This week's roundup:
- In Focus: New HMA Report Provides Insights on Strengthening State Medicaid NEMT Contracts
- HMA Expert Take: Plan for Changes in the Digital Quality Landscape in Healthcare
- Senior Senate Finance Committee Staffer Joins Leavitt Partners
- Arizona Issues Statewide ALTCS Case Management Services RFI
- Indiana Governor Signs Multiple Executive Orders Aligned with Make America Healthy Again Initiative
- Michigan Governor Orders DHHS Review of Medicaid Cut Impacts
- Ohio Medicaid Saved $140 Million After Moving to SPBM, Report Finds
- Ohio, West Virginia Rural Hospitals Form Integrated Network to Support Value-Based Care
- Accreditation Entities to Develop Standards Around AI Usage in Healthcare
In Focus
New HMA Report Provides Insights on Strengthening State Medicaid NEMT Contracts
This week, our In Focus section reviews insights from a new Health Management Associates (HMA) report, State Medicaid Non-Emergency Medical Transportation Contracts: Key Provisions, Standards, and Considerations. States are required to provide non-emergency medical transportation (NEMT) as part of their Medicaid programs, and NEMT can help improve health outcomes by reducing barriers to care, particularly for individuals with chronic conditions, disabilities, or living in rural areas.
States have considerable flexibility in the design and operation of their NEMT programs. As a result, states vary widely in their NEMT procurement and contract standards, metrics, reporting, and enforcement of requirements for NEMT brokers, managed care organizations (MCOs), and transportation providers.
This article reviews HMA’s analysis and identified strategies that states and their partners can adopt to enhance the quality and efficiency of their NEMT programs.
NEMT Landscape
Federal statute requires states to provide NEMT services to Medicaid enrollees who are without access to other transportation options to visit providers of medically necessary healthcare services. Though states must meet certain minimum federal requirements, they have flexibility to develop NEMT models that reflect local and regional dynamics and needs. States use different administrative models, including statewide brokers, regional brokers, and managed care carve-ins. Each model has unique strengths and challenges.
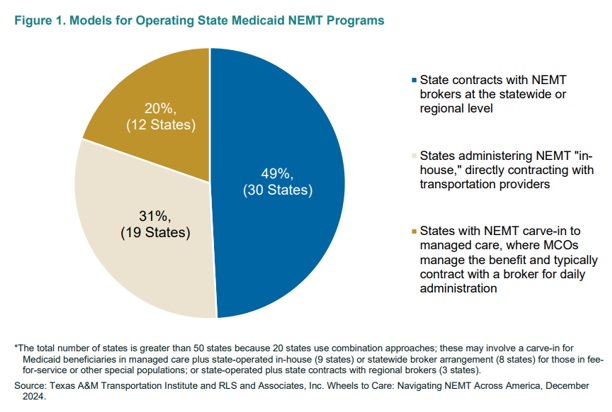
Figure 1 breaks down the models that states use for their NEMT programs.
Most states contract with NEMT brokers directly to manage the benefit or carve NEMT services into their contracts with Medicaid MCOs. MCOs with the NEMT benefit carved into their contracts usually subcontract with NEMT brokers, but some may also contract directly with transportation providers. Brokers manage call centers, ride scheduling, quality control, and build provider networks through agreements with local transportation providers. Some states manage NEMT in-house, and many states use a combination of approaches for different Medicaid populations.
Key Findings about NEMT Programs
HMA’s analysis of NEMT contracts, Requests for Proposals (RFPs), and programs across multiple states revealed the following:
- Critical Contract Elements: Stakeholders emphasized the importance of contract provisions that prioritize rider safety, robust network adequacy, reasonable call center metrics, and positive rider experiences.
- Challenges: Common issues include transportation provider shortages, late pickups, driver and rider no-shows, insufficient payment rates, and rider complaints.
- Technology Integration: States and brokers are increasingly leveraging technology, such as GPS tracking, mobile apps, vehicle cameras, and artificial intelligence (AI) to improve efficiency, program integrity, and rider experience.
- Program Integrity: Fraud, waste, and abuse remain concerns, particularly for mileage reimbursement (for Medicaid beneficiaries who drive themselves or have family/friends drive them to appointments) and high-utilization services (such as recurring trips to methadone clinics). States are implementing trip verification tools and other innovations to address these issues.
- Emerging Trends: States are expanding the use of transportation network companies (TNCs) like Uber and Lyft but acknowledge that guardrails for the use of TNCs for NEMT are needed. National standards for certain aspects of NEMT contracting and quality control in development.
Considerations for NEMT Procurements and Program Operations
State Medicaid agencies ultimately are responsible for providing their members with safe, timely, and efficient transportation. The HMA report identifies several areas for improvement and key considerations for states, including the need to balance standardized contract and program features with flexibility to innovate and respond to local needs. Leveraging contracts as a strategic tool, states may:
- Use standardized contract provisions to reduce administrative burden on NEMT brokers while tailoring requirements to state-specific needs, including urban and rural distinctions
- Ensure adequate payment rates that enable brokers to maintain robust provider networks, including flexibility to offer higher rates for rural areas
- Define clear contract performance metrics and enforcement mechanisms that prioritize rider safety and on-time performance
- Educate beneficiaries about mileage reimbursement options, assist healthcare facilities with their own vehicles to participate in NEMT, and encourage brokers and MCOs to use creative solutions, such as TNCs and volunteer drivers, to address transportation provider shortages
- Use procurements to encourage or incentivize brokers to adopt innovative technologies like AI, reloadable debit cards for public transit fare, and member-facing apps to improve access, efficiency, and program integrity
- Strengthen collaboration among states, brokers, transportation providers, healthcare facilities, and Medicaid beneficiaries to address challenges and improve program outcomes
All Medicaid stakeholders, including states, MCOs, brokers, transportation and healthcare providers, beneficiary advocates, technology innovators, and other interested organizations, have critical roles in shaping Medicaid NEMT programs. NEMT stakeholders can:
- Stay informed about federal Medicaid policy developments shaping state approaches to the NEMT benefit
- Engage with state policymakers, particularly state Medicaid agency leaders, to understand their state and local landscapes
- Collaborate with other stakeholders to identify challenges and solutions
- Educate and advise policymakers and partners on the adoption of innovative technologies that enhance enforcement strategies, program efficiency, and integrity
- Support assessment of the impact of NEMT strategies and innovations on access, safety, timeliness, and cost-effectiveness
Connect with Us
HMA offers expertise in Medicaid policy, program design, and evaluation to help states and stakeholders optimize their NEMT programs and advance their organizations’ goals. Our experts support clients in design and development of programs and RFPs that balance standardization, flexibility, and state-specific needs.
Read the full report here. For more information about Medicaid NEMT program contact report authors Sharon Silow-Carroll, Carrie Rosenzweig, and Jacob Briscoe.
HMA Expert Take: Plan for Changes in the Digital Quality Landscape in Healthcare
Digital quality measures (dQM) are becoming a cornerstone of healthcare operations. Propelled by federal initiatives and mandates, these measures are designed to enhance interoperability, transparency, and real-time data sharing. As healthcare organizations face increasing pressure to do more with fewer resources, digital innovation is becoming essential for driving efficiency and reducing administrative burden.
There is ongoing speculation about how the Trump Administration and Congress will approach digital healthcare transformation, particularly in areas like digital quality measurement. Recent indicators suggest they will stay on this course, and perhaps even accelerate the adoption of digital quality measures.
As part of Centers for Medicare & Medicaid Services (CMS) initiatives to transition to a fully digital landscape, for example, the agency is planning to update Medicare’s quality measurement and interoperability programs to prioritize safety and outcomes. Specifically, the fiscal year 2026 Hospital Inpatient Prospective Payment System (IPPS) and Long-Term Care Hospital Prospective Payment System (LTCH PPS) Proposed Rule includes a request for information (RFI) to gather comments on potential future quality measures, implementing Fast Healthcare Interoperability Resources® (FHIR®), modernizing health reporting, and reducing burden.
Health Management Associates (HMA), national digital healthcare experts, including, Ryan Howells and Cameron Graham, are actively focusing on this hot topic. In their HMA blog post they offer valuable insights and guidance to navigate this dynamic federal policy landscape.
Organizations that proactively adapt to these evolving mandates will be better positioned to improve patient outcomes, streamline operations, and remain leaders in this evolving market. Our experts can help your organization stay on top of compliance requirements and deadlines, as well as financial and legal risks. Our teams also are able to assess organizational readiness to succeed in this quickly changing healthcare landscape.
Get more insights here and learn more about HMA’s approach to dQM.
Senior Senate Finance Committee Staffer Joins Leavitt Partners
Leavitt Partners, an HMA Company, is pleased to announce that Conor Sheehey has joined the company’s team of health policy experts as a director, located in Washington, D.C.
Sheehey most recently served as senior health policy advisor to U.S. Senate Finance Committee Chair Mike Crapo (R-ID). In this role, he advised the Committee on a range of health care policy issues, including prescription drug pricing, telehealth, AI, provider coverage and reimbursement, fraud and abuse, medical devices, and Medicare Parts B and D. Sheehey led several bipartisan legislative efforts, including the development of comprehensive PBM reforms and bipartisan proposals on clinician payment reform and drug shortages.
Prior to his work at the Senate Finance Committee, Sheehey served as deputy legislative director for U.S. Senator Tim Scott (R-SC). Sheehey advised the Senator on all matters related to health care, education, workforce, human services, and retirement security policy before both the Senate Finance Committee and the U.S. Senate Health, Education, Labor, and Pensions (HELP) Committee.
Sheehey will advise clients throughout the health care sector on federal health care policy, strategy, and advocacy. He will also develop and manage multi-sector alliances.
“We are pleased to have Conor bring his deep Medicare expertise, bipartisan relationships, and creativity into the Leavitt Partners team,” said Josh Trent, chief executive officer, of Leavitt Partners. “Conor will hit the ground running to help clients across our enterprise who are seeking to navigate policy uncertainty and political processes to improve federal policy and health outcomes for millions of Americans.”
Sheehey joins a team of highly experienced, bipartisan health policy and government affairs consultants. The Leavitt Partners team includes former health policy directors and counsels of the U.S. Senate Budget Committee, the Senate HELP Committee, the U.S. House Energy and Commerce Committee, and other senior congressional staff. Leavitt Partners, founded by former HHS Secretary Michael O. Leavitt, features former senior political appointees in Democratic and Republican presidential administrations, leaders formerly serving in several U.S. Department of Health and Human Services (HHS) agencies, and former leaders in the nonprofit and corporate health sectors.
HMA Roundup
Arizona
Arizona Issues Statewide ALTCS Case Management Services RFI. The Arizona Health Care Cost Containment System (AHCCCS) issued on April 15, 2025, a Request for Information (RFI) seeking input on the potential creation of a standalone statewide case management contract for Arizona Long Term Care Services (ALTCS), which covers approximately 25,000 elderly and/or physically disabled members. Current case management is provided through the managed care organization (MCO) contracts. Eligible respondents include Medicaid/Medicare MCOs, social service agencies, or other qualified entities. AHCCCS seeks input on service delivery models, technology, compliance, cost structures, and return on investment. Responses are due by April 28, 2025.
Indiana
Indiana Governor Signs Multiple Executive Orders Aligned with Make America Healthy Again Initiative. Fierce Healthcare reported on April 16, 2025, that Indiana Governor Mike Braun has signed nine executive orders at a “Make Indiana Healthy Again” press conference, which aim to align the state with the Trump administration’s Make America Healthy Again initiative. One order seeks to bolster the state’s Medicaid program integrity and reduce costs by directing the state to submit a report to the Centers for Medicare & Medicaid Services (CMS) on improper payments by October 2025, to no longer accept certain eligibility information without verification before enrollment unless federally required, and to review eligibility information more frequently. Other executive orders focused on food-related and prevention initiatives, which would impose stricter work and eligibility requirements from the Supplemental Nutrition Assistance Program (SNAP), remove candy and soft drinks from SNAP, prompt evaluations of food dyes and diet-related chronic diseases, and increase direct-to-consumer food.
Michigan
Michigan Governor Orders DHHS Review of Medicaid Cut Impacts. Michigan Advance reported on April 17, 2025, that Michigan Governor Gretchen Whitmer signed an executive directive ordering a state analysis by the Department of Health and Human Services (DHHS) of how federal Medicaid funding cuts could impact Michigan. Whitmer warned that cuts could jeopardize care for children, seniors, and people with disabilities, especially in rural areas. Michigan has 2.6 million Medicaid members, with Medicaid representing 34 percent of the state’s total budget.
Ohio
Ohio Medicaid Saved $140 Million After Moving to SPBM, Report Finds. The Ohio Capital Journal reported on April 17, 2025, that the Ohio Department of Medicaid (ODM) saved $140 million over a two-year period after moving to a single pharmacy benefit manager (SPBM) system in October 2022, according to a report by ODM’s Medicaid actuarial firm. The move away from traditional PBMs was an attempt to create more transparency and ensure the state was getting the best price on prescriptions. Additionally, pharmacy dispensing fees increased by 1,200 percent on average. The SPBM, run by Gainwell Technologies, contracts with 99 percent of Ohio pharmacies and is the largest in-state pharmacy network.
Ohio, West Virginia Rural Hospitals Form Integrated Network to Support Value-Based Care. Modern Healthcare reported on April 17, 2025, that twenty-six rural hospitals in Ohio and West Virginia formed the Ohio High Value Network, a clinically integrated network to support value-based care, reduce costs, and strengthen negotiating power. Managed by Cibolo Health, the network enables independent hospitals to share services, close care gaps, and pursue alternative payment models often inaccessible due to low patient volume. Leaders cite looming federal Medicaid cuts as a key driver for the collaboration.
Stay in the know on federal and state healthcare developments with HMA’s Daily Roundup.
Sign up for HMA Information Services (HMAIS) here: https://hmais.healthmanagement.com/
Industry News
Accreditation Entities to Develop Standards Around AI Usage in Healthcare. Modern Healthcare reported on April 22, 2025, that organizations such has the National Committee for Quality Assurance (NCQA) and the Utilization Review Accreditation Commission (URAC) are working toward developing standards for the use of artificial intelligence (AI) in healthcare. Both organizations have sought public comments to develop both new, standalone accreditation guidelines for AI, and guidelines within existing programs to help guide payers, providers, and health technology companies navigate the technology. NCQA expects to add AI guidelines to its health plan, utilization management, and credentialing accreditation programs, according to the organization’s Chief Transformation Officer. However, developing specific AI accreditation programs is expected to take longer.
CORRECTION: MN-based UCare Seeks to Address Financial Challenges in Medicare Advantage Offerings. On April 7, HMAIS incorrectly reported that MN-based UCare was exiting the Medicare Advantage market. According to the Health Payer Specialist report from April 7, 2025, UCare is taking additional steps to manage costs in its Medicare Advantage offering after posting a $504 million operating loss in 2024. The company is suspending broker commissions for new Medicare Advantage enrollments, effective July 1, but is not exiting this market.
RFP Calendar
Actuaries Corner
Wakely Publishes Detailed Summary of CY2026 Final Rate Announcement & CY2026 Final Part D Redesign Instructions. The Centers for Medicare & Medicaid Services (CMS) recently released the Announcement of Calendar Year (CY) 2026 Medicare Advantage (MA) Capitation Rates and Part C and Part D Payment Policies, which finalizes important changes in plan payments, risk adjustment and other financial and regulatory requirements for 2026. In tandem, CMS released the ‘Final CY 2026 Part D Redesign Program Instructions’, finalizing guidance on CY2026 treatment of changes enacted by the Inflation Reduction Act. Wakely summarizes key changes that will affect Medicare Advantage pricing for CY2026.
Discover other developments in the Wakely Wire here.
HMA News & Events
HMA Podcast
Is Medicare Ready for the Next Era of Innovation? Amy Bassano is a Managing Director at Health Management Associates and a nationally recognized Medicare policy expert. In this episode of Vital Viewpoints on Healthcare, we unpack the complexities of Medicare innovation and examine where the program is headed next. Drawing on decades of experience—including her leadership at the Center for Medicare and Medicaid Innovation—Amy breaks down what makes value-based care so complex, why scaling successful models is harder than it sounds, and how Medicare Advantage continues to reshape the healthcare landscape. She also discusses how financial incentives, regulatory constraints, and the urgent need for system-wide efficiency are shaping the next chapter of Medicare policy. This conversation offers practical insights for policymakers, providers, and advocates navigating the future of one of the nation’s most essential programs.
Leavitt Partners Webinar
Digital Health & Interoperability Policy: New Ideas to Drive Federal Government Efficiency. Thursday, April 24, 2025, 12 PM ET. Building on previous successes across multiple administrations, we have an opportunity to continue to advance patient data exchange by taking an innovative approach to federal health care technology policy. How can we more effectively advance Fast Healthcare Interoperability Resources Application Programming Interface (FHIR API)-based data exchange between payers, providers, patients, and pharmacies? What should the role of The Centers for Medicare & Medicaid Services (CMS) and Office of the National Coordinator for Health IT (ONC) be over the next decade? What federal technology policies are needed (or not needed any longer) to truly create a patient-centered health care system? How does Certified Electronic Health Record Technology (CEHRT) need to evolve to support a modern, API-based, interoperable ecosystem? Join us to explore how top payers and providers, in collaboration with Leavitt Partners, an HMA Company, crafted bold, innovative federal technology and interoperability policy recommendations for the Trump administration.
HMA Webinars
Ask HMA Experts: Medicare Town Hall. Wednesday, April 30, 2025, 12 PM ET. Join us for an open and engaging Medicare Town Hall with the experts from Health Management Associates (HMA). Whether you’re navigating Medicare Advantage policy changes, seeking actuarial insights, analyzing risk-based payment structures, or working to improve integration for Dual Eligibles and align D-SNPs, our team is here to provide actionable insights and answers. This is your opportunity to ask anything—from strategy to service delivery, coverage to compliance. We’ll have HMA professionals from across the country ready to share their perspectives and help you navigate the complexities of Medicare. Bring your questions. Share your ideas. Gain clarity.
PACE Development Best Practices for Policy Makers and Program Sponsors. Thursday, May 15, 2025, 1 PM ET. Health Management Associates (HMA) conducted a multi-state study to examine the policy decisions influencing the operation and expansion of Programs of All-Inclusive Care for the Elderly (PACE). It explored different program structures, associated advantages and challenges, and strategies to enhance efficiency while meeting regulatory requirements. This webinar will summarize our research on 10 active PACE states (CA, FL, IL, KY, LA, MA, NJ, NY, OH, and WA) that have either implemented or expanded their PACE programs between 2020 and 2024. Using state survey responses and credible third-party, publicly available data, we will showcase the outcomes of PACE program development through open and competitive RFP processes. We will also outline development timelines to demonstrate the effectiveness of each approach and highlight key insights gained during the discovery and research phase of the study.
Survey Readiness: Prepare, Respond, Succeed, a 5-part Virtual Series. Every Wednesday in April 1:00 PM to 2:30 PM ET.
In today’s complex healthcare environment, navigating the scrutiny of regulatory and accreditation bodies like The Centers for Medicare & Medicaid Services (CMS), Department of Health (DOH), The Joint Commission, and Det Norske Veritas (DNV) Healthcare is critical for the success of every hospital and health system. Unexpected surveys, triggered by recertification, validations or even complaints, can occur at any time.
HMA has partnered with the Healthcare Association of New York State (HANYS) to develop the content for Survey Readiness: Prepare, Respond, Succeed, a 5-part virtual series on Wednesdays in April from 1- 2:30pm ET. HMA’s expert faculty will also co-teach the sessions. Attendees will dive deep into organizational strategies and tactics to prepare, manage and respond to surveyors effectively – and get the essential skills to excel in survey readiness.
While some examples in the program will address issues from the New York state perspective, attendees from organizations nationwide should attend. Hospital and long-term care executive team and leaders in quality and compliance, survey coordinators, and risk management will benefit from attending.
Survey Readiness: Prepare, Respond, Succeed
Virtual Series | April 2 – 30
- April 2: Survey readiness 101: Overview and getting started
- April 9: Preparation: How to mitigate risk and prepare for upcoming surveys
- April 16: They’re here: Establishing a survey response and management protocol
- April 23: Responding to survey findings: How to develop a strong correction plan and knowing your options
- April 30: What’s next: Leveraging survey findings and strengthening organizational quality and compliance
The cost to attend this series is $475.
State hospital associations and their members can enjoy $50 off when using this code when registering: SHADISCOUNT25
To learn more and to register, visit http://hanys.org/events/survey-readiness.
NEW THIS WEEK ON HMA INFORMATION SERVICES
(Exclusive Access for HMAIS Subscribers):
HMAIS Medicaid Market Overviews, Reports, and Data
- Special Needs Plans (SNP) Enrollment by State and Plan, Mar-25 Data
- HMA Federal Health Policy Snapshot
- New Medicaid enrollment, RFP documents, and other market intelligence resources for dozens of states.
- Updated Alaska State Overview
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services.
If you’re interested in becoming an HMAIS subscriber, contact Andrea Maresca at amaresca@healthmanagement.com.