This week, our In Focus section reviews the Minnesota Integrated Health Partnerships (IHP) Program request for proposals (RFP) released by the Minnesota Department of Human Services (DHS), Health Care Administration on July 6, 2021. Minnesota will contract with provider organizations to serve as IHPs and provide health care services to Medical Assistance and MinnesotaCare enrollees under alternative payment arrangements.
Background
IHP, formerly called the Health Care Delivery Systems (HCDS) demonstration, first launched in 2013 as a way to test alternative health care delivery systems, including Accountable Care Organizations (ACOs) and value-based payment arrangements for the state’s Medicaid program. It was designed to reduce total cost of care while maintaining or improving quality of care. Providers offer care to Medicaid enrollees in both fee-for-service (FFS) and managed care under a payment model that holds these organizations accountable. In 2018, the state expanded and enhanced this model by introducing multiple tracks to accommodate a diverse set of provider systems, added a quarterly population-based payment to support care coordination and infrastructure needs, and modified the quality measurement methodology. Currently, IHPs provide care to over 427,000 individuals.
RFP Overview
Under the new RFP, the state will further expand the IHP statewide and across different models of care delivery that will integrate health care with substance use and mental health services, safety net providers, and social service agencies. IHPs will not administer benefits or pay claims under the demonstration or be required to contract for additional services outside of the services delivered by the IHP.
IHPs can participate in one of two tracks described in the table below. All IHPs will be eligible for a quarterly population-based payment (PBP) for care coordination that corresponds with the ability to manage an individual’s total cost of care. The PBP encourages accountability for the total cost of care of attributed patients, resource utilization, and quality of health care services provided. The PBP will take the place of any current Health Care Home (HCH) or in-reach service coordination (IRSC) payments being received by the IHP for an IHP attributed member.
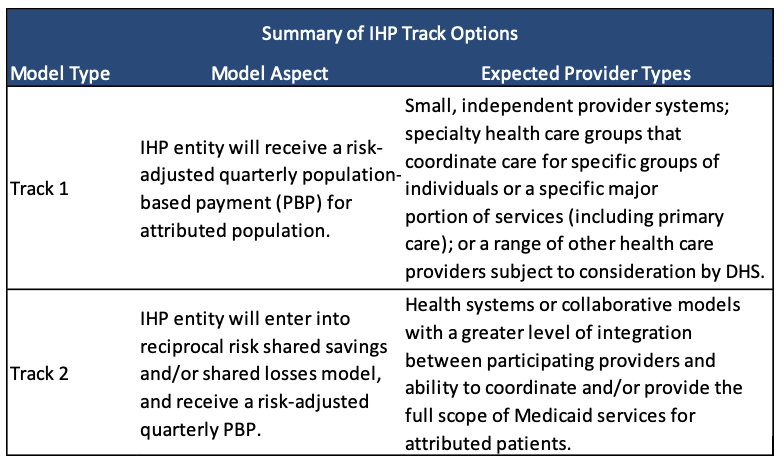
Track 2 IHPs will also be eligible to receive a portion of the shared savings or will be required to pay the state a portion of the shared losses as a result of yearly performance against a total cost of care target. While Track 1 IHPs are not subject to shared losses or shared savings, total cost of care is calculated for Track 1 IHPs in order to provide illustrative performance results.
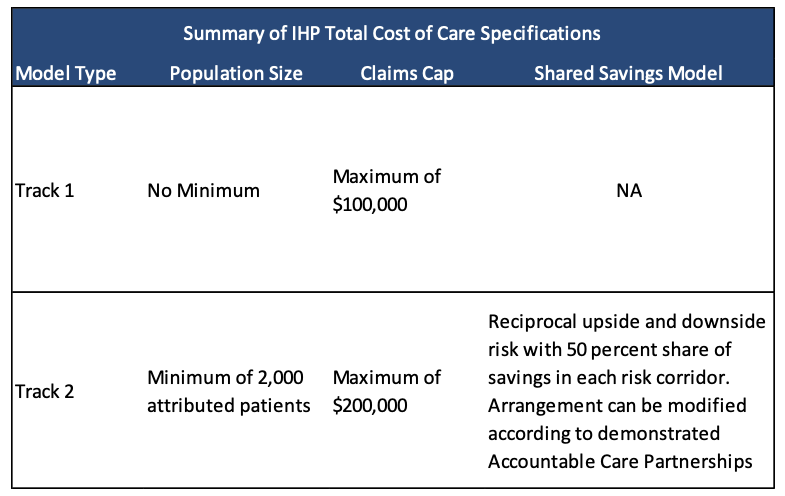
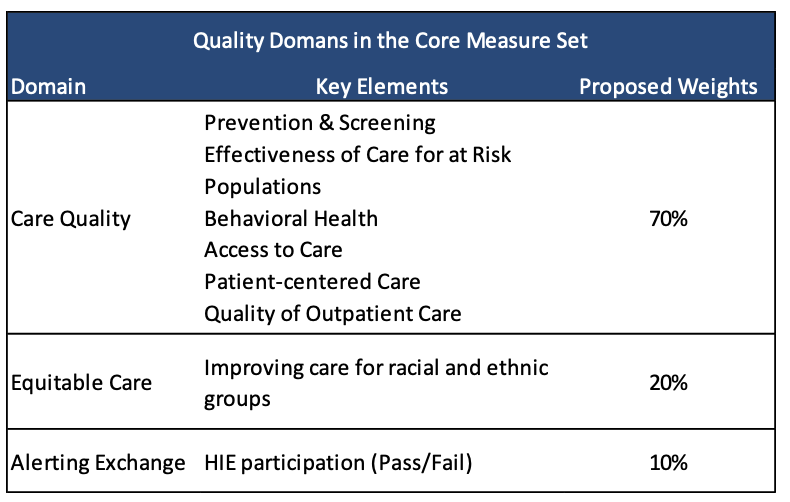
In Track 2, 50 percent of an IHP’s shared savings will be contingent on overall quality measurement results. DHS will calculate this based on three domains: care quality, equitable care, and encounter alert system measures.
Track 1 IHPs are eligible to additionally participate as an Accountable Care Partner with a Track 2 IHP. The parameters are flexible but could include greater potential savings than potential losses. Eligibility for the Accountable Care Partnership risk arrangement depends on the substantiveness of the community partnership, the amount of risk involved for the IHP and the community partner, and the financial impact of the community partnership on the total cost of care. Examples of areas in which IHPs can pursue community partnerships include but are not limited to housing, food security, social services, education, and transportation.
Managed Care Organizations (MCOs) will participate as a payer in the IHP payment pursuant to their contract with the state. The MCO contract has been modified to require cooperation with the IHPs. MHCP beneficiaries will be attributed to an IHP regardless of whether they are enrolled in fee-for-service or in an MCO.
Evaluation
Evaluation for the proposals will be conducted in three phases:
a. Phase I – Required Statements Review
b. Phase II – Evaluation of Proposal Requirements
c. Phase III – Selection of the Successful Responders
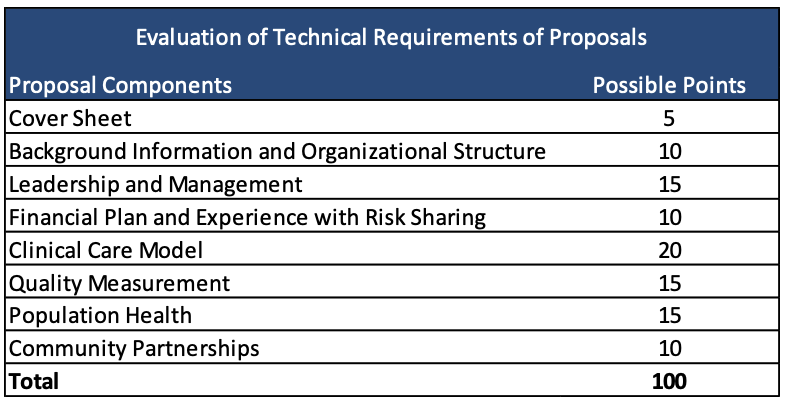
Technical proposals are scored out of 100 points.
Respondents will be required to propose an intervention to address social determinants of health and will be held accountable for agreed upon health equity measures related to the proposed intervention. Proposals must demonstrate how formal and informal partnerships with community-based organizations, social service agencies, counties, public health resources, and others are included in the care delivery model.
Existing IHPs that wish to continue in the IHP Program must clearly indicate previous learnings from health equity interventions, articulate how those learnings are incorporated into the intervention, and whether any changes will be made to expand or enhance the intervention. These responders will need to consider enhancements to existing metrics or propose new metrics that more effectively capture the impact of continued interventions. A responder’s final Population Health Report submission under an existing IHP contract will factor into whether a contract is offered under this RFP.
Respondents must demonstrate they effectively utilize health information technology to coordinate care and engage patients. Respondents must submit documentation with the application to provide evidence of interoperability and meet this requirement.
Additionally, IHPs must promote health and wellness activities, including Minnesota’s Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) Program called Child and Teen Check-ups (C&TC).
Current IHPs
Altair
Allina Health
Avera Health
Bluestone Physician Services
CentraCare Health System
Children’s Health Care
Essentia Health
Face to Face Health and Counseling
Fairview Health Services
Federally Qualified Health Center Urban Health Network (FUHN)
Gillette Children’s Specialty Healthcare
Hennepin Healthcare System (Hennepin County Medical Center Hospital and Clinics)
Integrity Health Network
Lake Region Health Care
Lakewood Health System
Mankato Clinic
Mayo Clinic
MN Association of Community Mental Health Programs (MACMHP)
North Memorial Health Care
Northern Minnesota Network
Northwest Metro Alliance (a partnership between Allina Health and HealthPartners)
Perham Health
Riverwood Healthcare Center
Tri-County Health Care
Wilderness Health
Winona Health Services
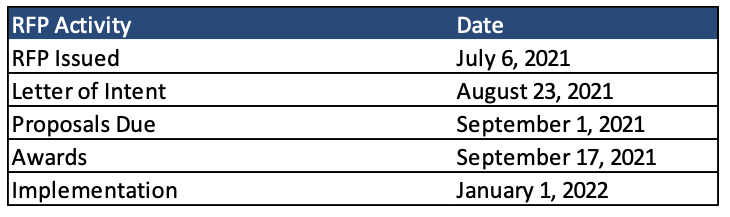
Timeline
Contracts will run for three years, from January 1, 2022, until December 31, 2024, with up to two additional one-year options. Mandatory letters of intent must be submitted by August 23, 2021, and proposals are due September 1, 2021. Awards are anticipated on September 17, 2021.