Colorado
Colorado Releases Medicaid, CHIP Enrollment Broker Services RFP. The Colorado Department of Health Care Policy and Financing released on September 28, 2022, a request for proposals (RFP) for an enrollment broker to serve the state’s Medicaid and Children’s Health Insurance Program (CHIP). The contract begins on June 30, 2023, after a six-month startup period, and runs for one-year with up to five annual renewal options. The current incumbent is Maximus Health Services. Read More
Louisiana
Louisiana to Begin Auto Assignment of Medicaid Beneficiaries into Managed Care Plans. The Louisiana Department of Health announced on September 30, 2022, that it will begin the auto-assignment of Medicaid beneficiaries into one of six Medicaid managed care plans awarded contracts in a recent procurement, with notifications going out to members in November. Five of the plans are incumbents. Enrollees can change their auto-assignment between November 8 and December 29, with the change effective when the new contracts begin on January 1, 2023. After that, changes can still be made up until March 31, 2023. Read More
Maine
Maine Looks to Renew NEMT Waiver, Release RFP. The Maine Department of Health and Human Services announced on October 4, 2022, its intent to release a request for proposals (RFP) for its Medicaid non-emergency medical transportation (NEMT) broker service. News of the RFP was included in an amendment submitted to federal regulators to renew the state’s NEMT waiver for five years. Proposed changes include use of a single capitated rate per region instead of allowing bidders to select from a range of rates as well as revising performance measures. The public comment period is open until November 4. Read More
Massachusetts
Massachusetts to Receive $14 Million in PBM Settlement. Massachusetts announced on September 29, 2022, that it will receive $14.2 million in a settlement concerning Medicaid pharmacy benefit management (PBM) overcharges. The case involved claims that Centene’s PBM operation had overcharged MassHealth for prescription drugs and services. Read More
Minnesota
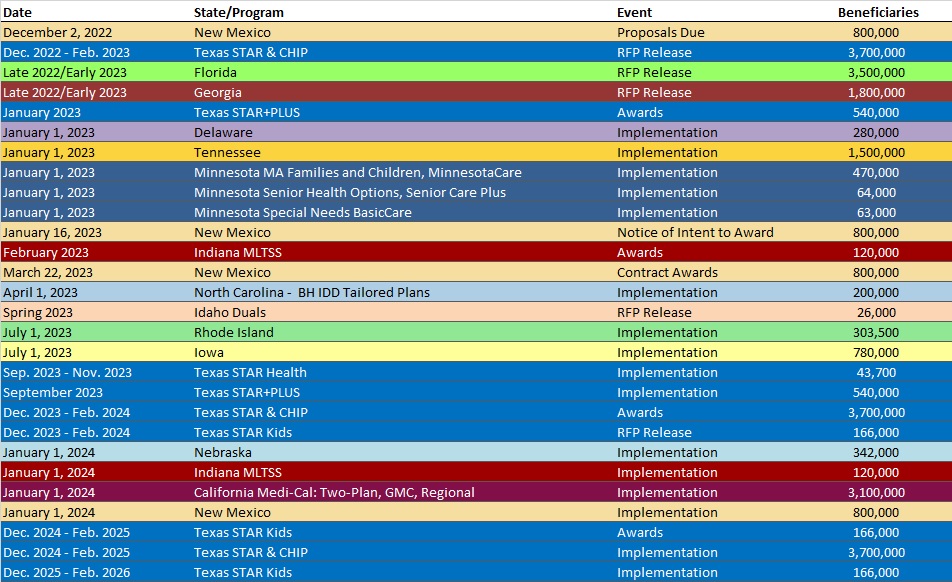
Minnesota Awards Medicaid Managed Care Contracts Covering Individuals Outside Twin Cities, Elderly, Disabled. The Minnesota Department of Human Services awarded on October 5, 2022, Medicaid managed care contracts covering more than 600,000 individuals effective January 1, 2023, including families and children outside the Twin Cities area and both the elderly and individuals with disabilities statewide. Plans awarded in the 80-county area for the state’s Families and Children Medical Assistance (MA) and MinnesotaCare Basic Health and for the Minnesota Senior Health Options (MSHO)/Minnesota Senior Care Plus (MSC+) programs were Blue Plus, HealthPartners, Itasca Medical Care, Medica, PrimeWest Health, South Country Health Alliance, UCare, and United Healthcare Community Plan of Minnesota. Plans awarded for the Special Needs BasicCare (SNBC) program were HealthPartners, Hennepin Health, Medica, PrimeWest Health, South Country Health Alliance, UCare, and United Healthcare Community Plan of Minnesota. Implementation is set for January 1, 2023. Read More
Nebraska
Nebraska Seeks Funds to Cover Aduhelm, Reduce Waiting List for Individuals With Development Disabilities. KPVI/ The Omaha World-Herald reported on October 2, 2022, that the Nebraska Department of Health and Human Services projects the state will need $16 million annually to cover the costs of Alzheimer’s drug Aduhelm for Medicaid beneficiaries. In a biennial budget request to the Governor, DHHS also requested $11.9 million to serve 250 wait listed individuals with developmental disabilities. Overall, DHHS is seeking $2.5 billion annually for the state Medicaid program.
Nevada
Nevada to Begin Medicaid Redeterminations Month After PHE Is Lifted. The Nevada Department of Health and Human Services announced on September 26, 2022, that it will begin conducting Medicaid eligibility redeterminations the month after the public health emergency (PHE) is lifted. Managed care organizations and dental benefits administrators can use text messages to engage members as long as they have opted into text.
New Jersey
New Jersey Senate Committee Advances Bill to Require Medicaid Coverage of Behavioral Health Services Provided in Schools. The New Jersey Senate Democrats announced on September 29, 2022, that legislation requiring Medicaid to reimburse providers for behavioral health services provided to eligible students in schools was unanimously passed by the Senate Education Committee. Previously, federal policy prohibited Medicaid reimbursement of certain school health services. Read More
New York
New York Medicaid Fraud, Waste Reduction Efforts Yield Results. Spectrum News reported on October 3, 2022, that the New York Medicaid program’s efforts to prevent waste and fraud resulted in nearly $3.2 billion recoveries and savings in 2021, according to acting state Medicaid inspector general Frank Walsh. Unnecessary cost avoidance accounted for $2.4 billion of the total, while provider audits and investigations accounted for $714 million. Read More
Molina Healthcare Completes Acquisition of AgeWell. Molina Healthcare announced on October 3, 2022, that is had completed the acquisition of AgeWell New York’s Medicaid managed long term care business. As of September 2022, AgeWell New York’s MLTC business served about 13,000 members. Read More
North Carolina
North Carolina Delays Implementation of Behavioral Health IDD Tailored Plans to April 2023. The North Carolina Department of Health and Human Services announced on September 29, 2022, that it has further delayed the implementation of Behavioral Health and Intellectual/Developmental Disabilities (IDD) Tailored Plans until April 1, 2023. Implementation was originally scheduled for July 2022 and then delayed to December 1, 2022. Tailored plans will be offered by the state’s Local Management Entity-Managed Care Organizations (LME-MCOs). Certain features of the tailored plans, including integrated care management and certain home and community-based services, will be effective in December. Read More
North Dakota
North Dakota Leads Country in Rate of Physicians Accepting New Medicaid Patients, Analysis Finds. The State Health Access Data Assistance Center reported on August 25, 2022, that North Dakota had the highest rate of physicians who accepted new Medicaid patients at 98.8 percent between 2014 and 2017, according to an analysis of health records survey data. New Jersey had the lowest at 42.2 percent. Read More
Ohio
Ohio Governor Looks to Expand Medicaid Eligibility for Pregnant Women to 300 Percent of Poverty. Ohio Governor Mike DeWine announced on September 30 2022, hopes to work with the state legislature to expand the Medicaid income-eligibility limit for pregnant women from 200 percent of poverty to 300 percent as part of a maternal and child health care initiative. DeWine also plans to expand Medicaid eligibility to children adopted through private agencies, as well as launch quality standards to improve birth outcomes at hospitals and birthing centers.
Oklahoma
Oklahoma Implements 25 Percent Rate Increase for Developmental Disability, HCBS Providers. The Oklahoman reported on October 4, 2022, that the Oklahoma Department of Health and Human Services has implemented a 25 percent rate increase for Medicaid providers serving individuals with intellectual and developmental disabilities and home and community-based services (HCBS) providers for seniors. The change, which is aimed at eliminating the state’s 13-year waiting list for developmental disability services, raises hourly wages to $12. More than 4,600 individuals with developmental disabilities are on the waiting list. Read More
Oklahoma to Cover Hospice Services for Medicaid Expansion Adults. The Oklahoma Health Care Authority announced on September 29, 2022, that Medicaid will cover hospice services for adults in the expansion population residing in long-term care facilities, effective October 1. Under the new policy, if Medicare is the primary insurer, the state Medicaid agency will only reimburse hospice providers for coinsurance and deductibles. Read More
National
HCSC Names Anne Rote President of Medicaid Division. Becker’s Payer Issues reported on October 4, 2022, that Health Care Service Corp. (HCSC) named Anne Rote president of its Medicaid division. HCSC is the parent company of Blue Cross Blue Shield of Texas, Illinois, New Mexico and Montana. Rote previously served stints at Molina Healthcare, United/Optum, and Aetna. Read More
Medicare Advantage Plans Are Criticized for Ending Nursing Home Coverage. Kaiser Health News reported on October 4, 2022, that Medicare Advantage (MA) plans are ending members’ coverage for nursing home and rehabilitation services before they are healthy enough to go home, according to health care providers and nursing home representatives. MA must cover the same benefits as Medicare but have leeway when deciding how much nursing home care is necessary. Read More
Less Than 6 Percent of Wealthy Individuals Enroll in Medicaid LTSS, Study Says. Forbes reported on October 4, 2022, that fewer than six percent of high-income individuals over age 65 enroll in Medicaid long-term services and supports (LTSS), according to a paper from Rich Johnson at the Urban Institute. The study also estimated that more than one-third of the lowest income individuals over age 65 use Medicaid LTSS. Read More
CMS Implements ACE Kids Act for Children with Complex Medical Needs. Senator Chuck Grassley (R-IA) announced on October 3, 2022, that the Centers for Medicare & Medicaid Services (CMS) implemented the Advancing Care for Exceptional (ACE) Kids Act, which is aimed at improving specialized care coordination for children with complex medical conditions. The bill was passed in April 2019 and had an implementation deadline of October 1, 2022. Read More
Federal Grants Topping $346 Million Awarded to Address Healthcare Staffing Shortages. Modern Healthcare reported on October 3, 2022, that the U.S. Health and Human Services (HHS) and Labor departments are awarding more than $346 million in grants to help address the health care workforce shortage by training nurses, community workers, and public health professionals. HHS plans to award $225.5 million to 83 recipients through the Community Health Worker Training Program and $40.7 million to 29 recipients through the Public Health Scholarship Program. The Labor Department is awarding $80 million to support programs that expand the pipeline of trained nurses with an emphasis on those from historically marginalized and underrepresented communities. Read More
Center for Medicare & Medicaid Innovation Is Developing Reimbursement Model for Palliative Care. Hospice News reported on October 3, 2022, that the Center for Medicare & Medicaid Innovation (CMMI) is developing a reimbursement model for palliative care. The model will include aspects of CMMI’s Medicare Care Choices Model demonstration, which ended in December 2021 and performed well on cost savings and patient satisfaction. Read More
Biden Is Expected to Sign Bill Extending Rural Hospital Payment Programs. Fierce Healthcare reported on September 30, 2022, that President Biden is expected to sign a short-term budget bill passed by Congress, which would extend two rural hospital programs through December 16 – the hospital payment adjustment for certain low-volume hospitals and the Medicare-Dependent Hospital program. The short-term bill also gives provider groups a window to head off a four percent mandatory cut under the PAYGO law and a 4.5 percent cut to Medicare payments.
Read More
5 Percent of Children Were Uninsured From 2016-20, Report Finds. Health Payer Intelligence reported on September 30, 2022, that five percent of children aged 17 and younger were uninsured between 2016 and 2020, according to a report from the State Health Access Data Assistance Center, funded by the Robert Wood Johnson Foundation. Among racial and ethnic groups, the uninsured rate was highest for American Indian and Alaska Native children at 14.1 percent. Data is for 50 states and the District of Columbia from U.S. Census Bureau estimates. Read More
CMS Offers States Grants to Develop Health Homes for Children With Complex Conditions. The Centers for Medicare & Medicaid Services (CMS) announced on September 30, 2022, that it will award grants to states for activities related to the development of health homes aimed at improving care coordination for children with medically complex conditions. The initiative would allow states to expand coverage of coordination of care, including efforts by out-of-state providers. Read More
CMS Projects Medicare Advantage Premiums to Fall Nearly 8 Percent in 2023. The Centers for Medicare & Medicaid Services (CMS) announced on September 29, 2022, that the projected average monthly premium for 2023 Medicare Advantage Plans will be $18, down eight percent from $19.52 in 2022. The average basic monthly premium for standard Part D coverage is projected to decrease nearly two percent from $32.08 to $31.50. Read More
Federal Judge Rules HHS Must Restore Full 340B Drug Payments for Remainder of 2022. Modern Healthcare reported on September 29, 2022, that the U.S. Department of Health and Human Services (HHS) must restore full 340B drug payments for the remainder of 2022, according to a federal judge’s ruling. The ruling follows a Supreme Court order from June that HHS must compensate providers for lower 340B payments received in prior years. Read More
Medicaid, Medicare Enrollment Exceeds 142 Million in June 2022, CMS Reports. The Centers for Medicare & Medicaid Services announced on September 29, 2022, that Medicaid and Children’s Health Insurance Program (CHIP) enrollment exceeded 89 million in June 2022, an increase of 0.5 percent since May 2022. Medicare enrollment was nearly 65 million, an increase of 0.2 percent. More than 12 million individuals were eligible for both Medicare and Medicaid. Read More
Tricare PBM to Drop Nearly 15,000 Pharmacies From Network. Health Payer Specialist reported on September 28, 2022, that pharmacy benefit manager Cigna/Express Scripts will drop nearly 15,000 pharmacies from the U.S. Defense Department’s Tricare network effective next month. The Tricare PBM contract, which was awarded to Cigna/Express Scripts last year, runs 15 months with seven one-year renewal options. Tricare is expected to announce awards for its medical care plans in November. Read More
Medicaid NEMT Fraud Investigations Result in Convictions, Settlements. The U.S. Government Accountability Office (GAO) announced on September 28, 2022, that state Medicaid fraud investigations resulted in nearly 200 criminal convictions, civil settlements, and judgments against non-emergency medical transportation providers (NEMT) from 2015 through 2020, according to a GAO report. The fraud included NEMT providers billing for trips that were not provided or using unauthorized drivers or vehicles. The report also found that most states utilize a combination of managed care, third party brokers, and in-house approaches to administer NEMT benefits. Read More
Medicare Telehealth Usage Increased 10-Fold During Pandemic, GAO Reports. The U.S. Government Accountability Office (GAO) reported on September 26, 2022, that the use of Medicare telehealth services increased from 5 million between April and December 2019 to 53 million between April and December 2020. Overall Medicare usage was down over the same period. GAO recommends additional oversight and education for beneficiaries on privacy and security risks. Read More