This week's roundup:
- In Focus: HMA Identifies Key Trends for Emerging Medicaid Section 1115 Demonstration Proposals

- California Faces Lawsuit from Health Plan Over Alleged Public Records Act Violation

- Kansas to Hold Public Meetings on KanCare With Beneficiaries, Stakeholders

- Massachusetts to Transition Dual Eligibles from MMP Demo to D-SNP

- Mississippi Submits Amendment to Increase Reimbursement Rates for Private Duty Nurses by 15 Percent

- Oklahoma Gubernatorial Candidates Clash on Medicaid Managed Care Implementation

- Texas Releases STAR, CHIP Draft RFP

- Utah to Transition to New MMIS in 2023

- West Virginia Releases RFP for Foster Children, Youth in Medicaid Managed Care

- Treasury Announces Rules Aimed at Fixing Exchange Plan ‘Family Glitch’

- Walgreens Boots Alliance to Acquire Remaining 45 Percent Stake in CareCentrix

- Cimarron Healthcare Capital, Tacoma Holdings Invest in Frontpoint Health

In Focus
HMA Identifies Key Trends for Emerging Medicaid Section 1115 Demonstration Proposals
This week, our In Focus explores a new trend to watch in Medicaid Section 1115 waiver demonstration programs. As discussed in our previous In Focus, state Medicaid agencies are exploring pathways and concepts to address the historic inequities and health disparities laid bare and exacerbated by the COVID-19 pandemic. These efforts are closely aligned with the Centers for Medicare and Medicaid Services’ (CMS) policy objectives for the Medicaid program, specifically:
- Addressing health inequities
- Improving access and coverage
- Promoting whole person care
Teams of experts from across the HMA family of companies are supporting state agencies, counties, health plans, providers, community and consumer organizations, and other stakeholders with translating federal goals and parameters into concrete proposals for new demonstration programs. HMA’s experts assist stakeholders with proposals as they move through the stages of concept paper, application, negotiation, approval, and implementation. Demonstrations will reflect each state’s unique political and policy landscapes, but the programs will be grounded in certain federal goals and expectations to enhance accountability and improve outcomes.
In the earlier In Focus, our experts shared initial insights and considerations for stakeholders about one of the emerging trends: state Medicaid leaders are seeking to improve health equity in communities by providing health-related social services and engaging community organizations. Building on this and informed by our collective “on the ground” expertise we are writing this week about a second emerging trend we see across states’ Section 1115 activities:
Trend #2: States are seeking to use Medicaid demonstration programs to build essential capacity and infrastructure at the community and organizational levels.
The recently approved and submitted demonstration proposals signal CMS’ willingness to allow states to support some limited capacity building for community-based organizations. Several state 1115 demonstration proposals describe the state-specific types of community-based organizations and other entities that Medicaid programs want to engage to address the social and health-related drivers of health outcomes. This requires augmenting the existing workforce, providing training on Medicaid health plan contracting requirements, and building an infrastructure platform and systems that will support efficient communications and service delivery.
CMS has indicated a strong interest in advancing states’ community-based activities. This is evident in CMS’ decision to revise the federal framework used to determine whether a state’s Section 1115 demonstration program is budget neutral for the federal government. CMS has also decided to reopen the opportunity for states to propose Designated State Health Programs (DSHPs) under more limited size and scope parameters. CMS articulated these updated policies in the recent approval letters for Section 1115 demonstration programs in Massachusetts and Oregon. The federal reinterpretation provides states significantly more flexibility relative to the prior policy to use federal Medicaid funding to do the following:
- Design and implement a broader set of health-related service need (HRSN) initiatives,
- Make investments in the infrastructure to support HRSNs; and
- Invest in building workforce capacity.
States will continue to act on these shifts in federal priorities and policies, crafting proposals aligned with their state-specific environments and goals. However, CMS’ willingness to support capacity building as part of state demonstration programs will need to adhere to certain scope and financing parameters. These guardrails are articulated in more detail in the approval letters for Massachusetts and Oregon. States and stakeholders will also want to be responsive to CMS’ expectations that its investments will be sustainable over time. They may need to plan and develop additional capacity to utilize non-Medicaid sources of federal and non-federal funding in tandem with the demonstration initiatives.
Importantly, the terms of the approved demonstration projects reinforce the need for states, managed care plans, and providers engage in new partnerships with community leaders and ensure the perspectives and experiences of consumers are continuously reflected in programs. Examples of proposed capacity building partnerships include:
Massachusetts’ recently secured CMS approval for a Section 1115 demonstration program which will fund a variety of health-related service needs (HRSN) initiatives. As part of the HRSN initiatives, CMS is allowing the state to receive federal Medicaid funding to support capacity-building, infrastructure, and operational costs for these activities. For example, under the demonstration federal funding will be available for participating “community partners” to pay for health information technology system investments, expand workforce capacity, manage startup costs, and enhance operational infrastructure such as system change resources. Additionally, the state will be able to receive federal Medicaid funding for provider workforce recruitment and retention activities, specifically primary care and behavioral health provider student loan repayment programs and a family nurse practitioner residency program.
In September 2022, Oregon received approval for a Section 1115 demonstration program to provide increased coverage of certain services that address HRSN. These services include critical nutritional services and nutrition education, as well as transitional housing supports for individuals with a clinical need or transitioning out of institutional care, congregate settings, out of homelessness or a homeless shelter, or the child welfare system. Additionally, the state will be able to receive federal Medicaid funding to make infrastructure investments to support those services, such as cultural competency training, trauma-informed training, traditional health worker certification, accounting and billing systems among others.
New York State envisions that Social Determinant of Health Networks (SDHNs) will work to organize and coordinate small neighborhood organizations familiar with their communities’ needs and the capacity to address multiple social risk factors as well as larger county or regionally focused entities. The state aims to allow SDHNs to receive Medicaid funding to invest in developing the infrastructure they need to assist Medicaid enrollees, such as the IT and business processes and other capabilities. Alongside this, the state is proposing a minimum fee schedule for certain services addressing social care needs. In addition, New York is requesting support for a statewide social services referral technology platform.
Washington state has a proposal pending with CMS that builds on its earlier demonstration program to further invest in multi-sector, community-based partnerships and approaches using Accountable Communities of Health (ACH). Specifically, the state is proposing to invest in the development and operation of Community Hubs and a Native Hub, which will serve as centers for community-based care coordination. These hubs will focus on health-related social needs (HRSNs) that provide screening for and referral to community-based services for Medicaid enrollees. These hubs will also distribute funding to build capacity among community-based organizations (CBOs) and community-based providers.
New Jersey has designed an 1115 demonstration proposal focused on the lack of stable housing as a driver of unnecessary hospitalization, institutionalization, or other avoidable instances of high-cost care, negative clinical outcomes, and worsening of chronic conditions. While it does not plan to make direct investments in community-based entities, the state aims to enhance contractual requirements with its Medicaid managed care organizations around housing specialists. This includes requiring health plans to have their housing specialists coordinate with community-based organizations that provide housing services or other related services to address social drivers of health. Its proposal also is designed to facilitate coordination across state and community resources that are essential to the provision of health and housing services.
Conclusion
The Massachusetts and Oregon demonstration programs provide important insight on CMS’ willingness to support state investments in HRSN and the state and local infrastructure to support delivery of culturally appropriate services.
Stakeholders will want to monitor these and other proposals as they move forward, particularly to understand the conditions and timing for funding to flow to community entities. Additionally, each state demonstration will have reporting and accountability structures that could impact payment and future investments made by Medicaid health plans, providers, CBOs and other stakeholders.
HMA’s interdisciplinary teams of Medicaid, human services, and actuarial experts are assisting states as well as stakeholders as they conceptualize, develop, and implement Section 1115 programs. To learn more about our work and connect with an HMA expert in your state please contact Andrea Maresca.
HMA Roundup
Arkansas
Arkansas Recovers $42.5 Million in Medicaid Fraud Cases in Fiscal 2022. Southwest Arkansas Today reported on October 6, 2022, that the Arkansas Medicaid Fraud Control Unit (MFCU) recovered a record amount of more than $42.5 million in civil settlements, restitution, and fines in fiscal 2022. The MFCU also secured 33 convictions and 51 arrests.
California
California Requests Denial of Medi-Cal Managed Care Award Appeals. The California Department of Health Care Services requested on September 30, 2022, that appeals to the state’s recent Medi-Cal managed care awards be denied. Appeals were filed by Blue Shield of California Promise Health Plan, CVS/Aetna, Community Health Group, and Centene/Health Net.
California Faces Lawsuit from Health Plan Over Alleged Public Records Act Violation. Becker’s Healthcare reported on October 7, 2022, that Blue Shield of California filed a lawsuit against the California Department of Health Care Services (DHCS), alleging DHCS violated the state public records act in refusing to release documents on the scoring process, methodology, and communications related to the award of Medi-Cal contracts for 2024. Blue Shield was not awarded Medi-Cal contracts in any of the 13 counties it bid on. Read More
Kansas
Kansas to Hold Public Meetings on KanCare With Beneficiaries, Stakeholders. KZRF reported on October 7, 2022, that the Kansas Department of Health and Environment is holding a series of public meetings to allow KanCare beneficiaries and stakeholders to comment on the program and the Section 1115 waiver. Meetings will be held in-person and virtually throughout October. Read More
Massachusetts
Massachusetts to Transition Dual Eligibles from MMP Demo to D-SNP. The Massachusetts Executive Office of Health and Human Services (EOHHS) submitted to federal regulators on September 30, 2922, a plan to convert the state’s One Care program for dual eligibles from a Medicare‐Medicaid Plan (MMP) demonstration to a Dual Eligible Special Needs Plan (D-SNP) program, effective January 1, 2026. As of September 2022, there were 35,000 individuals enrolled in One Care. Read More
Mississippi
Mississippi Submits Amendment to Increase Reimbursement Rates for Private Duty Nurses by 15 Percent. Mississippi Today reported on October 5, 2022, that the Mississippi Division of Medicaid submitted to federal regulators an emergency amendment to increase reimbursement rates for private duty nurses by 15 percent for the remainder of the public health emergency. If approved, the rates would be retroactive to October 1. Read More
Oklahoma
Oklahoma Gubernatorial Candidates Clash on Medicaid Managed Care Implementation. KGOU reported on October 12, 2022, that the Oklahoma Gubernatorial race is likely to decide the future of Medicaid managed care implementation in the state. Republican incumbent Governor Kevin Stitt supports the program. His Democratic opponent, State Superintendent of Public Instruction Joy Hofmeister, opposes. The state legislature approved managed care in May 2022, with the stipulation that provider-led entities would receive preferential treatment for contract awards. Read More
Tennessee
Tennessee Releases NEMT Technology Solutions RFI. The Tennessee Division of TennCare released on October 10, 2022, a request for information (RFI) on blockchain solutions related to online credentialing, auditing, and complaint management in the state’s Medicaid non-emergency medical transportation (NEMT) benefit. The responses are due November 4. Read More
Texas
Texas Releases STAR, CHIP Draft RFP. The Texas Health and Human Services Commission (HHSC) released on October 6, 2022, a draft request for proposals (RFP) for the state’s STAR and Children’s Health Insurance Program (CHIP) Medicaid managed care program. A final RFP will be issued on December 7, with responses due on February 8, 2023. HHSC will award at least two managed care organizations for each service area. Read More
Texas Senator to Reintroduce Medicaid Expansion Legislation. State of Reform reported on October 5, 2022, that Texas Senator Nathan Johnson (D-Dallas) plans to reintroduce Medicaid expansion legislation during the next legislative session. Johnson, who spoke at the 2022 North Texas State of Reform Health Policy Conference, pointed to the financial and social benefits that Texas would receive from expansion. Read More
Utah
Utah to Transition to New MMIS in 2023. State of Reform reported on October 11, 2022, that the Utah Department of Health and Human Services (DHHS) will begin the transition to a new Medicaid management information system (MMIS) in January 2023, with full implementation expected in April. The new provider reimbursement information system (PRISM) aims to create an online claims database. DHHS is also preparing for the end of the federal public health emergency by developing a communication toolkit, plans to provide 60 days advance notice to members, and developing a dashboard to display Medicaid eligibility metrics. Read More
West Virginia
West Virginia Releases RFP for Foster Children, Youth in Medicaid Managed Care. The West Virginia Department of Administration released on September 30, 2022, a request for proposals (RFP) for Medicaid managed care coverage of children and youth in foster care. The RFP covers statewide physical and behavioral health services. Proposals are due on November 1. The contract is anticipated to run from July 1, 2024, through June 30, 2025, with three one-year options. CVS Health/Aetna is the incumbent.
National
Treasury Announces Rules Aimed at Fixing Exchange Plan ‘Family Glitch’. The Associated Press reported on October 11, 2022, that new rules announced by the Treasury Department would attempt to fix the “family glitch,” in which a family’s eligibility for Affordable Care Act (ACA) tax credits are based on the cost of an individual’s work-sponsored health insurance plan instead of the cost of the plan for the whole family. About one million Americans would be impacted by the new rules. Open enrollment begins on November 1. Read More
D-SNPs Are Twice as Likely to Offer SDoH Benefits than Other Medicare Plans, Study Finds. Health Payer Intelligence reported on October 10, 2022, that Medicare Advantage (MA) dual-eligible special needs plans (D-SNPs) were more than twice as likely to offer social determinants of health (SDOH) and nonmedical supplemental benefits than general MA plans, according to a study in JAMA Network Open. Almost 31 percent of D-SNPs offered at least one of these benefits, compared to 14.6 percent for general MA plans. Among fully integrated dual eligible SNPs, 42.4 percent offered at least one of these benefits. Transportation services and food assistance were most commonly offered benefits. Read More
51 Percent of Medicare Advantage Plans With Drug Coverage Will Have Star Rating of 4 or Higher in 2023. Fierce Healthcare reported on October 6, 2022, that 51 percent of Medicare Advantage (MA) plans with drug coverage will have a star rating of four or more in 2023, according to the Centers for Medicare & Medicaid Services (CMS). That is down from 68 percent in 2022. One reason for the decrease is that for 2023, CMS is removing a COVID-19 disaster provision. Open enrollment for Medicare begins on October 15. Read More
Industry News
Walgreens Boots Alliance to Acquire Remaining 45 Percent Stake in CareCentrix. Modern Healthcare reported on October 11, 2022, that Walgreens Boots Alliance announced plans to acquire the remaining 45 percent stake in CareCentrix for $392 million. Walgreens acquired a 55 percent share in the company in August for $330 million. The transaction is expected to close by March 2023. Read More
Bright Health to Trim Medicare Advantage Offerings, Exit Exchange Market. Fierce Healthcare reported on October 11, 2022, that Bright Health will exit the Exchange market and trim its Medicare Advantage footprint to California and Florida in 2023. Bright reported a $1.2 billion net loss in 2021. Read More
LCMC Health Agrees to Buy 3 HCA Healthcare Hospitals in Louisiana.
Modern Healthcare reported on October 10, 2022, that LCMC Health, in partnership with Tulane University, has agreed to buy three Louisiana hospitals from Tennessee-based HCA Healthcare for $150 million. The deal, which includes Tulane Medical Center, Tulane Lakeside Hospital and Lakeview Regional Medical Center, is expected to close in late 2022 or early 2023. Read More
Medicare Plan Is Unable to Expand Footprint in 9 Markets in 2024, Analysis Finds. Modern Healthcare reported on October 10, 2022, that Centene will be unable to expand its footprint in nine of its 108 Medicare Advantage (MA) contracts in Ohio, North Carolina, Arizona, Connecticut and Nevada in 2024 because of low Star ratings, according to an analysis by HealthMine. The nine plans cover 84,000 members or five percent of Centene’s total for MA plans with Part D coverage. Read More
BayMark Health Services Acquires Fritz Clinic. BayMark Health Services/Applegate Recovery announced on October 6, 2022, the acquisition of Fritz Clinic, a group of six office-based opioid treatment (OBOT) programs throughout Alabama. The clinics will operate under the Applegate Recovery brand, which consists of 70 OBOT clinics across 19 states. Read More
Council Capital, Health Enterprise Partners Invest in Alivia Analytics. Council Capital and Health Enterprise Partners announced on October 6, 2022, an investment in Alivia Analytics, which provides technology aimed at ensuring accurate healthcare payments and reducing Medicaid fraud, waste, and abuse. Clients include state Medicaid agencies. Read More
Cimarron Healthcare Capital, Tacoma Holdings Invest in Frontpoint Health. Cimarron Healthcare Capital and Tacoma Holdings announced on October 5, 2022, the recapitalization of Frontpoint Health, a home health and hospice platform serving Medicare Advantage beneficiaries. Brent Korte, former executive of Evergreen Health, will serve as chief executive of Frontpoint. Read More
Avita Acquires AbsoluteCare Atlanta.Avita announced on October 5, 2022, the acquisition of AbsoluteCare Atlanta, which provides integrated care and pharmacy services with a focus on LGBTQ+, HIV, PrEP, gender-affirming, and sexual wellness care. AbsoluteCare Atlanta serves over 5,500 individuals. Read More
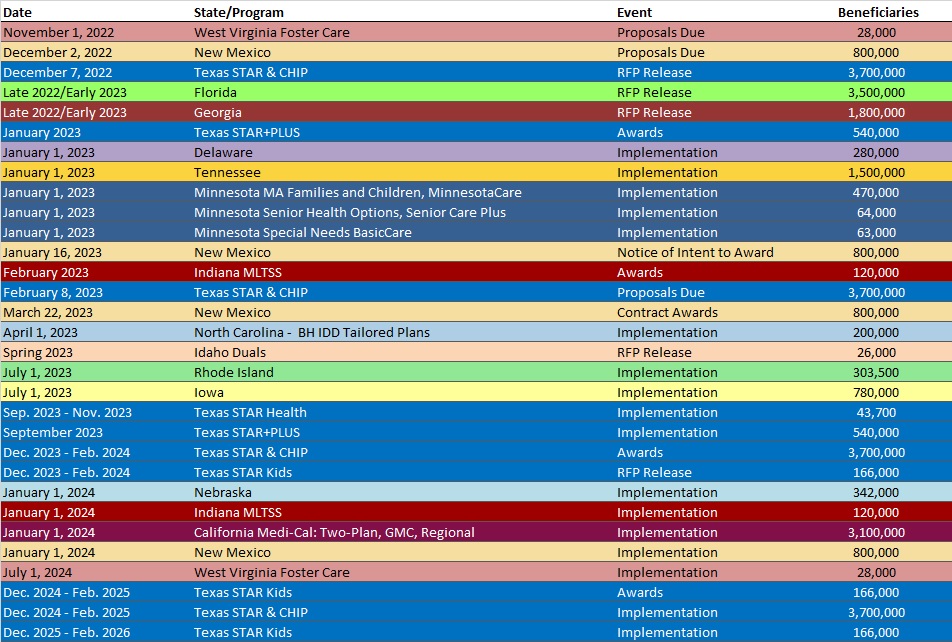
RFP Calendar
HMA News & Events
WAKELY, AN HMA COMPANY, WHITE PAPERS
Wakely Risk Insight for the Medicare Shared Savings Program: Performance Year 2021 Results. Since its inception, the Medicare Shared Savings Program has been committed to achieving the triple aim of healthcare: better care for individuals, better health for populations, and lowering the growth of expenditures. Read More
Summary of 2023 Medicare Advantage and Part D Star Ratings. On October 6, 2022, CMS published the 2023 Medicare Advantage (MA) and Part D Star Ratings. The latest results indicate a drastic decrease in average Star Ratings, mainly attributed to the removal of COVID-19 protections CMS put in place for the 2022 Star Ratings. This brief discusses the overall changes seen in the 2023 Star Ratings and dives further into some of the drivers behind the significant decline in ratings. Read More
Proposed Benchmarking Updates to the Medicare Shared Savings Program. On July 7, 2022, the Center for Medicare and Medicaid Services (CMS) released the 2023 Medicare Physician Fee Schedule Proposed Rule which contained some of the larger proposed updates to the Medicare Shared Savings Program (MSSP) in the history of the program. While not yet final, many of these proposed changes have been received favorably by the industry, providing an early indication that several of the updates may become final. With the final rule set to come out later this year, this white paper contains a deep dive, including detailed examples, of the proposed updates to the MSSP benchmarking and risk adjustment methodologies set forth in CMS’s proposal. We encourage both current MSSP ACOs as well as those thinking about entering or re-entering the program to review this paper as they assess the potential implications for their organization. Read More
HMA WELCOMES
Anna Edwards, Principal – Los Angeles, CA
Anna Edwards is a seasoned clinician and healthcare leader. Her nursing career spans nearly 30 years, with the past 20 years focused on the managed care setting.
Her passion is serving vulnerable populations and inspiring innovative care teams to address complex medical, social, and functional issues facing vulnerable populations and the community. She values continuous learning opportunities, participating in synergistic collaboration opportunities to improve the health and well-being of the community, and advancing the nursing profession in healthcare.
Anna developed and implemented a disease management program based on the Chronic Care Model for a large federally qualified healthcare organization in Los Angeles, CA. In the role of nurse practitioner, she administered a diabetes group visit program which included health educators and community health workers which demonstrated improved clinical outcomes and revenue generation.
Previously Anna served as director of care management for LA Care Health Plan where she was responsible for complex care management and care coordination programs for Medi-Cal and dual eligible populations of all ages. In this role she successfully transitioned a vendor complex case management program to an in-house program (which passed the first NCQA audit), transitioned the D-SNP program to Cal MediConnect (dual demonstration program), and implemented the Covered CA care management program.
She also served as clinical director of behavioral health and care management at Inland Empire Health Plan. In this role, she successfully led her department through audits, developed an integrated care team (physical, behavioral, pharmacy), implemented an in-house Health Risk Assessment (HRA) process, developed and implemented a food insecurity program with a closed loop referral process, and implemented several successful disease management programs for the dual eligible population.
Anna’s prior experience includes providing training, clinical and operational support for Los Angeles County’s Department of Health Services Ambulatory Clinics.
She received her Bachelor of Science degree in nursing from Azusa Pacific University, Master of Science in nursing from California State University (nurse practitioner), and her Doctor of Nursing Practice from Rush University.
Katherine A. Peters, Principal – New York, NY
Katherine Peters is a versatile healthcare leader with a track record of delivering business strategies that drive growth, operational efficiency, and improved member experience. Her ability to form collaborative relationships with staff at all levels and work successfully with cross-functional teams has fueled high quality development of internal systems and processes as well as financial performance.
Her extensive Medicare expertise includes Medicare Advantage, Special Needs Plans, Part D/Prescription Drug Plan (PDP), and Medicare-Medicaid plans. She also has experience with Medicare Supplement Plans, ancillary benefits, model of care and product start-up.
Prior to joining HMA, Katherine was senior director of Medicare Product at the Centene Corporation. In this role she mobilized an enterprise strategy for 2021 Dual Special Needs Plan (DSNP) integration requirements and led the integration of multiple acquisitions across PDP and Medicare Advantage Prescription Drug contracting lines of business. Her leadership drove innovation for supplemental benefits, value-based insurance design, and Center for Medicare & Medicaid Innovation (CMMI) demonstration participation to prompt sales, improve quality, and provide medical savings and operational efficiency.
Katherine previously served as Medicare Product Development Director for a subsidiary of EmblemHealth. She was responsible for the launch of a DSNP and Medicare Supplement plans from concept to implementation. She also worked as DSNP program manager for UnitedHealth Group. In this role she reported to the chief operating officer of the New Jersey Health Plan. Katherine was responsible for the financial, quality, and operational performance of a Fully Integrated Dual Eligible Special Needs Plan, coordinating Medicare and Medicaid programs to become a seamless product experience for members and providers.
Katherine earned her Bachelor of Science in Finance from Villanova University. She received her Project Management Professional (PMP) certification from the Project Management Institute.
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Ohio Dual Demo Enrollment is Down 2.8%, Mar-22 Data
- Pennsylvania Medicaid Managed Care Enrollment is Up 4%, Jul-22 Data
- Rhode Island Dual Demo Enrollment is Down 0.9%, Mar-22 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- California Medi-Cal Managed Care Two-Plan, GMC, and Regional Models RFP, Proposals, Evaluation, Awards, Appeals and Responses, Oct-22
- California T-MSIS Standard Operating Procedures Testing Services RFO, Sep-22
- Minnesota AFMN Technical Assistance Provider Grant Opportunities, Oct-22
- Rhode Island PHE Medicaid Renewals Campaign RFP, Oct-22
- Tennessee Medicaid NEMT Credentialing, Auditing, Complaint Management Solutions RFI, Oct-22
- Texas Medicaid and CHIP Managed Care Services RFP Responses, 2011
- Texas STAR, CHIP Managed Care Draft RFP, Oct-22
- West Virginia Medicaid Specialized Managed Care for Children, Youth RFP, Sep-22
- Wisconsin Family Care MLTC RFP, Responses, and Evaluation, Mar-22
Medicaid Program Reports, Data, and Updates:
- Alabama CHIP Annual Reports to CMS, 2017-21
- California Medi-Cal Managed Care Quality Strategy Reports, 2013-22
- Colorado CHIP Annual Reports to CMS, 2017-21
- District of Columbia Medicaid HITECH Implementation Advance Planning Documents, 2017-21
- Florida CHIP Annual Reports to CMS, 2017-21
- Massachusetts Initial Transition Plan for One Care, Sep-22
- Nebraska Medicaid HITECH Implementation Advance Planning Document, 2014-2022
- New York Medicaid Pharmacy Managed Care to FFS Transition Presentations, Sep-22
- Pennsylvania MLTSS Subcommittee Meeting Materials, 2021-22
- Texas Dually Eligible Individuals Enrolled in Medicaid Managed Care Reports, 2022
- Vermont Medicaid and Exchange Advisory Board Meeting Materials, Jul-22
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.