HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Nebraska Releases Medicaid Managed Care RFP

- California Assembly Committee to Hold Hearing on Bill Allowing No-Bid Medi-Cali Contract

- Connecticut Seeks Medicaid Waiver to Address Coverage Gap

- Illinois Senate Passes Automatic Medicaid Renewal Legislation

- Kansas Lacks Effective System for Tracking HCBS Waiver Redeterminations, Audit Finds

- Mississippi Hires Analytics Firm to Investigate PBMs

- Missouri Senate Committee Advances Measure Aimed at Medicaid Expansion Funding

- Pennsylvania Delays Implementation of Modified Medicaid Managed Care Contracts

- Wisconsin Governor Vetoes Bills Aimed at Tightening Medicaid Eligibility Requirements

- CMS Proposes 3.2 Percent Increase to Fiscal 2023 Inpatient Hospital Payments

- Exchange Plan Premiums Fall 1.8 Percent, Study Finds

- FFL Partners Announces Investment in Perlman Clinic

The next HMA Weekly Roundup will be May 4.
In Focus
Nebraska Releases Medicaid Managed Care RFP
This week, our In Focus section reviews the Nebraska Heritage Health request for proposals (RFP), released by the Nebraska Department of Health and Human Services (DHHS) on April 15, 2022. DHHS will award statewide contracts to two or three Medicaid managed care organizations (MCOs) to serve approximately 342,000 individuals. Implementation is set to begin July 1, 2023. Contracts are currently worth $1.8 billion annually.
RFP
MCOs will provide integrated physical health, behavioral health, pharmacy, and dental services. Dental services are currently not covered under the MCO contracts and are instead provided under a separate dental benefit management contract. With the integration of dental services in the upcoming contracts, Nebraska Medicaid will be increasing dental rates to providers and removing the annual dental benefit limits for adults.
MCOs will be required to have a Fully Integrated Dual Eligible (FIDE) Dual Special Needs Plan (DSNP) in place no later than January 1, 2024.
Winning bidders will also be required to establish a common provider credentialing service. MCOs will work with all other contracted MCOs to jointly procure a Central Credentialing Verification Subcontractor (CCVS). The CCVS must begin its work at full capacity no later than one year from the start of the MCO’s contract start date. The CCVS will help reduce administrative burdens on providers and streamline the process to improve member access. A provider seeking to be credentialed with any of the MCOs will need to only submit a single application to the CCVS.
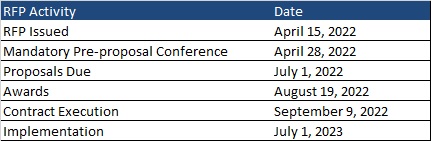
Timeline
A mandatory pre-proposal conference will be held on April 28, 2022. Proposals are due by July 1, 2022, with awards expected August 19. Contracts will be executed September 9, 2022, and implementation will begin July 1, 2023. Contracts will run for five years with two one-year renewal options.
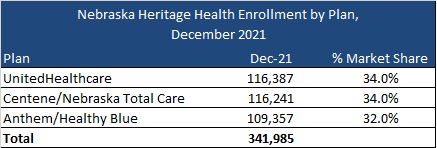
Current Market
Current incumbents are Anthem/Healthy Blue, Centene/Nebraska Total Care, and UnitedHealthcare, serving 342,000 Medicaid members as of December 2021.
Evaluation
Proposals that meet the mandatory requirements will be scored out of a total possible 6,600 points. Part 1, consisting of the corporate overview, will be worth 1,000 possible points. The corporate overview should include:
- the ability, capacity, and skill of the bidder to deliver and implement the system or project that meets the requirements of the solicitation
- the character, integrity, reputation, judgment, experience, and efficiency of the bidder
- whether the bidder can perform the contract within the specified time frame
- the quality of vendor performance on prior contracts
Part 2, consisting of the approach, will be worth 5,100 points. Bidders will provide a detailed response on how managed care services will be provided. Topics include:
- eligibility and enrollment
- business requirements
- staffing requirements
- covered services and benefits
- member services and education
- grievances and appeals
- provider network requirements
- provider services
- subcontracting requirements
- care management and case management
- quality management
- utilization management
- program integrity
- provider reimbursement
- systems and technical requirements
- claims management
- reporting and deliverables
- transition and implementation
- electronic visit verification for home health care services
Oral interviews, if required, will be worth 500 points.
HMA Roundup
California
California Assembly Committee to Hold Hearing on Bill Allowing No-Bid Medi-Cali Contract. California Healthline reported on April 18, 2022, that the California Assembly Committee on Health will hold its first hearing on a bill (AB 2724) that would allow the state to enter into a no-bid Medi-Cal contract with Kaiser Permanente. Stakeholder groups opposing the legislation include Local Health Plans of California, the California State Association of Counties, and the National Union of Healthcare Workers. Read More
California Hospital Loses Medicaid, Medicare Funding. ABC7 reported on April 14, 2022, San Francisco’s Laguna Honda Hospital has lost access to Medicare and Medicaid funding in light of issues with hygiene and infection prevention and control. The hospital will continue to receive Medicare and Medicaid payments over the next 30 days but cannot take on any new patients. The hospital serves approximately 700 patients. Read More
Connecticut
Connecticut Seeks Medicaid Waiver to Address Coverage Gap. The Connecticut Department of Social Services submitted on April 1, 2022, a Section 1115 waiver application to provide Exchange plan premium assistance to individuals who exceed the Medicaid income limit but do not exceed 175 percent of poverty. Eligible individuals would include parents or caretaker relatives and dependents under age 26 as well as non-pregnant childless adults aged 19 to 64. Dental services and non-emergency medical transportation services comparable to the benefits under Connecticut Medicaid would also be provided. The federal public comment period will be open until May 13. Read More
Florida
Florida Health Plan Pays Fine for Failing to Pay Provider Claims. Florida Politics reported on April 16, 2022, that Centene/Sunshine Health Plan has paid the Florida Agency for Health Care Administration $9.1 million for failing to pay more than 121,000 in provider claims. A state ban on Medicaid managed care auto-enrollment in Sunshine remains in effect. Sunshine blamed software issues following its acquisition of WellCare. Read More
Medicaid Claims Settlement Elicits Comment from Pinellas County Juvenile Welfare Board CEO. The Tampa Bay Times reported on April 14, 2022, that Beth Houghton, chief executive of the Juvenile Welfare Board (JWB) of Pinellas County defended the organization’s role in a Medicaid false claims scheme. BayCare agreed to pay $20 million to settle a lawsuit alleging it illegally donated money to JWB to increase its federal Medicaid matching funds. Read More
Illinois
Illinois Senate Passes Automatic Medicaid Renewal Legislation. The Illinois Senate Democratic Caucus reported on April 13, 2022, that the Illinois Senate passed House Bill 4343, which automatically renews Medicaid coverage without requiring beneficiaries to report changes in income. Individuals with zero income would also be auto-renewed. Under current law, Medicaid beneficiaries must report changes in income for 12 months after approval or redetermination. The bill also includes Medicaid coverage for midwife services and increased funding for dental care and non-emergency medical transportation. The bill heads back to the House, which has already passed a previous version. Read More
Kansas
Kansas Adopts Full Practice Authority for Nurse Practitioners. The American Association of Nurse Practitioners announced on April 15, 2022, that Kansas enacted a law adopting full practice authority (FPA), which authorizes nurse practitioners to evaluate patients; diagnose, order, and interpret diagnostic tests; and initiate and manage treatments under a single license with the state board of nursing. Kansas is the 26th state to adopt FPA. Read More
Kansas Lacks Effective System for Tracking HCBS Waiver Program Redeterminations, Audit Finds. A Kansas audit released on April 13, 2022, found that the agency responsible for administering the state’s Medicaid home and community-based services (HCBS) waiver program lacked an effective system for tracking beneficiary redeterminations. The audit, released by Kansas Medicaid Inspector General Steven Anderson, identified 2,854 HCBS waiver members without any HCBS claims filed on their behalf. Read More
Kentucky
Kentucky Enacts Law to Cover Individuals with Sickle Cell Disease Under Medicaid. WHAS reported on April 14, 2022, that Kentucky enacted a law (Senate Bill 276) that will expand Medicaid to cover individuals with sickle cell disease. The law will go into effect in 90 days. Read More
Massachusetts
Massachusetts Extends Postpartum Medicaid Coverage From 60 Days to 12 Months. The Massachusetts Executive Office of Health and Human Services announced on April 19, 2022, the extension of postpartum Medicaid coverage from 60 days to 12 months. The extension was effective on April 1, 2022. Read More
Health Policy Commission Raises Health Care Cost Growth Benchmark to 3.6 Percent. The Boston Business Journal reported on April 13, 2022, that the Massachusetts Health Policy Commission (HPC) voted to raise its health care cost growth benchmark for the state to 3.6 percent for 2023, the highest level in the last five years. HPC predicts that 2021 and 2022 spending will exceed the 3.1 percent threshold set in response to COVID-19. Read More
Michigan
MI Extends Postpartum Medicaid Coverage to 12 Months. The Centers for Medicare & Medicaid Services announced on April 14, 2022, the approval of a state plan amendment allowing Michigan to extend postpartum Medicaid coverage to 12 months. There are an estimated 16,000 pregnant and postpartum individuals who will receive coverage. Read More
Mississippi
Mississippi to Implement Centralized Credentialing Process for Medicaid Managed Care Network Providers. Y’all Politics reported on April 18, 2022, that the Mississippi Division of Medicaid will implement a centralized credentialing process for providers enrolling in the networks of Medicaid managed care plans, which the state refers to as coordinated care organizations (CCOs). Effective July 2022, providers serving CCOs for MississippiCAN or the Children’s Health Insurance Program will utilize the same screening process currently used for fee-for-service Medicaid. Providers will still be required to complete a separate credentialing process with the CCOs. Read More
Mississippi Hires Analytics Firm to Investigate PBMs. The Daily Journal reported on April 17, 2022, that Mississippi State Auditor Shad White has hired Delaware-based data analytics firm Intelaform to collect and analyze data on pharmacy benefit managers (PBMs). The contract runs through June 30, 2023, and the services are being provided at no cost to the state. Read More
Mississippi Economic Development Organization Calls on Lawmakers to Expand Medicaid. Mississippi Today reported on April 14, 2022, that Medicaid expansion received the backing of the Delta Council, a lobbying group and economic development organization. Approximately 225,000 Mississippians would qualify for Medicaid expansion. Read More
Missouri
Missouri Senate Committee Advances Measure Aimed at Making Funding of Medicaid Expansion Optional. The Missouri Independent reported on April 13, 2022, that the Missouri Senate Appropriations Committee advanced a proposed constitutional amendment aimed at making Medicaid expansion funding optional. The measure, which requires voter approval, would allow lawmakers to decide each year whether to fund expansion. The measure has already cleared the House. Missouri voters approved Medicaid expansion in a ballot measure in 2020. Read More
Montana
MT Medicaid Expansion Beneficiaries See Decline in ER Use, Report Finds. Montana Public Radio reported on April 13, 2022, that individuals enrolled in the Montana Medicaid expansion program experienced a decline in emergency department utilization over time, according to a report from the Montana Healthcare Foundation. Individuals enrolled for one to three years saw emergency visits decrease between 10 percent and 30 percent; instead, beneficiaries tended to use outpatient services. Read More
New York
New York Made $965 Million in Improper Payments to Inactive Medicaid Providers, Audit Finds. Crain’s New York reported on April 20, 2022, that the New York State Department of Health made improper payments of $965 million to Medicaid providers listed as inactive, according to an audit from the office of the state comptroller. The audit included payments from January 2015 through December 2019. Read More
Ohio
Ohio Advocate Says 10-15 Percent of Medicaid Members Could Lose Coverage When Redeterminations Begin. Statehouse News Bureau reported on Wednesday April 13, 2022, that 200,000 to 300,000 Ohio Medicaid enrollees could lose coverage when the state begins eligibility redeterminations after the public health emergency ends, according to John Corlett, executive director of the Center for Community Solutions and former state Medicaid director. The figure represents about 10 to 15 percent of Medicaid beneficiaries in the state. Read More
Pennsylvania
Pennsylvania Delays Implementation of Modified Medicaid Managed Care Contracts to August 1. WFMZ/The Center Square reported on April 19, 2022, that the Pennsylvania Department of Human Services (DHS) has delayed implementation of modified Medicaid managed care contracts from July 1 to August 1. The state blamed difficulties being experienced by at least one plan in network negotiations with UPMC, which could affect network adequacy requirements. The modified contracts include draft language preventing Medicaid plans from including providers that have had work stoppages in the past five years unless the provider’s employees are now unionized.
Vermont
Vermont Releases Survey on Mobile Crisis Intervention. WCAX reported on April 15, 2022, that the Vermont Agency of Human Services is seeking feedback on how it should allocate federal funds for mobile crisis intervention services. Survey responses are due by April 29. Read More
Wisconsin
Wisconsin Governor Vetoes Two Bills Aimed at Tightening Medicaid Eligibility Requirements. WisPolitics.com reported on April 15, 2022, that Wisconsin Governor Tony Evers vetoed two bills aimed at tightening Medicaid eligibility requirements. One bill (Senate Bill 905/Assembly Bill 934), would require the Department of Health Services (DHS) to review individual Medicaid eligibility every six months and prohibit automatic renewal. The other bill (Senate Bill 912/Assembly Bill 936), would take away Medicaid benefits from able-bodied childless adults who turn down a job offer or additional work that would make them ineligible for benefits. Read More
National
CMS Releases Action Plan to Advance Health Equity. The Centers for Medicare & Medicaid Services (CMS) released on April 20, 2022, an action plan to advance health equity by striving to close gaps in access, promote culturally appropriate services, build on outreach and enrollment efforts, standardize data collection, better support safety net providers, and other measures. CMS will convene industry stakeholders beginning in Summer 2022 to ensure progress toward these goals. Read More
CMS Proposes 3.2 Percent Increase to Fiscal 2023 Inpatient Hospital Payments. Modern Healthcare reported on April 18, 2022, that the Centers for Medicare & Medicaid Services proposed increasing inpatient hospital payments by 3.2 percent in fiscal 2023, according to the proposed fiscal 2023 Hospital Inpatient Prospective Payment System rule. Read More
U.S. Supreme Court Dismisses Medicaid Work Requirements Cases as ‘Moot’. Modern Healthcare reported on April 18, 2022, that the U.S. Supreme Court dismissed challenges to Medicaid work requirements in Arkansas and New Hampshire, calling the cases “moot” after the Biden administration revoked regulatory approval of the requirements. Read More
Justice-Involved Individuals Gain Coverage Through Medicaid Expansion, Study Finds. Health Payer Intelligence reported on April 18, 2022, that Medicaid expansion is reaching justice-involved individuals. According to a study in JAMA Health Forum, 82.5 percent of eligible, justice-involved individuals were enrolled in Medicaid in expansion states, while only 54.2 percent were enrolled in non-expansion states. Overall, the study found a 14.9 percentage point increase in Medicaid coverage for justice-involved individuals from 2010 to 2017 as a result of expansion. Read More
Exchange Plan Premiums Fall 1.8 Percent, Study Finds. The Robert Wood Johnson Foundation (RWJF) reported on April 12, 2022, that average Exchange premium rates fell 1.8 percent in 2022, according to a report from the Urban Institute. Average Exchange premium rates fell 1.7 percent in 2021 and 3.2 percent in 2020. The report suggests several factors that could lead to lower Exchange rates, including increased competition, an improving risk pool, and other factors. Read More
MACPAC Releases Updated Reference Guide to Federal Medicaid Statute, Regulations. The Medicaid and CHIP Payment and Access Commission released on April 14, 2022, an updated reference guide to the federal Medicaid statutes and regulations. Read More
Industry News
Pritzker Organization to Acquire Epic Staffing Group. The Pritzker Organization announced on April 18, 2022, a definitive agreement to acquire Epic Staffing Group, which provides outsourced staffing for biopharmaceutical and healthcare organizations. Financing for the acquisition, which is expected to close this year, will be provided by Truist Securities and Wells Fargo Securities. Read More
FFL Partners Announces Investment in Perlman Clinic. FFL Partners announced on April 18, 2022, an investment in Perlman Clinic, with 100 primary care providers in 16 facilities in the greater San Diego market. FFL Partners, a private equity firm, plans to expand the provider’s presence in southern California, where Perlman Clinic has both capitated and fee-for-service contracts with health plans. Read More
Centene Board Member Leslie Norwalk Resigns. Modern Healthcare reported on April 15, 2022, that Leslie Norwalk resigned from the Centene board of directors, citing a disagreement over the company’s governance process. Norwalk joined the board in January 2022. She is strategic counsel to law firm Epstein Becker Green and formerly served as administrator of the Centers for Medicare & Medicaid Services. Read More
Commonwealth Care Alliance Acquires Vitality Health Plan of California. Commonwealth Care Alliance (CCA) announced on April 14, 2022, the acquisition of Vitality Health Plan of California, which operates two Medicare advantage plans primarily serving Santa Clara and San Joaquin counties. Vitality’s plans will operate under the name CCA Health California, effective immediately. CCA expects to continue expanding in California. Read More
Kaiser Permanente to Invest $200 Million More in Affordable Housing. Modern Healthcare reported on April 14, 2022, that Kaiser Permanente (KP) will invest another $200 million in its Thriving Communities Fund, which creates and preserves affordable housing across the U.S. The new investment will double KP’s initial investment in the fund and allow for the support of 30,000 housing units before 2030. Read More
Cigna Launches Initiative to Improve Care for Individuals With Autism. Modern Healthcare reported on April 14, 2022, that Cigna has launched an initiative to develop autism treatment standards, common performance metrics, and improvements to care access for individuals with autism. Cigna is working with Behavioral Health Center of Excellence, which accredits organizations providing applied behavior analysis services. Read More
Humana to Invest Additional $25 Million in Affordable Housing. Humana announced on April 13, 2022, that it will invest another $25 million to increase the supply of affordable housing in states including Florida, Georgia, Illinois, Indiana, Kentucky, Louisiana, Ohio, Oklahoma, South Carolina, Virginia, Wisconsin. Humana, which invested $25 million last year, said the program takes advantage of low-income tax credits. Read More
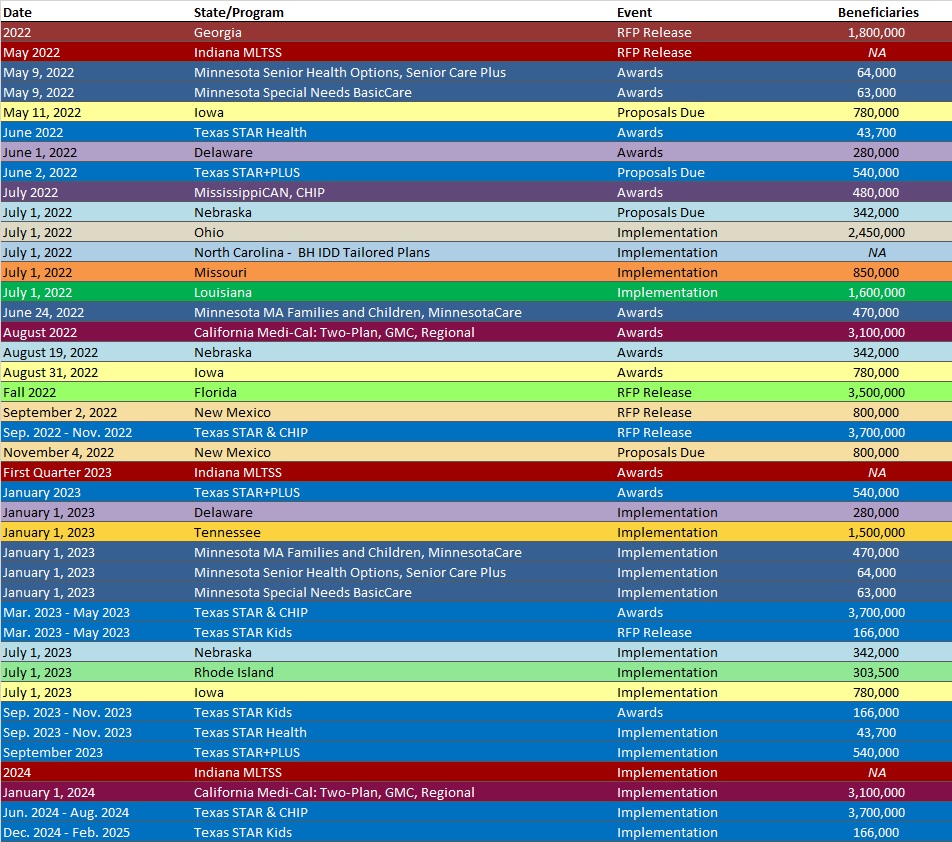
RFP Calendar
Company Announcements
HMA News & Events
HMA Welcomes New Colleagues:
Robert Ross, FACHE
Principal
New York, NY
An experienced healthcare executive, Robert Ross is dedicated to developing solutions to provide quality, accessible, cost-effective care while ensuring the sustainability of safety-net providers to meet the needs of their communities. Rob’s expertise includes strategic planning, system integration, financial turnaround, continuum of care strategies, provider alignment, service line development, and leadership development.
During his long tenure with St. Luke’s Cornwall Hospital in Newburgh, New York where he served in leadership positions including vice president and president and chief executive officer. While there, Rob led the financially distressed organization through a financial turnaround resulting in a more than 40% bottom-line improvement in one year. He led the board and community through the development and implementation of a strategic plan focused on long-term stability of the hospital. This process included the evaluation of partnerships culminating in the merger with an academic medical center. Also, while at St. Luke’s, he planned and executed a $150 million master facility plan, integrated two hospitals, developed three clinical institutes, achieved Healthgrades Patient Safety award for five consecutive years and launched 10 new service lines.
As COO of 912-bed Medstar Washington Hospital Center in the District of Columbia, Rob led efforts resulting in improved operational performance reducing emergency department wait time, inpatient length of stay, and patient time to admission. He created the Office of Patient Experience resulting in improved CMS star ratings. In addition, he collaborated on an assessment of behavioral health services and led resulting improvement efforts.
As regional executive vice-president with Westchester Medical Center he led the execution of a financial stabilization plan, integrated four community hospitals and developed a regional primary care practice.
Rob earned a Master of Health Services Administration from George Washington University, and a bachelor’s degree in computer and information sciences from Brooklyn College. He is a Fellow of the American College of Healthcare Executives and has served on community non-profit boards. In addition, he is an adjunct professor of management and healthcare policy and serves as a local Red Cross Disaster Response leader.
Catherine Knox, RN, PHN, MSN
Principal
Los Angeles, CA
An experienced nurse leader with a focus on advancing population health, Catherine Knox is a diverse and seasoned innovator who has led efforts to support population health in value-based settings to address healthcare disparities.
Before joining HMA, she served as clinical director of both integrated care management and practice transformation for Inland Empire Health Plan where she collaborated with senior leadership in planning and operations of the plan’s Health Home program and launch of the California Advancing and Innovating Medi-Cal (CalAim) Enhanced Care Management (ECM) program.
Catherine has worked in primary care practice transformation, the safety-net delivery system, and public health including emergency preparedness and response. In addition, her nursing background includes critical care nursing with a focus in cardiothoracic intensive care, working with children and families in dependency court, as well as hospice nursing.
As vice president of CalMedi Connect program development, she supported development of the CalMedi Connect program for 10,000 dual eligible members in southern California and reduced acute admissions while increasing in-home support services caregiver engagement.
Her leadership experience includes working in the Los Angeles County Department of Public Health as a nurse manager and program specialist developing and implementing emergency preparedness and response activities for the department.
Catherine earned a Master of Science in nursing from Norwich University, a bachelor’s degree, also in nursing, from California State University, Los Angeles, and a Comprehensive Nursing Diploma from Auckland Technical Institute. She is a registered nurse, licensed in California and holds several FEMA certifications. In addition, she holds a National Committee for Quality Assurance Patient-Centered Medical Home Content Expert Certification.
Mayur Chandriani
Associate
Washington, DC
An experienced non-profit manager, Mayur Chandriani is committed to programs focused on immigrant healthcare, maternal and child health and community involvement.
Before joining HMA, Mayur led a county-wide substance abuse prevention and outreach program aimed, but not limited to, Latino populations with the Latin American Community Center (LACC). While there, he provided prevention education, developed and disseminated educational materials and handled referrals to treatment and therapy.
A skilled facilitator and program manager, Mayur has facilitated community partnerships and capacity building efforts including LACC Advocacy Task Force, Fetal Alcohol Syndrome Disorder (FASD) Task Force, and Safe Kids Delaware. He was an active member of the Delaware Community Response Team (CRT), a pilot initiative jointly funded by the Delaware Division of Public Health and HMA. In that role, he which responded to sentinel events, provided opioid misuse prevention education, and distributed naloxone alongside a team of diverse stakeholders.
With a background in education, Mayur also has experience with early childhood education and sports and was previously a student advisor and facility manager with Kaplan Test Prep and Admissions. He is a certified prevention specialist and has completed certificates in nonprofit leadership and immigration law. He earned a bachelor’s degree in biological sciences from Drexel University.
Michael Chittenden
Principal
Phoenix, AZ
As a professional in the intellectual/developmental disabilities (I/DD) field with over 35 years of experience, Michael has established and maintained positive relationships throughout the United States with governmental, social/human services, advocacy, religious, and other business leaders.
He has served in a variety of positions including director of population health in Medicaid Managed Care, behavior management coordinator, executive director and regional director in program services, and he is the former executive director of The Arc of Nebraska.
Michael has worked to create effective supports with other disability advocates and fields of service. He has served on the Governor’s I/DD Advisory Committee, the Brain Injury Advisory Committee, the Nebraska Consortium of Citizens with Disabilities, the State Rehabilitation Committee, and as a statewide advisor to People First Nebraska. He is president of the Nebraska Transition College.
Daniel Nemet
Actuarial Consultant, Edrington Health Partners
Phoenix, AZ
A seasoned actuary and presenter, Daniel Nemet is skilled in various programming and coding systems and regulations surrounding healthcare actuarial work.
He joins Edrington Health Partners after serving with UnitedHealth Group where he had oversight of filing quarterly reports for healthcare clients as well as reporting for sales and underwriting departments.
Daniel spent more than seven years with Blue Cross Blue Shield of Arizona working in pricing and rate filing as well as forecasting and reserving. He developed, presented, and filed all Patient Protection and Affordable Care Act (PPACA) and pre-ACA individual products as well as wrote SAS code, maintained, and updated pricing models and prepared corporate incurred but not reported (IBNR) triangles and assisted decisions on completion factors for Medicare clients.
He earned a Bachelor of Science degree in mathematics from Arizona State University and has passed several actuarial exams. He is involved in professional service organizations and volunteers with youth programs.
Jodi Carter-Jones, DNP, MSN FNP-BC, NEA-BC, LSSBB-Healthcare
Senior Consultant
Denver, CO
Double board certified as both an advanced nursing executive and family nurse practitioner, Jodi Carter-Jones is a results-focused healthcare leader with expertise in all aspects of healthcare delivery services, managed care, program development and evaluation, policy creation, and education.
Before joining HMA, Jodi served in several roles and leadership positions as an independent family nurse practitioner, including working in rural health, government contracts, and providing telemedicine, primary care, and independent medical exams for veterans. In addition, her previous work also includes serving as national lead for regulatory compliance, business development, and clinical programs director with CVS Health overseeing CMS contracts, fee-for-service transitions to managed care, integrated care models, directing senior leadership teams, and value-based innovations.
A strategist and convergent thinker with demonstrated success in implementing the Quadruple Aim of improving population health, patient, and provider satisfaction, and reducing per capita cost as a collaborator with payers and health systems, she has a wide range of clinical operations and patient care expertise including clinical strategy, innovation, clinical quality improvements, leadership, and mentoring. Dr. Carter-Jones is also an adjunct professor for a graduate nursing program and teaches organizational theory and leadership.
She earned her doctoral degree from the University of South Alabama and two Masters of Science degrees, ne in executive administration and one as a family nurse practitioner. She is a Lean Six Sigma Blackbelt in Healthcare, fellow of the Management and Strategy Institute, certified in Trauma-Informed care, and holds several Federal Emergency Management Agency and Centers for Disease Control and Prevention certifications. Dr. Carter-Jones is licensed in multiple states.
Lindsey Kato
Senior Consultant
Seattle, WA
Lindsey Kato is a public health professional who specializes in multidisciplinary work to strategically address complex issues at the intersection of public health and public safety.
She returned to HMA after two years embedded within the Centers for Disease Control and Prevention (CDC) Division of Overdose Prevention, through the CDC Foundation, where she served as the training and strategy lead for the National Overdose Response Strategy (ORS). In that role, Lindsey oversaw the technical assistance and training components of the program, as well as supported the strategic direction of the program, helping the program align with other state and federal overdose, substance use prevention and treatment funding and priories.
During her career, she has worked on projects including planning and facilitating state law enforcement summits and developing and providing ongoing training and technical assistance to states and communities. In addition, she has worked implementing overdose prevention including, provider education, naloxone distribution, safe disposal of household medication, and medication assisted treatment (MAT) in community and correctional setting. She has also built multidisciplinary coalitions and task forces around shared visions and goals.
Additionally, Lindsey has consulted for public safety agencies across the country to minimize overdose risk by working with public and behavioral health partners to implement sustainable solutions based on meaningful partnerships. In 2017, Lindsey was awarded the U.S. Attorney’s Award for Outstanding Contributions to Cooperative Law Enforcement.
Prior to her work in overdose prevention, Lindsey coordinated community suicide prevention efforts in her hometown of Juneau, located in Áak’w Kwáan Territory in Southeast, Alaska.
Lindsey has a Master of Public Health in epidemiology from the Colorado School of Public Health and a Bachelor of Science in public health, focused on health promotion and behavior, from Oregon State University.
New This Week On HMA Information Services (HMAIS):
Medicaid Data
- Colorado RAE Enrollment is Up 1.5%, Feb-22 Data
- Michigan Dual Demo Enrollment is Down 4.6%, Jan-22 Data
- Michigan Medicaid Managed Care Enrollment is Flat, Jan-22 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Nebraska Heritage Health Medicaid Managed Care RFP, Apr-22
Medicaid Program Reports, Data and Updates:
- Arizona Quarterly Progress Reports for CMS, 2019-22
- Arkansas DHS Annual Statistical Reports, 2018-21
- California Medicaid Older Adult Full Scope Expansion Presentation, Feb-22
- Georgia Medicaid External Quality Review Reports and CMO Compliance Reports, 2017-22
- Kansas OMIG Medicaid HCBS Waiver Program Audit, Apr-22
- Michigan Medicaid Health Plan HEDIS Reports, 2016-21
- Minnesota Managed Care HEDIS Reports, 2016-21
- New York Managed Care Medical Loss Ratio Reports, SFY 2018
- New York State Comptroller Audits of Medicaid Program, Apr-22
- Oklahoma Medical Advisory Meeting Materials, 2017-22
- Tennessee Medicaid Managed Care HEDIS/CAHPS Reports, 2015-21
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio at [email protected].
