This week our In Focus section reviews the Louisiana Medicaid managed care request for proposals (RFP) released on June 23, 2021, by the Louisiana Department of Health. Louisiana is seeking full-risk health plans to serve approximately 1.6 million Medicaid beneficiaries. Contracts are worth approximately $9 billion annually.
Previous procurement awards from 2019 to incumbents AmeriHealth Caritas, Healthy Blue/Anthem, and UnitedHealthcare, and new entrant Humana, were rescinded. The state executed emergency contracts with the five current MCOs following protests from two incumbents who were not awarded contracts.
Louisiana implemented its Medicaid managed care program in 2012 and expanded Medicaid under the Affordable Care Act in 2016. Medicaid managed care organizations (MCOs) will provide physical health and behavioral health services to beneficiaries.
Services such as dental, long-term care, and home and community-based services are not carved into the contracts. Dental benefits began to be provided in 2018 through a Prepaid Ambulatory Health Plan (PAHP). In light of a national focus on Pharmacy Benefit Manager (PBM) regulation, MCOs will also be asked to address issues related to pharmacy benefits, “particularly advancing the efficiency and economy of the pharmacy program by moving to a single PBM for the entire Louisiana Medicaid Managed Care Program.”
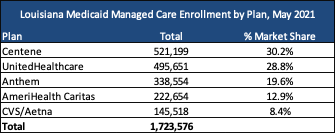
Current Market
Incumbents AmeriHealth Caritas, Anthem/Healthy Blue, Centene/LA Healthcare Connections, CVS Health/Aetna, and UnitedHealthcare served 1.7 million beneficiaries as of May 2021.
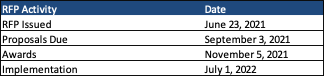
Timeline
Proposals are due September 3, 2021, with awards expected November 5, 2021. Contracts will be implemented July 1, 2022, and run for three years with an option to extend up to two more years.
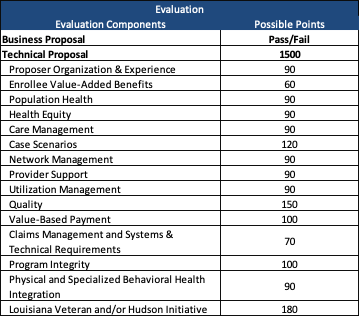
Evaluation
Plans with a minimum of seven years of experience covering health care services for a Medicaid managed care program and serving a Medicaid population of 1.5 million enrollees or greater are desired. Technical proposals will be scored out of 1,500 points. Twelve percent of the total points are reserved for MCOs that are certified small entrepreneurships, or subcontract with one or more small entrepreneurships, through the Veteran‐Owned and Service‐Connected Disabled Veteran‐Owned Small Entrepreneurships (Veteran Initiative) and Louisiana Initiative for Small Entrepreneurships (Hudson Initiative).