This one-time opportunity allows states to submit a comprehensive plan that could redefine how rural communities access care, manage chronic conditions, and sustain their healthcare infrastructure.
As outlined in our earlier In Focus article, States Begin to Engage with the Rural Health Transformation Program, RHTP represents one of the most significant federal investments in rural health in decades.
Applications must be signed by governors and submitted by November 5, 2025, and awards are expected by December 31, 2025, providing states with a very narrow window to act.
The remainder of this article explains key aspects of the RHTP application, including the evaluation and scoring aspects. Notably, the structure of the scoring system will reward states that are already aligned with these federal priorities, as well as those willing to implement new initiatives or make state policy changes to achieve alignment.
Program Overview and Funding Structure
Created under HR.1, the 2025 Budget Reconciliation Act, the RHTP allocates $10 billion annually from federal fiscal year (FY) 2026 to FY 2030, totaling $50 billion over five years. Funding is split into two tranches:
- Tranche 1 (Baseline funding): $25 billion distributed evenly across all states with approved applications.
- Tranche 2 (Workload funding): $25 billion distributed based on CMS scoring criteria, which include:
- The percentage of the state population in rural census tracts
- The proportion of rural health facilities in the state
- The financial and operational status of hospitals
- Other factors explained in the RHTP application notice
States must submit a single, one-time application that covers the full five-year period. Stand-alone provider applications will be declined. Hence, states must coordinate across agencies, providers, and stakeholders to develop a unified transformation strategy.
Importantly, this award is not a grant; rather, it is a cooperative funding agreement, which means CMS will play an active role in oversight and collaboration. States must be prepared to meet higher standards of accountability, transparency, and performance monitoring. According to the RHTP application, continued funding requires states to demonstrate satisfactory progress toward implementing their plan.
Application Requirements and Strategic Priorities
To be eligible for funding, states must submit a Rural Transformation Plan that addresses eight core priorities as follows:
Within these core priorities, state plans must propose activities that address several specific issues.
Technical Factor Weighting for Workload Funding Reflects Federal Policy Priorities
CMS outlines the eligibility criteria for baseline funding and the scoring components for workload funding. Baseline funds will be distributed equally among states, while workload funding will be based on each state’s rural facility and population score as well as their technical score. Evaluators will score technical factors based on state policy actions and initiative-based plans for each state.
The technical factors, and the weighting of these factors, in the RHTP application are not just neutral scoring mechanisms; rather, they are closely linked to the Trump Administration’s health policy priorities.
- Weighting Structure: The RHTP funding is split evenly between baseline funding (50%) and workload funding (50%). Although baseline funding ensures all states receive support, the workload funding is directly tied to technical scores that reflect how well a state’s plan aligns with federal objectives and demonstrates readiness to implement transformative change that furthers federal objectives.
- Scoring Criteria: Technical factors, such as rural population share, facility density, hospital financial status, scope of proposed activities, administrative capacity, stakeholder engagement, evaluation framework, and especially alignment with federal priorities, all contribute to the overall score. States that have already adopted or are willing to adopt federal policy priorities are positioned to score higher and receive more funding.
- Annual Recalculation: CMS will recalculate each state’s technical score and workload funding annually to incentivize ongoing alignment with federal priorities and measurable progress toward transformation goals.
- Alignment with Federal Priorities: One of the explicit scoring factors is “Alignment with Federal Priorities,” which measures the degree to which a state’s plan supports CMS goals for rural health transformation and sustainability. Under the Trump Administration, these priorities may include promoting value-based payment models, encouraging technology adoption, advancing adoption of Supplemental Nutrition Assistance Program (SNAP) food restriction waivers that prohibit the purchase of non-nutritious items, availability of integrated care plans for the Medicare-Medicare dually eligible population, reporting of full Medicaid T-MSIS data, and align policies with federal guidance on short-term limited duration insurance plans.
Preparing for What Happens Next: Implications for States, Providers, and Health Plans
The RHTP offers a rare opportunity to reshape rural healthcare. But success will require strategic coordination and a commitment to long-term change. States in the short and long term should consider include:
- Identifying stakeholders who will be involved: Hospitals, rural health clinics, federally qualified health centers (FQHCs), behavioral health providers, and community organizations must be part of the planning process.
- Reexamining priorities: States will need to reconcile competing needs across regions and provider types, balancing infrastructure investments with service delivery redesign.
- Understanding infrastructure needs to support their project: Technology, workforce, and models of care must be strengthened to support long-term transformation.
- Designing evaluation frameworks: States must include robust performance monitoring and reporting mechanisms to meet CMS expectations and secure future funding.
Providers and other stakeholders should also prepare to align with state strategies. Examples include:
- Participating in regional partnerships
- Adopting new care models and payment arrangements
- Investing in technology and workforce development
- Contributing data and insights to support evaluation efforts
The scoring structure also incentivizes states that may not yet be fully aligned to implement new initiatives or make policy changes that would improve their technical scores and secure greater funding. States and their partners will need to be united on the goals and initiatives, disciplined about implementing and evaluating the plans based on data informed reports, nimble and willing to make strategic pivots based on feedback and experiences.
Connect With Us
States that are already aligned with Trump Administration priorities—such as those with established value-based payment models, short-term limited duration plan options, preferred technology infrastructure, or strong rural hospital support policies—are positioned to be rewarded in the scoring and funding process.
Health Management Associates (HMA), is actively supporting states in developing compliant and compelling RHTP applications. Our advisory services include:
- Strategic assessments and stakeholder engagement
- Program design and grant writing
- Implementation support and technical assistance
- Actuarial support
- Evaluation and performance monitoring
We help clients navigate the complexities of federal funding, align transformation goals with community needs, and build sustainable models for rural care delivery. For details about the RHTP, including the HMAIS State Action Tracker, contact HMA experts Alessandra Campbell, Andrea Maresca, Gabby Palmieri, and Greg Uszak.
MAHA Children's Health Strategy Report: Driving a New Era for Child Health Policy
The September 2025 release of the “Make Our Children Healthy Again Strategy Report” marks a pivotal moment in the Trump Administration’s effort to address childhood chronic disease. Building on the work of the Make America Healthy Again (MAHA) Commission—established by executive order in February 2025 and led by US Health and Human Services (HHS) Secretary Robert F. Kennedy, Jr.—the Strategy Report provides a proposed road map for federal, state, and local action.
The MAHA child-focused Strategy Report is already driving the Trump Administration’s healthcare agenda. Though the report sets ambitious goals, public health entities, state governments, and other experts have raised concerns that several recommendations run counter to established scientific research or lack sufficient evidence.
In this article, Health Management Associates (HMA) experts highlight the areas of focus in the Make Our Children Healthy Again Strategy Report and offer specific recommendations, initiatives, and considerations for stakeholders. Earlier editions of In Focus have addressed the commission’s formation, initial assessment, and the administration’s growing focus on childhood health (Spotlight on Development of President Trump’s Children’s Health Strategy).
Key Components of the MAHA Strategy
Advancing Critical Research to Drive Innovation
The strategy identifies broad areas of research to inform healthy outcomes and positions HHS to direct initiatives in collaboration with the US Food and Drug Administration (FDA), the Centers for Disease Control and Prevention (CDC), and other agencies. Examples include:
- Support the MAHA Chronic Disease Initiative, advance the Real-World Data Platform linking data from claims, electronic health records (EHRs), and wearables
- Establish a working group on mental health diagnosis and prescription, led by several HHS agencies, to focus on SSRIs (selective serotonin reuptake inhibitors), antipsychotics, mood stabilizers, and stimulants
- Study food for health, with the National Institutes of Health (NIH) Office of Nutrition coordinating research initiatives across HHS and the US Departments of Agriculture and Veterans Affairs (VA)
- Identify opportunities to strengthen the use of repurposed drugs for chronic disease
- Address vaccine injury data collection and analysis, as well as mental health research focused on screen time and prescription practices
Realigning Incentives and Systems to Drive Health Outcomes
The report recommends improvements to transparency and efficiency in regulatory processes to address nutrition, fitness, pharmaceuticals and vaccines, and care delivery and payment to address chronic disease. Specific initiatives include:
- Updating the Dietary Guidelines for Americans and developing an “ultra-processed food” definition
- Promote breastfeeding through the Special Supplemental Nutrition Program for Women, Infants, and Children
- Updating hospital food service nutrition guidance
- Developing options to get “MAHA boxes” of healthy food to Supplemental Nutrition Assistance Program (SNAP) enrollees
- Support states with SNAP waivers to encourage healthy food purchases among SNAP participants
- Enhance oversight of direct-to-consumer pharmaceutical advertising and develop a new vaccine framework
- Establish Medicaid managed care quality metrics for nutrition coaching and fitness, and work with states to develop prescribing safeguards for school-age children
- Promote evidence-based prevention and wellness initiatives and restructure agencies to reduce conflicts of interest
Increasing Public Awareness and Knowledge
Major campaigns will involve:
- Launching the “Make American Schools Healthy Again” initiative to assist states with promoting physical activity and nutrition in schools
- Expanding education on environmental exposures, fluoride, and pesticide safety
- Increasing awareness of opioid dangers, vaping, and screen time impacts
- Training school and library staff to respond to opioid overdoses
Fostering Private Sector Collaboration
The strategy emphasizes the administration’s work to advance private sector partnerships aligned with MAHA priorities, including partnerships to achieve the following:
- Improve nutrition in government-funded programs (schools, VA hospitals, prisons)
- Support community-led initiatives to reduce chronic disease in children
Key Considerations for Partners and Stakeholders
Early engagement is critical as federal agencies begin implementing over 120 recommended actions.
States, providers, health plans, and community organizations should identify how their current approaches to children’s health could align with the MAHA initiative and strategy report, as well as where these new ideas might conflict with present policies. This assessment will identify opportunities to maximize new federal funding opportunities and additional resources.
Progress toward the Strategy Report’s specific goals will require coordinated efforts across agencies, sectors, and communities. Stakeholders should consider how and when to engage in research, policy development, and public awareness campaigns outlined in the report.
Connections to Trump Administration Priorities and Broader Opportunities
The report’s recommendations are already influencing federal agency actions and are driving congressional hearings and new legislation at the federal and state levels.
The US Department of Agriculture’s (USDA), for example, is working with states to approve SNAP waivers to restrict the purchase of junk food with federal benefits. HMA experts are tracking the SNAP waiver actions, and as of September 2025, a total of 12 states have received USDA approval for waivers that restrict the purchase of soda, candy, and other unhealthy foods with SNAP benefits. Other states are considering similar waivers, and the USDA is providing technical assistance to support these efforts.
The FDA has enhanced oversight of direct-to-consumer pharmaceutical advertising, including new enforcement activities and rulemaking on drug safety disclosures in ads. This approach aligns with MAHA recommendations and Trump Administration priorities for transparency and consumer protection.
HHS is also pursuing a new vaccine framework; however, states retain significant authority over school-based immunization requirements, and several are considering alternative approaches or maintaining broader vaccine recommendations than those outlined in the MAHA report. Recent legislative actions in some states seek to shift authority for determining school-based immunization requirements solely to the legislature, reflecting ongoing debate and federal-state dynamics.
Connect with Us
As implementation of the Make Our Children Healthy Again Strategy Report advances, all stakeholders must be ready to engage, partner, innovate, and drive change that will shape the future of child health.
HMA guides state and local government, providers, plans and other partners through the multi-pronged strategies and recommendations in the report as well as the complexities of federal funding opportunities, such as the new Rural Health Transformation Program. We are helping state and local policymakers plan for MAHA and Trump Administration priorities, which includes guidance on how to leverage innovative approaches like SNAP waivers to promote healthy food access for children and families.
With deep expertise in policymaking and operational management, HMA consultants are enabling states and their partners to accelerate their work, build sustainable models for child health improvement, and position themselves to take advantage of new federal, state, and local policy opportunities driven by the MAHA report. To discuss questions about the impact of the report contact Jean Glossa and Andrea Maresca.
HMA Conference: Important Insights, Facilitated Introductions, Real Impact
As states and organizations across the country are navigating tight budgets and difficult decisions, Health Management Associates (HMA) recognizes the challenge and is committed to supporting leaders and teams who are driving change. That’s why we’re offering a special discount code: FLASH25 for this year’s HMA National Conference. We want to make it easier for you to gain important insights, be inspired by innovations changing the healthcare landscape, and connect with other healthcare leaders Oct. 14-16, in New Orleans, LA.
Why Attend the HMA National Conference?
This is not just another industry event. The HMA National Conference brings together an unmatched group of thought leaders, decision makers, experienced administrators, and innovators from across the health policy, government, community, and industry sectors. In today’s environment, it is more important than ever to get out to events, build your network, and engage with the people who are shaping the future of health care.
What makes the HMA event different?
- Networking that Matters: This is your opportunity to connect with peers and leaders who understand the challenges you are facing and can offer practical solutions and inspiration. HMA experts are there to facilitate introductions and make the connections that are not possible at other meetings.
- Unparalleled Caliber of Attendees: You will not find this mix of roles and expertise anywhere else. Our attendees include those developing and championing policy, investing in infrastructure, leading growth initiatives, process efficiency leaders, and those advancing value and access across the continuum—from physical and behavioral health to the social determinants of health.
- Comprehensive Agenda: The conference agenda is designed to tackle the most pressing issues, including policy and budget reprioritization, infrastructure investments, optimizing digital health technology and AI, consumer empowerment, process efficiency, and strategies to improve value and access to services. We have powerhouse speakers lined-up to challenge and inspire you.
Acknowledging Budget Realities
HMA understands the financial pressures facing organizations and agencies across the health care sector. Our work with clients and partners gives us a unique perspective on the tough choices leaders are making every day. That’s why we want to help make participation at the 2025 HMA National Conference possible. Use code FLASH25 for a 25% discount on registration—because we believe that investing in your professional growth and connections is more important than ever.
Join Us
Whether you’re focused on policy, operations, IT, consumer engagement, or strategy and growth, the HMA National Conference is the place to find the people, ideas, and strategies that will help you tackle today’s challenges and prepare for tomorrow’s opportunities. For more information about the event contact Andrea Maresca.
HMA Roundup
Georgia
Georgia Rural Hospital to Close Labor, Delivery Unit Due to Medicaid Cuts. The Georgia Recorder reported on September 17, 2025, that St. Mary’s Sacred Heart Hospital in Lavonia, Georgia, will shut down its labor and delivery services next month, forcing pregnant patients in four rural counties to travel for maternal care. Hospital leaders cited recent federal Medicaid cuts under H.R. 1, physician shortages, and changing demographics as key drivers of the decision. Only about one-third of Georgia’s rural hospitals still deliver babies. Other hospitals in Georgia are also discussing scaling back services as Medicaid cuts are expected to deepen financial strain.
Idaho
Idaho Seeks $60 Million Supplemental Medicaid Funding Amid Rising Costs. The Idaho Capital Sun reported on September 12, 2025, that the Idaho Department of Health and Welfare has requested an additional $60 million in Medicaid funding for fiscal year 2026 to cover rising costs and ensure timely provider payments, even after a 4 percent reimbursement rate cut intended to save $30 million. Officials cite higher health care utilization and more intensive services as key cost drivers, along with a $22 million accounting error tied to the state’s new business system. If not approved, payments to providers could be delayed until fiscal 2027. Looking ahead, the agency’s fiscal 2027 budget request includes about $2.9 million to implement new Medicaid cost-cutting measures, such as work requirements and twice-a-year eligibility checks, in line with state law and federal policy changes.
Illinois
Illinois Releases HealthChoice Medicaid Managed Care RFP. The Illinois Department of Healthcare and Family Services (HFS) issued on September 15, 2025, a request for proposals (RFP) for HealthChoice Illinois (HCI), the state’s statewide Medicaid managed care program. The program covers about 2.4 million members statewide. The state is seeking Medicaid managed care organizations (MCOs) that can deliver comprehensive, equitable, whole-person care, with a strong focus on:
• high-quality benefits with efficient and effective service delivery
• holistic, proactive care that prioritizes enrollee needs, addresses social determinants of health, and improves overall health outcomes
• availability and accessibility of care
• quality management by incentivizing providers through performance-based payment models (e.g. Alternative Payment Models)
MCOs will cover families and children, Medicaid expansion adults, special needs children, individuals with disabilities, and other Medicaid-eligible individuals who are not eligible for Medicare.
Bidders may propose either statewide coverage (up to five awards) or Cook County-only coverage (up to two awards). Each MCO will also be required to execute two contracts: the HCI Model Contract for Federally Funded Managed Care Services and the HCI Model Contract for State Funded Managed Care Services, to comply with the Centers for Medicare & Medicaid Services 2025-2026 Medicaid Managed Care Rate Development Guide, which requires state-funded services to be placed in a distinct contract vehicle.
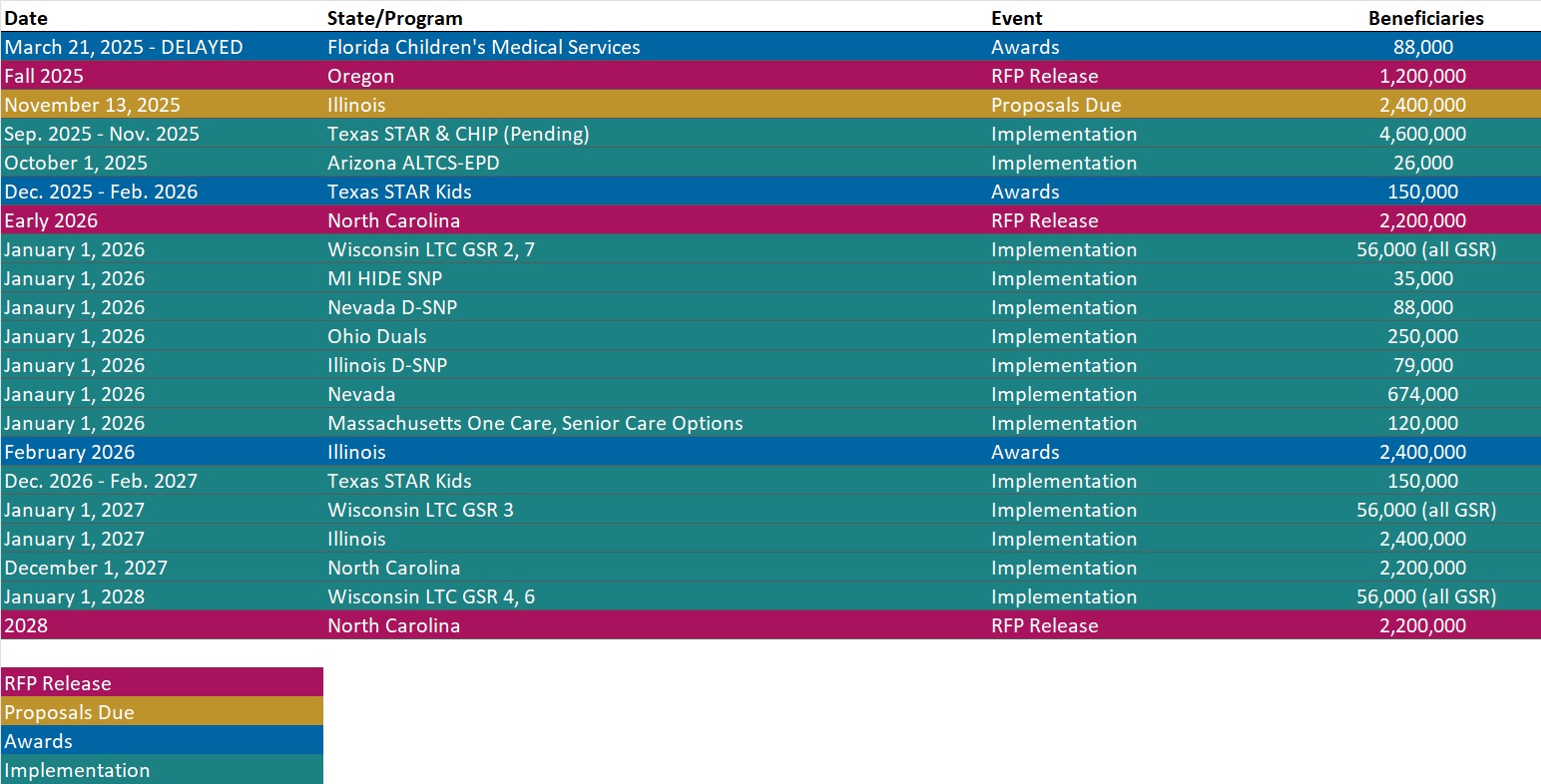
Responses are due November 13, with awards expected in February 2026. The contracts are expected to begin July 2026, with operations starting January 1, 2027, and run through December 2030, with renewal options for up to 10 years in total. Current incumbents are Blue Cross Blue Shield of IL, Cook County Health/CountyCare Health Plan, CVS/Aetna Better Health, Molina, Centene/Meridian Health Plan.
Louisiana
Louisiana Issues PACE RFI. The Louisiana Department of Health (LDH) released on September 15, 2025, a request for information (RFI) seeking input to potentially develop a Program of All-Inclusive Care for the Elderly (PACE) in the Shreveport area. LDH welcomes feedback from relevant stakeholders on available resources in the area, as well as resources that need to be developed, that will help PACE providers fully support the program’s potential participants. Responses are due October 31, 2025.
North Carolina
North Carolina to Expand Mobile Crisis Clinics. North Carolina Health News reported on September 16, 2025, that North Carolina is turning to mobile crisis clinics to help expand treatment for substance use disorder, especially for people living in rural areas. The state’s first mobile clinic opened in July 2025 and the second mobile clinic is set to open in the coming weeks. The state Department of Health and Human Services received $3.75 million to fund six mobile clinic units after Hurricane Helene, and there may be as many as 10 additional mobile clinics that open in upcoming months, according to the State Opioid Treatment Authority.
National
House Stopgap Bill Extends Health Programs, Omits ACA Subsidies. Modern Healthcare reported on September 16, 2025, that House Republicans have proposed a stopgap bill to fund the government through November 21, extending key health programs such as telehealth, hospital-at-home, and Medicaid disproportionate share hospital funding, but not addressing the expiring enhanced Affordable Care Act (ACA) marketplace subsidies. GOP leaders, led by Speaker Mike Johnson (R-LA), argue the subsidies do not expire until year-end and should not be part of a short-term measure. Democrats counter that failing to act now will raise premiums and destabilize coverage, setting up a funding standoff.
Lawmakers Submit Letter Urging HHS to Scrap 340B Pilot Rebate Plan. Fierce Healthcare reported on September 10, 2025, that a bipartisan group of 163 lawmakers has sent a letter to the U.S. Department of Health and Human Services (HHS) urging the agency to cancel a new pilot that would issue after-the-fact rebates for hospital drugs purchased through the 340B drug discount program. The letter states that the pilot will require 340B providers to float cash to pharmaceutical companies and are not always guaranteed to be paid rebates, which could damage community health centers, safety net hospitals, and other 340B providers. It goes on to state that Disproportionate Share Hospitals are estimated to have to float $72.2 million annually to the companies under this pilot. If HHS chooses to move forward with the pilot, lawmakers requested more details outlining how it would shield hospitals and the government from additional administrative burden before the application opens on September 15, 2025.
Industry News
NCQA Releases 2025 Health Plan Ratings. Fierce Healthcare reported on September 16, 2025, that the National Committee for Quality Assurance (NCQA) released the 2025 Health Plan Ratings, based on HEDIS and CAHPS measure ratings. A total of 11 health plans received 5-star rating in 2025, including three Medicare plans, more than doubling last year’s total. The report noted improvements in Medicare care coordination and continuity, as well as significant progress across diabetes-related measures, particularly kidney health evaluations. Adult and adolescent immunization rates also improved, while childhood vaccination rates continued to decline, though at a slower pace. NCQA added a new “Language Diversity of Membership” metric this year to help identify communication gaps and promote more equitable care.
RFP Calendar
Actuaries Corner
Mayo Clinic to Close 6 Clinics, Consolidate Service Lines. The nonprofit provider said low patient volumes and persistent staffing shortages motivated the decision. Editor’s Note: Mayo Clinic plans to close six of its clinics in Minnesota by Dec. 10. It is consolidating services in part to address lower patient volumes and staffing shortages. Experts warn that rural hospital cuts and closures could increase as implementation of the One Big Beautiful Bill Act begins.
Discover other developments in the Wakely Wire here.
HMA News & Events
HMA Webinar
Beyond Bundles: Preparing Hospitals for Success in TEAM and the Next Generation of Value-Based Models. Tuesday, September 30, 2025, 12 PM ET. Hospitals and health systems are under growing pressure to succeed in new value-based models that demand both operational transformation and strategic alignment. In this webinar, advisors from Health Management Associates, Wakely, an HMA Company and Nixon Peabody will break down the latest regulatory and contractual developments, explore lessons learned from the Comprehensive Care for Joint Replacement (CJR) model, and discuss how organizations can prepare for upcoming opportunities.
Speakers will share practical insights on:
- The regulatory, operational, and actuarial considerations hospitals must navigate
- Key takeaways from bundled payment initiatives like CJR
- How to leverage data and design strategies to build partnerships that position organizations for success in new Medicare models
This session is designed for hospital executives, provider organizations, payers, and policy leaders seeking to better understand how emerging value-based models will shape the future of care delivery and payment.
Beyond the Bill: How Pair Team and MCOs Are Meeting Community Needs Under HR 1. Thursday, October 2, 2025, 1 PM ET.
As Medicaid evolves under HR 1, Managed Care Organizations face increasing pressure to meet new engagement requirements while ensuring vulnerable communities don’t fall through the cracks. This shifting landscape demands scalable, innovative care models that go beyond compliance – focusing instead on meaningful connections, coordinated support, and whole-person care.
In this session, Jami Snyder, former HHSC Commissioner of TX and Medicaid Director of AZ, joins Neil Batlivala, CEO and Co-Founder of Pair Team, and Dr. Nate Favini, Chief Medical & Strategy Officer, to explore how Pair Team and its MCO partners are meeting this moment. Learn how their model combines technology, care coordination, and community-based partnerships to engage hard-to-reach members and address social drivers of health. You’ll hear real-world examples of how payers and partners can come together in smarter, more connected ways. By aligning efforts and building trust, they can drive better outcomes and create stronger community connections for the people who need support the most.
Medicaid 1115 Justice Involved Reentry Demonstration Opportunities: Engaging Key Stakeholders. Wednesday, October 22, 2025, 12 PM ET. This webinar will explore how states, local agencies, and community organizations can maximize Medicaid’s new 1115 demonstration authority to improve reentry outcomes for justice-involved individuals. Presenters will discuss practical strategies for assessing health and social needs, building strong collaborations with community providers, and implementing effective Medicaid enrollment processes. Attendees will gain insights into designing and operationalizing reentry programs that promote continuity of care, reduce recidivism, and support successful community reintegration. This session is ideal for State Medicaid agencies, carceral facilities, correctional healthcare companies, health plans, community-based organizations, and federally qualified health centers.
NEW THIS WEEK ON HMA INFORMATION SERVICES
(Exclusive Access for HMAIS Subscribers):
HMAIS Medicaid Market Overviews, Reports, and Data
- Updated HMA Federal Health Policy Snapshot
- New Medicaid enrollment, RFP documents, and other market intelligence resources for dozens of states
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services.
If you’re interested in becoming an HMAIS subscriber, contact Andrea Maresca at [email protected].