This week's roundup:
- In Focus: Delaware Substance Use Disorder Treatment System Needs Assessment

- HMA Conference: Registration Ending Soon

- Kentucky Seeks to Expand Number of PACE Providers, Counties Served

- Montana Medicaid Reimbursement Rates Are 22 Percent Below Benchmarks, Study Finds

- New York Proposes 1115 Waiver Amendment to Address Equity, Housing, Workforce Shortages

- Oregon Medicaid Mobile Crisis Intervention Services Program Receives CMS Approval

- Texas Awards STAR Health Contract to Centene/Superior HealthPlan

- CareSource, Legacy Community Health Form Joint Venture to Bid on Texas STAR, CHIP RFP

- CMS to Phase Out D-SNP Look-Alikes Within Medicare Advantage in 2023

- Illinois Review Board to Reconsider Merger of Advocate Aurora, Atrium Health

In Focus
Delaware Substance Use Disorder Treatment System Needs Assessment
This week, our In Focus highlights a Health Management Associates Institute on Addiction (HMA IOA) report, Delaware Substance Use Disorder Treatment System Needs Assessment, published in June 2022. HMA IOA conducted a statewide three-county substance use disorder (SUD) treatment system needs assessment in Delaware. This project began in November 2021 and was primarily funded by New Castle County with contributions from Kent and Sussex counties. The goal was to review the current state of the SUD treatment ecosystem, identify strengths and gaps collecting input from as many Delawareans across multiple sectors as possible, and make actionable recommendations to build a more robust and sustainable future state system.
The final analysis included interviews with key stakeholders, focus groups, a survey of all licensed SUD providers, claims data analysis, and a comparison of Delaware’s public (e.g., Medicaid) outpatient and residential SUD reimbursement rates with selected regional states. This approach provided a unique cross-sector view of where the most significant opportunities for improvement and investment may rest.
The areas of greatest experienced need in the system were reported as: inadequate treatment beds, especially for some populations, like children and youth; lack of residential services for adults, especially those on Medicare and without insurance; needed supports for those experiencing negative impacts from social determinants of health (SDOH), like transportation and housing needs; lack of consistent access and care coordination; lack of adequate reimbursement to sustain the system or expand the treatment system; the need for trauma-informed care (TIC); and the need for more harm reduction and prevention strategies, including greater access specifically to Narcan 4mg Nasal Spray or its generic equivalent.
The study found that Delaware is meeting only 15 percent of SUD treatment needs and only meeting five percent of the need for the highest-intensity services, including inpatient treatment.
The results also showed an apparent discrepancy between what the state is working hard to implement to address the SUD and overdose crisis in Delaware and the community’s perception of, or lived experience with, those SUD treatment services and supports. Additionally, HMA IOA heard about many treatment system strengths from interviewees, town hall participants, and focus groups and included recommendations that are meant to leverage those existing strengths in the future treatment system.
Click here to read the report.
HMA Conference: Registration Ending Soon
Registration Ends Sept. 23rd.
More than 45 industry speakers, including health plan executives, state Medicaid directors, policy experts, and providers are confirmed for HMA’s The New Normal: How Medicaid, Medicare, and Other Publicly Sponsored Programs Are Shaping the Future of Healthcare in a Time of Crisis conference, October 10-11, at the Fairmont Chicago, Millennium Park. In addition to plenary sessions on state Medicaid priorities, managed care opportunities, and value-based payments, attendees can choose from breakout sessions on dual eligibles, healthcare investing, successful value-based payment initiatives, technology-enabled integrated care, social determinants of health, and much more.
Register Now.
HMA Roundup
Florida
Florida Faces Lawsuit from Transgender Rights Groups over Medicaid Coverage Determination. Politico reported on September 7, 2022, that a coalition of transgender rights activists has filed a state lawsuit against the Florida Agency for Health Care Administration, alleging that the state’s determination that Medicaid will not cover gender-affirming care violates the U.S. Constitution’s equal protection clause. The complaint also alleges that the state would be denying critical care to 9,000 individuals. Read More
Kentucky
Kentucky Seeks to Expand Number of PACE Providers, Counties Served. The Kentucky Cabinet for Health and Family Services announced on September 13, 2022, that the state has certified two Programs of All-Inclusive Services for the Elderly (PACE) and is looking to expand the number of PACE providers and counties served. The two current PACE organizations are Horizon PACE and Bluegrass Care Navigators, which cover 19 counties. Read More
Montana
Medicaid Reimbursement Rates Are 22 Percent Below Benchmarks, Study Finds. The Montana Free Press reported on September 7, 2022, that Montana’s Medicaid reimbursement rates were 22 percent below benchmarks for comparable providers in other states who care for seniors in assisted-living facilities, individuals with disabilities, and children and adults with mental illnesses and addiction, according to a study commissioned by the state legislature and performed by Guidehouse. The study also found that it would cost $82 million annually in state and federal funding to bring the state up to par. Read More
New Jersey
Health Partners Plans to Offer Medicare Advantage Options in New Jersey. The Philadelphia Inquirer reported on September 12, 2022, that Pennsylvania insurer Health Partners Plans will expand into Burlington, Camden, and Gloucester counties in New Jersey, with a Medicare Advantage (MA) offering. Open enrollment for the 2023 coverage year will begin on October 15, 2022. Health Partners Plans, which offers MA and Medicaid plans in Pennsylvania, is now fully owned by Thomas Jefferson University. Read More
New York
Lawmakers Urge U.S. Senate to Pass Legislation to Provide Continuity of Medicaid Coverage for Foster Care Youth. Spectrum News reported on September 9, 2022, that a group of New York state lawmakers sent a letter to U.S. Senators Chuck Schumer (D-NY) and Kirsten Gillibrand (D-NY) urging the Senate to pass the Ensuring Medicaid Continuity for Children in Foster Care Act of 2021, which would ensure Medicaid eligibility for children and youth in foster care. Currently, not all foster children are able to obtain Medicaid coverage. Read More
New York Proposes 1115 Waiver Amendment to Address Equity, Housing, Workforce Shortages. The New York Department of Health proposed on September 2, 2022, a Medicaid Redesign Team 1115 Waiver amendment aimed at addressing health equity, developing transitional housing for individuals at risk of institutionalization, redesigning state systems addressing quality and workforce shortages, and creating digital health and telemedicine infrastructure statewide. The state submitted the proposal to the Centers for Medicare & Medicaid Services for approval.
North Carolina
North Carolina Medicaid Official Urges Lawmakers to Expand Medicaid This Year to Maximize Federal Funding. WGHP reported on September 7, 2022, that North Carolina secretary for Health and Human Services Kody Kinsley urged state lawmakers to expand Medicaid and establish the Healthcare Access and Stabilization Program this year or lose more than $1 billion in federal funds, more than half of which would go toward mental health, rural health and other initiatives. Kinsley noted that thousands of individuals will lose coverage when the public health emergency ends if the state does not expand Medicaid. Read More
Oklahoma
Task Force Recommends Raising Income Eligibility Limit for Pregnant Women, Extending Postpartum Coverage to 12 Months. The Tulsa World reported on September 13, 2022, that a task force created by Oklahoma Governor Kevin Stitt recommended that the state extend Medicaid postpartum coverage to 12 months from 60 days and increase the Medicaid eligibility income limit for pregnant woman to 205 percent of poverty. The current limit is 138 percent. The recommendations would extend coverage to 2,500 women in the state. Read More
Oregon
Oregon Medicaid Mobile Crisis Intervention Services Program Receives CMS Approval. The Centers for Medicare & Medicaid Services (CMS) announced on September 12, 2022, approval of the Oregon Health Authority’s state plan amendment (SPA) to offer Medicaid community-based mobile crisis intervention services for individuals experiencing mental health and substance use crises. The SPA was made possible through the American Rescue Plan Act. Read More
Texas
Texas Awards STAR Health Contract to Centene/Superior HealthPlan. The Texas Health and Human Services Commission announced on September 13, 2022, its intent to award incumbent Centene/Superior HealthPlan a contract for Texas STAR Health, the state’s Medicaid managed care program for children and youth in foster care. Implementation is scheduled between September 2023 and November 2023. Read More
CareSource, Legacy Community Health Form Joint Venture to Bid on Texas STAR, CHIP RFP. The Dayton Daily News reported on September 13, 2022, that CareSource and Legacy Community Health have formed a joint venture called CareSource Bayou Health to bid on the Texas STAR Program and Children’s Health Insurance Program (CHIP). Legacy is a Federally Qualified Health Center serving Texas. The request for proposals (RFP) is expected to be released between December 2022 and February 2023. Read More
West Virginia
West Virginia Allocates Funding to Increase Medicaid HCBS Payments. Becker’s Hospital Review reported on September 12, 2022, that the West Virginia Department of Health and Human Services has allocated $240 million to increase Medicaid reimbursement rates for home and community-based services (HCBS) providers. The funds, which will be available October 2022 pending federal regulatory approval, will run through the state’s Aged and Disabled Waiver, Intellectual/Developmental Disabilities Waiver, and Children with Serious Emotional Disorders Waiver. At least of 85 percent of the increased funds must go toward increased wages and benefits for direct-care workers. Read More
Wisconsin
Joint Finance Committee Allocates $1 Million to Address SUD Among Medicaid Beneficiaries. Wisconsin Health News reported on September 8, 2022, that the Wisconsin Joint Finance Committee unanimously approved the allocation of $1 million to expand the state’s pilot program to address substance use disorders (SUDs) for Medicaid beneficiaries. The allocation is part of a broader state Department of Health Services spending plan for $31 million in opioid settlement funds. The plan also provides $2 million for SUD medication-assisted treatment. Read More
National
CMS Approves Extension of Postpartum Coverage to 12 Months in Indiana, West Virginia. The Centers for Medicare & Medicaid Services (CMS) announced on September 8, 2022, that it has approved the extension of postpartum Medicaid and Children’s Health Insurance Program (CHIP) coverage to 12 months in Indiana and West Virginia. The extensions will provide coverage for 15,000 individuals in the two states. Read More
CMS to Phase Out D-SNP Look-Alikes Within Medicare Advantage in 2023. Hospice News reported on September 12, 2022, that the Centers for Medicare & Medicaid Services (CMS) will phase out dual-eligible special needs plan (D-SNP) look-alikes within Medicare Advantage (MA) in 2023. MA plans began offering D-SNP look-alikes in recent years, which are not subject to the same regulations as actual D-SNPs. There are about 12 million individuals who are dually eligible, with about 3.8 million enrolled in D-SNPs. Read More
CMS to Resume Standard Process for Calculating Medicare Advantage Star Ratings. Modern Healthcare reported on September 12, 2022, that the Centers for Medicare & Medicaid Services (CMS) will resume the standard process for calculating Medicare Advantage (MA) star ratings, which was relaxed in 2021 and 2022 due to COVID-19. The relaxed process resulted in a record number of insurers receiving higher scores and an increase in federal spending on bonuses. MA plans received $9.2 billion in bonuses in 2021 and will receive an estimated $10 billion in 2022, which is more than triple what they received in 2015. Read More
Medicaid Drug Rebate Case to Be Heard by Full 4th Circuit Court of Appeals. Reuters reported on September 12, 2022, that the full 4th U.S. Circuit Court of Appeals will hear arguments in a Medicaid False Claims Act lawsuit alleging that Allergan’s Forest Laboratories defrauded the Medicaid program by reporting inaccurate drug pricing data to the Centers for Medicare & Medicaid Services. Previously, a panel of judges ruled in Forest Laboratories’ favor in a split decision. Read More
Lack of Medicaid Expansion Correlates to Rural Hospital Closures, Report Finds. Becker’s Hospital Review reported on September 9, 2022, that 74 percent of the 136 rural hospitals that closed between 2010 and 2021 occurred in states where Medicaid expansion was not implemented or had been in place for less than a year, according to report from the American Hospital Association. The report also found that rural hospitals require increased state and federal resources to address barriers and called on Congress to extend the Medicare-dependent Hospital program and the Low-Volume Hospital program, which are set to expire October 1. Read More
Medicare Telehealth Usage Rises, Largely in Urban Areas, OIG Reports Find. Modern Healthcare reported on September 8, 2022, that telehealth service usage rose dramatically in the first year of the pandemic versus the previous year, according to a report by the U.S. Office of Inspector General (OIG). However, Medicare telehealth fraud remained low. The report found that two in five Medicare beneficiaries utilized telehealth during the first year of the pandemic, with overall usage up 88 times the prior year. Another OIG Report found that Medicare beneficiaries in urban areas were more likely to use telehealth services than those in rural areas during the first year of the pandemic, with 20 percent of beneficiaries using audio-only telehealth services. Read More
Industry News
Agape Care Group Acquires GHC Hospice. Agape Care Group announced on September 14, 2022, its acquisition of GHC Hospice, a hospice care provider in Georgia and South Carolina. Agape Care is a portfolio company of Ridgemont Equity Partners. Read More
Illinois Review Board to Reconsider Merger of Advocate Aurora, Atrium Health. Modern Healthcare reported on September 13, 2022, that the Illinois Health Facilities & Services Review Board said it will reconsider its initial opposition to change-of-ownership exemptions that would allow Advocate Aurora to merge with Atrium Health. The merged not-for-profit health system would operate 67 hospitals under the Advocate Health name and serve 5.5 million patients annually. Read More
Pharos Capital Announces ‘Significant’ Investment in Renal Care 360º. Pharos Capital announced on September 12, 2022, an investment in Renal Care 360°, a nephrology practice and chronic care management company with a focus on underserved, rural communities. Renal Care 360° founder Joe Cashia will remain chairman and chief executive. Read More
CVS Health/Aetna to Offer Exchange Plans in California, Delaware, Illinois, New Jersey. Fierce Healthcare reported on September 12, 2022, that CVS Health/Aetna will offer Exchange plans in California, Delaware, Illinois, and New Jersey in 2023, in addition to the eight states in which it already offers Exchange plans. Open enrollment begins November 1, 2022. Read More
AbsoluteCare Names Chris Goldsmith President of ACO Division. AbsoluteCare announced on September 8, 2022, that Chris Goldsmith was named president of the company’s Accountable Care Organization (ACO) division. Goldsmith previously served stints at Vault Health and Landmark Health. Read More
UnitedHealthcare Hopes to Offer Exchange Plans in Kansas, Mississippi, Missouri, Ohio. The Star Tribune reported on September 7, 2022, that UnitedHealthcare is seeking regulatory approval to offer Exchange plans in Kansas, Mississippi, Missouri, and Ohio in 2023. Currently, UnitedHealthcare offers Exchange plans in 18 states. Read More
Walmart to Provide Preventative Care Services to UnitedHealth Medicare Advantage Beneficiaries. Modern Healthcare reported on September 7, 2022, that Walmart will provide preventive health care services to UnitedHealth Group Medicare Advantage (MA) beneficiaries in Florida and Georgia under a 10-year deal, beginning on January 15. The arrangement is expected to be expanded into additional states. The two companies are also marketing a co-branded MA plan in Georgia. Read More
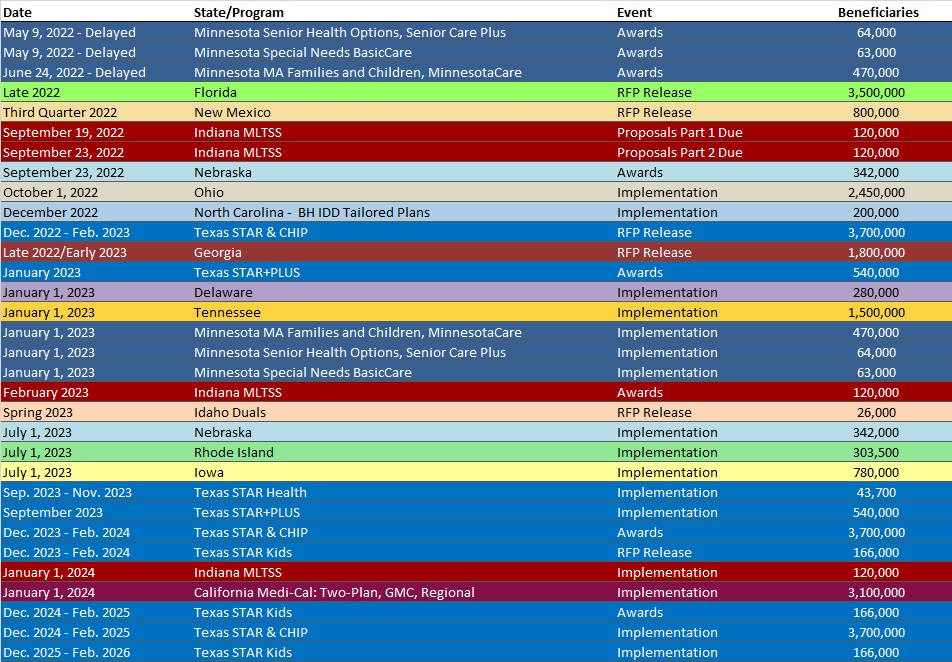
RFP Calendar
HMA News & Events
HMA WELCOMES
Nic Kohler, Managing Director, Corporate Development – Tallahassee, FL
Nic Kohler is a strategic impact-focused leader with a strong quantitative background and extensive experience executing acquisitions and optimizing businesses.
He has managed corporate development teams and transactions for over 20 years with a focus on healthcare services businesses. His main expertise is related to government sponsored healthcare, managed care payers, healthcare services and providers.
Nic joined HMA as the managing director of corporate development services where he oversees HMA’s services across the government sponsored, healthcare information technology, and healthcare services segments.
Prior to joining HMA, he served as senior vice president, strategy & development at Alignment Healthcare. Earlier in his career Nic held corporate development leadership positions at Anthem (now Elevance), PRA group, Xerox and Amerigroup.
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Florida Medicaid Managed Care Enrollment is Up 4.1%, May-22 Data
- Michigan Medicaid Managed Care Enrollment is Up 1.4%, Apr-22 Data
- Michigan Dual Demo Enrollment is Down 1.9%, Apr-22 Data
- Mississippi Medicaid Managed Care Enrollment is Down 12.1%, Aug-22 Data
- Nebraska Medicaid Managed Care Enrollment Is Up 4.8%, May-22 Data
- Nevada Medicaid Managed Care Enrollment is Up 2.8%, May-22 Data
- New Mexico Medicaid Managed Care Enrollment is Up 1.3%, Jun-22 Data
- New Mexico Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
- New York Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
- North Carolina Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
- Ohio Medicaid Managed Care Enrollment is Up 0.8%, Mar-22 Data
- Oklahoma Medicaid Enrollment is Up 6%, May-22 Data
- Pennsylvania Medicaid Managed Care Enrollment is Up 3.1%, May-22 Data
- Puerto Rico Medicaid Managed Care Enrollment is Up 1.8%, Aug-22 Data
- Tennessee Medicaid Managed Care Enrollment is Up 2.5%, May-22 Data
- Washington Medicaid Managed Care Enrollment is Up 2.2%, May-22 Data
Medicaid Financials and Utilization Data:
- MLRs at Nevada Medicaid MCOs Average 78.1%, 2021 Data
- MLRs at New Mexico Medicaid MCOs Average 83%, 2021 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- California Medi-Cal Managed Care Two-Plan, GMC, and Regional Models RFP, Proposals, Evaluation, Awards, and Appeals, Sep-22
- Delaware Medicaid Managed Care RFP, Proposals, Scoring, and Awards, 2021-22
- Maryland Behavioral Administrative Services Organization (ASO) RFP, Proposals, and Contract, 2018-19
- Mississippi MississippiCAN and CHIP RFQ, Amendments, Proposals, Scoring, and Award, 2021-22
Medicaid Program Reports, Data, and Updates:
- New Carolina Medicaid Consumer Assessment of Healthcare Providers and Systems Report and Summary, 2021
- North Carolina Medicaid EQRO Annual Technical Report, 2021
- North Carolina Medicaid HITECH Implementation Advance Planning Document, 2019-21
- North Carolina Medicaid Managed Care Quality Strategy, 2018-21
- North Carolina Medicaid Quality Measurement Technical Specifications Manual, Jan-22
- North Carolina Plan for HCBS Implementation of the American Rescue Plan Act and Quarterly Reports, 2021-22
- North Carolina Standard Plan Network Adequacy Reports, 2021-22
- Oregon Health Authority Ombuds Annual Report, 2021
- Tennessee TennCare Annual Reports, FY 2010-21
- Texas COVID-19 Federal Funds Presentation to Legislature, Sep-22
- Texas Initiatives to Reduce Avoidable Emergency Room Utilization and Improve Health Outcomes in Medicaid Report, Aug-22
- Texas Report on Continuity of Care for Women Aging Out of Medicaid and CHIP, Aug-22
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.