HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- The Basics of Evaluating PBM Contracts

- Cityblock to Serve About 10,000 MDWise Members in Indiana

- Kentucky Appeals Panel Upholds 2020 Medicaid Managed Care Contracts With 5 Plans, Excluding Elevance Health

- Missouri Meets Federal Requirement of 45 Days for Processing Medicaid Expansion Applications

- New York PACE Could Expand Dramatically Under Bill Awaiting Governor’s Signature

- Ohio Releases Medicaid Electronic Visit Verification Services RFP

- AbsoluteCare Expands Into Pittsburgh Through Collaboration With Highmark Wholecare

- Tennessee Is Hit With Lawsuit Over Medicaid Managed Care Procurement

- Texas to Receive $165.6 Million in Settlement Over Medicaid Drug Pricing

- Medicaid Eligibility Redeterminations Could Take 12 Months Following PHE, State Regulators Say

- NCQA, CHCF Release Framework to Measure Health Equity in Medicaid Managed Care

- UnitedHealth Group Is Cleared to Acquire Change Healthcare

- Humana to Fully Acquire 20 Senior Primary Care Clinics After Buying Out Welsh, Carson’s Stake

In Focus
The Basics of Evaluating PBM Contracts
This week, our In Focus section highlights an issue brief from Wakely, an HMA Company, The Basics of Evaluating PBM Contracts, published September 2022. The brief provides an overview of the basic financial elements of a pharmacy benefit manager (PBM) contract. Evaluation of a traditional request for proposals (RFP) or PBM contract should begin with financial analysis of the following four key elements: discount guarantees (typically understood as point-of-sale ingredient costs), dispensing fees, rebate guarantees, and PBM administrative fees. This paper addresses various points of consideration when attempting a financial analysis of these contract elements.
Payors today face unprecedented degrees of complexity when conducting a PBM RFP or evaluating PBM contracts. To stay competitive, payors must navigate an ambiguous and changing pricing environment. That requires a solid understanding of PBM contracting. In a proposal, some PBMs may offer better AWP discounts while other PBMs offer better rebate guarantees. Alternatively, a payor may find a PBM that offers the best discounts and rebates but charges significantly higher administrative fees. Such analysis will consider the impacts of these key components together with historical and projected drug mix. While any PBM analysis must start with the elements discussed in this paper, a complete analysis must dive below the surface and into the fine print underlying these items.
HMA Roundup
California
California Enacts Law to Deliver Court-Ordered Behavioral Health Care to Homeless. The Associated Press reported on September 14, 2022, that California Governor Gavin Newsom signed legislation to deliver court-ordered mental health and substance use disorder services to individuals with severe mental illness beginning October 1, 2023. The law, which is aimed at the state’s homeless population, allows family members, first responders, and others to request a court-ordered care plan that could run up to two years and include medication, housing, and therapy. Read More
Indiana
Cityblock to Serve About 10,000 MDWise Members in Indiana. Fierce Healthcare reported on September 20, 2022, that Cityblock Health has expanded into Indiana to provide community-based primary care, behavioral health care, and social services to about 10,000 MDwise Medicaid manged care members. Read More
Kentucky
Kentucky Appeals Panel Upholds 2020 Medicaid Managed Care Contracts With 5 Plans, Excluding Elevance Health. The Louisville Courier Journal reported on September 15, 2022, that a three-judge panel of the Kentucky Court of Appeals upheld the state’s 2020 selection of CVS Health/Aetna Better Health of Kentucky, Humana Health Plan, Centene/Wellcare Health Insurance of Kentucky, UnitedHealthcare, and Passport by Molina to serve as the state’s Medicaid managed care plans. However, the ruling excludes Elevance Health (formerly Anthem Blue Cross Blue Shield), which was added as a sixth plan while the legal dispute was pending. Current contracts will run through December 31, 2024. Read More
Maryland
Maryland Launches Pilot Program Matching Students on Medicaid to Free School Lunch. The Maryland State Department of Education announced on September 15, 2022, a pilot program that allows school districts to use Medicaid data to match students to free or reduced-price lunches, without families completing a meal benefit application. The program, which was approved by the U.S. Department of Agriculture, starts July 1, 2022. Read More
Missouri
Missouri Meets Federal Requirement of 45 Days for Processing Medicaid Expansion Applications. The St. Louis Post-Dispatch reported on September 14, 2022, that the Missouri Department of Social Services (DSS) is now processing Medicaid expansion applications within the federal requirement of 45 days, eliminating a previous backlog, according to DSS acting director Robert Knodell. In July, the Centers for Medicare & Medicaid Services approved a plan to help reduce application processing times. As of August 2022, the state had enrolled 228,361 Medicaid expansion members. Medicaid expansion enrollment began in October 2021. Read More
New York
PACE Could Expand Dramatically Under Bill Awaiting Governor’s Signature. Crain’s New York Business reported on September 21, 2022, that the Program of All-Inclusive Care for the Elderly (PACE) could expand dramatically in New York under a bill passed by the state legislature and now awaiting signature by Governor Kathy Hochul. The legislation streamlines the regulatory framework for PACE programs by developing a uniform authorization process, creating a singular licensure, improving oversight, and establishing a payment rate methodology. Hochul is reviewing the bill, according to a spokesperson. Read More
New York Improperly Claims $84.3 Million in Federal Medicaid Reimbursements for NEMT, HHS Audit Finds. Becker’s Hospital Review reported on September 15, 2022, that New York improperly claimed at least $84.3 million in federal Medicaid reimbursements for non-emergency medical transportation (NEMT) services in New York City, according to an audit from the Department of Health and Human Services (HHS) Office of the Inspector General. The audit also estimated the state claimed $112 million in federal reimbursements that may not have complied with certain federal and state requirements. The audit looked at payments totaling more than $269.5 million for NEMT services in 2018 and 2019. Read More
North Carolina
North Carolina Hospitals Are Open to Certificate of Need Reform to Boost Prospects for Medicaid Expansion. The Triangle Business Journal reported on September 20, 2022, that North Carolina hospitals are now open to certificate of need (CON) reform in hopes of boosting prospects for Medicaid expansion. In a letter to lawmakers, the North Carolina Healthcare Association said it would now accept certain CON reforms, including repealing requirements for chemical dependency and psychiatric beds, and exempting requirements for certain operating rooms in ambulatory surgery centers. Read More
Ohio
Aetna Cancels Contract with Dual Eligible NEMT Vendor. Becker’s Payer Issues reported on September 20, 2022, that Aetna, which operates a Medicaid managed care plan in Ohio, will cancel a contract with its non-emergency medical transportation (NEMT) vendor in the state for dual eligibles, effective December 31, 2022. The health plan cited persistent complaints about late or no-show rides. Read More
Ohio Releases Medicaid Electronic Visit Verification Services RFP. The Ohio Department of Medicaid released on September 19, 2022, a request for proposals (RFP) to provide electronic visit verification (EVV) services for Medicaid home and community-based services. Contracts will run from January 13, 2023, through June 30, 2025, with up to five, two-year renewal options. Sandata Technologies is the current EVV services contract holder for the state. Proposals are due by November 4, 2022. Read More
Ohio Launches Online Childhood Behavioral Health Tool. WTVG/ABC 13 reported on September 15, 2022, that the Ohio Department of Medicaid launched an online behavioral health tool that provides families, teachers, and healthcare providers with resources to navigate children’s behavioral health needs. The content was developed by a panel of clinical childhood behavioral health experts. Read More
Oregon
Oregon Medicaid Members Are Concerned About Access to Mental Health, SUD Services, Report Finds. The Lake County Examiner reported on September 19, 2022, that access to mental health, substance use disorder (SUD), and supporting behavioral health services is a significant challenge for Oregon Medicaid members, according to a report from the Oregon Health Authority’s Ombuds Program. Other concerns include language access and equity-centered approaches, care coordination, and member-centered transitions across services and benefits. Read More
Pennsylvania
Pennsylvania Receives $12 Million for HCBS Through the Money Follows the Person Program. The Pennsylvania Department of Human Services (DHS) announced on September 19, 2022, that the state recieved $12 million in federal funding for the Money Follows the Person (MFP) program, which helps to move individuals from institutional care to home and community-based services (HCBS). DHS has previously used MFP funding for affordable housing, nursing home transition training, programs to support individuals with behavioral health needs, and more. Read More
AbsoluteCare Expands Into Pittsburgh Through Collaboration With Highmark Wholecare. AbsoluteCare announced on September 15, 2022, its expansion into Pittsburgh, PA, through a collaboration with Highmark Wholecare. AbsoluteCare provides primary care services to clinically complex and vulnerable Medicaid and Medicare members. Read More
Tennessee
Tennessee Is Hit With Lawsuit Over Medicaid Managed Care Procurement. Health Payer Specialist reported on September 19, 2022, that Centene subsidiary Rhythm Health Tennessee filed a state lawsuit, alleging that the state’s recent Medicaid managed care procurement process was “unlawful, arbitrary and discriminatory.” Rhythm was the only of four bidders not to be awarded a contract, and its protest of the awards was denied. Read More
Texas
Texas to Receive $165.6 Million in Settlement Over Medicaid Drug Pricing. Kaiser Health News reported on September 19, 2022, that Centene has agreed to pay $165.6 million to resolve claims that it overcharged the Texas Medicaid program for prescription drugs and pharmacy benefit management services. The deal was signed in July, but not publicly announced until September. Texas is the 12th state to settle pharmacy billing claims with Centene. Read More
Utah
Utah Has Nation’s Lowest Rate of Children from Low-Income Families on Public Insurance, Study Finds. Axios Salt Lake City reported on September 19, 2022, that Utah has the nation’s lowest rate of public health insurance among kids from low-income families (less than $53,000 for a family of four), according to an Axios analysis of U.S. census data. Overall, Utah continues to have one of the nation’s highest rates of eligible individuals who are not enrolled in Medicaid, despite implementing Medicaid expansion. Read More
Virginia
Virginia Investigates Potential Fraud in Medicaid Mental Health Crisis Program. InsuranceNewsNet/The Culpeper Star-Exponent reported on September 16, 2022, that Virginia is investigating potential fraud in the state’s Medicaid community stabilization program, which covers individuals experiencing a mental health crisis. A state audit found that providers billed $88.5 million through six Medicaid managed care plans in fiscal 2022, against a budget of $12.5 million. Billings in fiscal 2023 are already $28.9 million, against a budget of $21.2 million. Effective this month, the state is requiring providers to receive prior authorization for the service from managed care plans. The state Medicaid office has also referred the issue to the attorney general’s Medicaid Fraud Control Unit. Read More
National
CMS Releases Guidance on Medicaid Upper Payment Limit Calculations for Nursing Facilities. The Centers for Medicare & Medicaid Services (CMS) released on September 21, 2022, guidance for state Medicaid programs to transition Medicaid upper payment limit calculations for nursing facilities to reflect the Patient-Driven Payment Model that will be adopted for Medicare, effective October 1, 2023. At that time, CMS will no longer support the Medicare Resource Utilization Groups model. Read More
HHS Releases Strategy to Support Family Caregivers With a Focus on Diversity. The U.S. Department of Health and Human Services (HHS) released on September 21, 2022, the 2022 National Strategy to Support Family Caregivers, which focuses on person- and family-centered approaches, trauma, diversity, and the direct care workforce. The strategy includes almost 350 actions the federal government will take to support family caregivers and more than 150 actions that can be adopted at other levels of government and across the private sector. Read More
U.S. Lawmakers Seek Legislation Requiring All States to Permanently Extend Postpartum Medicaid Coverage to 12 Months. The Washington Post reported on September 19, 2022, that U.S. Senator Dick Durbin (D-IL) and U.S. Representative Frank Pallone Jr. (D-NY) are seeking legislation that would require all states to permanently extend postpartum Medicaid coverage to 12 months. There are 15 states that have not yet voluntarily extended postpartum Medicaid coverage to 12 months. In addition, Congress has only authorized coverage extensions for five years through April 1, 2027. Read More
HHS Offers Strategy for Improving Mental Health, Substance Use Care. Fierce Healthcare reported on September 19, 2022, that the U.S. Department of Health and Human Services (HHS) released a roadmap for improving mental health and substance use care, including a focus on integration into larger health systems, financing arrangements that foster parity, expanding access, and addressing workforce shortages. The roadmap also includes an effort to advance behavioral health promotion, upstream prevention, and recovery. Read More
AIDS HealthCare Foundation Wins $23 Million PBM Arbitration Judgement. Health Payer Specialist reported on September 19, 2022, that CVS Health/Caremark lost its appeal of an arbitration judgement awarding $23 million to the AIDS Healthcare Foundation (AHF) over pharmacy benefit management clawbacks on prescriptions filled by AHF pharmacies. CVS Health/Caremark had appealed the arbitration judgement to a federal court. Read More
Medicaid Eligibility Redeterminations Could Take 12 Months Following PHE, State Regulators Say. Fierce Healthcare reported on September 16, 2022, that state Medicaid agencies may require 12 months to complete Medicaid eligibility redeterminations after the end of the federal COVID-19 public health emergency (PHE) ends, according to stakeholders at a Medicaid and CHIP Payment and Access Commission meeting. The Centers for Medicare & Medicaid Services will allow states 14 months to complete all redeterminations. Read More
One-Fourth of Hospitals to Avoid Readmission Penalties. Modern Healthcare reported on September 15, 2022, that one in four hospitals will not face Medicare readmission penalties because this is the first year the Centers for Medicare & Medicaid Services (CMS) is using pandemic-era data for payment adjustments under its Hospital Readmissions Reduction Program. Hospitals that did not meet the standard in recent years can also expect lower reimbursement cuts. Read More
U.S. House Task Force Urges Senate to Pass Mental Health Grants Package. CQ News reported on September 15, 2022, that the U.S. House Bipartisan Addiction and Mental Health Task Force released a 2022 legislative agenda that urges the U.S. Senate to pass a mental health grants package, which has already been passed by the House. The agenda also seeks to ensure that a fiscal 2023 omnibus spending bill includes sufficient funding for mental health treatment and recovery, along with numerous proposed bills on prevention, prescribing, treatment, health care parity, recovery, education and stigma reduction, rural communities, and youth and families. Read More
NCQA, CHCF Release Framework to Measure Health Equity in Medicaid Managed Care. The National Committee for Quality Assurance (NCQA) released on September 15, 2022, a framework that can be used by states to measure health equity in Medicaid managed care programs. The framework, which was developed by NCQA with funding from the California Health Care Foundation (CHCF), consists of the following: social interventions, access to care, structures of care, experience of care, high-quality clinical care, and overall well-being. Read More
U.S. Representative Introduces Legislation to Expand NEMT Access for Dual-Eligibles. MedPage Today reported on September 15, 2022, that U.S. Representative Buddy Carter (R-GA) introduced a bipartisan bill in the House that would allow partial dual-eligible beneficiaries to qualify for non-emergency medical transportation (NEMT) benefits. The Access to Critical Non-Emergency Transportation Services Act would also require the U.S. Department of Health and Human Services to issue guidance on assisting dual-eligibles in accessing partial NEMT benefits. Read More
Study Calls for Increased Access to Naloxone to Treat Opioid Overdoses. Well Being Trust released on September 15, 2022, a study recommending that more naloxone in any form needs to be made available to individuals with opioid use disorder. The study, conducted by Health Management Associates, also recommended additional research on the availability of naloxone, creation of practice standards, and enactment of federal and state policy to drive access. Read More
Medicare Advantage Prior Authorization Bill Passes House. Modern Healthcare reported on September 14, 2022, that Medicare Advantage plans would be required to use electronic prior authorization programs, submit annual lists of services subject to prior authorization, and embrace beneficiary protection standards, according to a bipartisan bill passed by the House. The bill now moves to the Senate, where it is part of a mental health package referred to the Senate Finance Committee. Read More
Proposed Legislation Would Prevent 2023 Medicare Physician Payment Cut. Fierce Healthcare reported on September 14, 2022, that U.S. Representatives Larry Bucshon, MD, (R-IN), and Ami Bera, MD, (D-CA), introduced the Supporting Medicare Providers Act of 2022, which would prevent a 4.5 percent pay cut for Medicare physicians in 2023. Physicians are also urging Congress to continue a five percent bonus for participation in alternative payment models. Read More
11 States Submit 1115 Waivers to Provide Care for Justice-Involved Groups. The Commonwealth Fund reported on September 13, 2022, that Arizona, California, Kentucky, Massachusetts, Montana, New Jersey, New York, Oregon, Utah, Vermont, and Washington have submitted Section 1115 waiver proposals to the Centers for Medicare & Medicaid Services (CMS) to provide Medicaid-covered healthcare services to justice-involved populations before release to support community reentry. The requests vary on eligible populations, scope of services, and duration of coverage. CMS has yet to issue guidance on the parameters of these waivers under legislation enacted in 2018. Read More
Industry News
UnitedHealth Group Is Cleared to Acquire Change Healthcare. Modern Healthcare reported on September 19, 2022, that a federal judge cleared UnitedHealth Group to acquire Change Healthcare. The judge also ordered UnitedHealth Group to divest Change Healthcare’s ClaimsXten business to TPG Capital, which UnitedHealth Group has agreed to do for $2.2 billion. The acquisition, which the U.S. Department of Justice was attempting to block, is set to be completed by December 31. Read More
Humana to Fully Acquire 20 Senior Primary Care Clinics After Buying Out Welsh, Carson’s Stake. Modern Healthcare reported on September 16, 2022, that Humana will own 100 percent of 20 CenterWell Senior Primary Care clinics after acquiring shares owned by private equity firm Welsh, Carson, Anderson & Stowe for $550 million. Humana and Welsh, Carson built the clinics through a joint venture, with Humana holding a minority stake and Welsh, Carson holding a majority. Humana has two joint ventures with Welsh, Carson to build a total of 167 clinics. Humana has the option of acquiring 100 percent of each clinic after five years. Read More
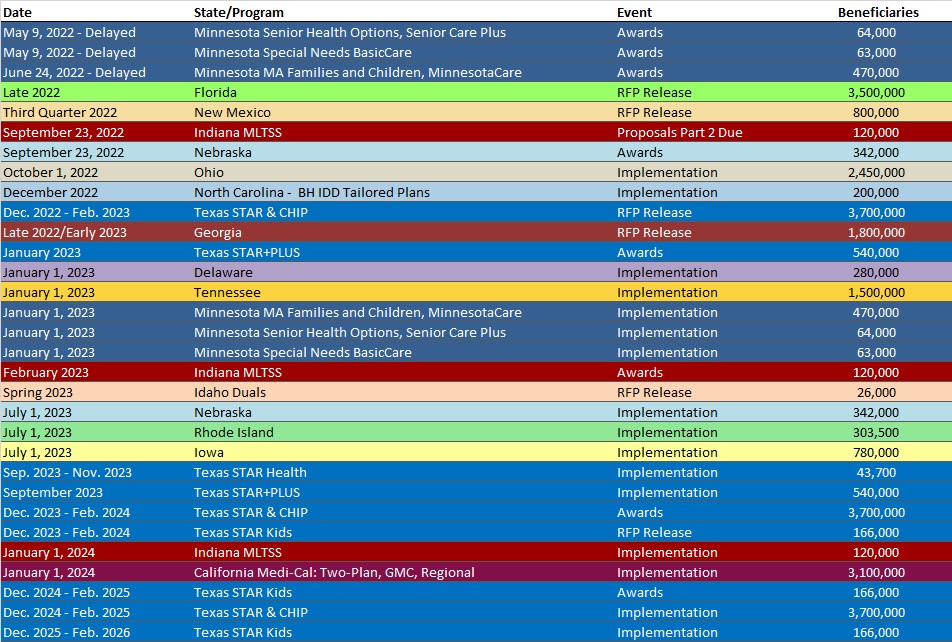
RFP Calendar
HMA News & Events
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Arkansas Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
- Colorado RAE Enrollment is Up 3.4%, May-22 Data
- District of Columbia Medicaid Managed Care Enrollment is Up 3.1%, Jun-22 Data
- District of Columbia Medicaid Managed Care Enrollment is Up 4.5%, Jul-22 Data
- Hawaii Medicaid Managed Care Enrollment is Up 0.9%, Jan-22 Data
- Indiana Medicaid Managed Care Enrollment Is Up 4.2%, Apr-22 Data
- Kentucky Medicaid Managed Care Enrollment is Up 3.3%, Jul-22 Data
- Louisiana Medicaid Managed Care Enrollment is Up 3.2%, Jun-22 Data
- Maryland Medicaid Managed Care Enrollment Is Up 3%, Jun-22 Data
- Nebraska Medicaid Managed Care Enrollment Is Up 5.4%, Jun-22 Data
- New Jersey Medicaid Managed Care Enrollment is Up 3.6%, Jun-22 Data
- North Dakota Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
- Oregon Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
- Texas Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
- Utah Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
- Virginia Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
- Wisconsin Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
- Wyoming Medicaid Enrollment Is Down 2.9%, FY 2021 Data
Medicaid Financials and Utilization Data:
- Sole North Dakota Medicaid MCO’s MLR Is 94.1%, 2021 Data
- Wyoming Medicaid Spending Up 4.2% to $567 Million, FY 2021 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- California Medi-Cal Managed Care Two-Plan, GMC, and Regional Models RFP, Proposals, Evaluation, Awards, and Appeals, Sep-22
- Florida Children with Special Health Needs Managed Care RFI, Responses, and Related Documents, Aug-22
- Florida Statewide Medicaid Managed Care Model Contract, Feb-22
- Nebraska Preventative Health Services and Health Services Block Grant Sub-Award RFA, Sep-22
- New Hampshire Medicaid Care Management Dental Benefit RFI and Responses, Aug-22
- Ohio Medicaid Electronic Visit Verification Services RFP, Sep-22
- Pennsylvania HealthChoices Physical Health RFA, Model Contract, List of Bidders, Awards, and Related Documents, 2019-20
Medicaid Program Reports, Data, and Updates:
- Nevada Medicaid COVID-19 Public Health Emergency Unwinding Plan, Sep-22
- New Mexico Medicaid HITECH Implementation Advance Planning Document, 2020
- New York HHS OIG NEMT Services Audit, Sep-22
- Ohio Medicaid Budget Variance Reports, 2021
- Oregon HITECH Implementation Advance Planning Document, Apr-17
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
