This week's roundup:
- In Focus: CMS Requests Input on Improving Medicare Advantage: Stakeholders Have a Brief Window to Offer Ideas to Inform Agency’s Initial Proposals

- Alabama Releases SMI Independent Evaluator RFP

- Arkansas Withdraws Previously Released PBM RFP To ‘Start from Scratch’

- Georgia Receives Approval for 2 Percent Rate Increase for HCBS Waivers

- Michigan Seeks Another Year to Implement SPA for Community Support Services

- Mississippi Delays Medicaid Managed Care Awards to August

- Missouri Submits Substance Use Disorder 1115 Waiver Application

- New York Attorney General Files Antitrust Lawsuit Against CVS Over 340B Program

- Ohio Releases Medicaid IV&V Services RFP

- Oregon Seeks Medicaid Coverage for Individuals Up to 200 Percent of Poverty After PHE Ends

- South Carolina to Convene Working Group on Emergency Mental Health

- National Uninsured Rate Hits a Record Low of 8 Percent

- Biden Administration May Allow Medicaid Waivers to Cover Out-of-State Abortions

- Medical Transportation Management Finalizes Acquisition of Veyo

In Focus
CMS Requests Input on Improving Medicare Advantage: Stakeholders Have a Brief Window to Offer Ideas to Inform Agency’s Initial Proposals
This week, our In Focus section reviews the request for information (RFI) on ways to strengthen the Medicare Advantage (MA) program, released by the Centers for Medicare & Medicaid Services (CMS) on July 28, 2022. CMS’s intent is to better align the MA program with the agency’s Vision for Medicare and the CMS Strategic Pillars. The agency is strongly emphasizing the importance of stakeholder comments for this process. This openness to feedback presents MA plans, providers, and other stakeholders an opportunity to inform the agency’s early thinking as it considers potential regulatory actions impacting supplemental benefits, value-based contracting arrangements, risk adjustment, prior authorization, and marketing among other issues.
The questions are grouped into five categories. Throughout each section CMS seeks to better understand operational issues and insights from past or ongoing experiences tackling health equity issues in states and communities. Below we describe several of the questions and themes within each category:
- Advance Health Equity: This extensive set of questions is intended help CMS better understand MA plans’ specific programs, screenings, benefits, and data that are components of addressing health equity and how the agency can better ensure that all MA enrollees receive the care they need. CMS also is seeking to better understand the collaborations and reimbursement arrangements between MA plans and providers that partner with community-based organizations, particularly as these arrangements become more central to efforts to address social drivers of health. The agency continues to focus on the dual eligible population, and asks specifically how it can support efforts by Special Needs Plans to provide targeted, coordinated care for enrollees.
- Expand Access: Coverage and Care: In this section CMS explores MA plans’ marketing efforts, including the tools beneficiaries use and how plans differentiate themselves to beneficiaries, as well as factors for building and changing plan networks. Additionally, CMS poses many questions about supplemental benefits, including questions about how MA plans design supplemental benefits, how they inform beneficiaries about these benefits and whether there are evaluations or data elements that are used. CMS also anticipates receiving information on how it can ensure that enrollees have access to the covered behavioral health services they need, access and use of telehealth services.
- Drive Innovation to Promote Person-Centered Care: Last year, CMS committed to ensuring that 100 percent of Medicare beneficiaries were in accountable care relationships by 2030. This will require changes for more than 30 percent of Medicare beneficiaries. To date, much of the attention around this goal has been focused on fee-for-services arrangement. With this RFI, CMS is turning its attention to value-based arrangements in MA. Specifically, it asks stakeholders about the factors driving MA plans and providers participating in value-based contracting. The agency wants to better understand the data that is crucial for value-based contracting and the experiences of MA plans in trying to align with value-based contracting in other Medicare programs/models, Medicaid, and the commercial payers. Stakeholders also have an opportunity to provide input on how CMS could better support efforts of MA plans and providers to appropriately and effectively collect, transmit, and use appropriate data as well as potential new tops of payment or service delivery models that could be tested.
- Support Affordability and Sustainability: This set of questions turns to payment and competition in the marketplace. Specifically, the agency asks for input on potential methodologies to ensure risk adjustment is accurate and sustainable. CMS also wants to understand how stakeholders are thinking about the relationship between risk adjustment and health equity and addressing social determinants of health SDOH. The agency also wants to consider specific local market barriers to entry and advantages and disadvantages in different markets.
- Engage Partners: This group of questions provides an opportunity for stakeholders to address information gaps for Medicare beneficiaries. The agency also is interested in how it could promote collaboration among MA stakeholders.
Why It Matters:
As the urgent issues with the pandemic continue to ease, CMS is turning its attention to proposals that could help refocus the Medicare program, including Medicare Advantage, to address health equity, quality, and affordability.
Stakeholders will want to carefully consider how they could use their RFI responses to shape the agency’s potential future proposals. Health plans, providers, community organizations, and vendors have an opportunity to highlight concepts, tools, and other innovations that have proven successful and scalable.
Specific concrete examples of the impact on Medicare beneficiaries would be highly valued by the agency. It will also be important to focus responses on regulatory policy changes and actions that CMS can advance with its existing authority.
HMA experts can assist stakeholders with their responses on these impactful issues including but not limited to:
- Innovations stakeholders have tried, barriers to concepts and needs they have identified, and other ideas on flexibilities for local partnerships and technology.
- Approaches to improve the MA experience for the Medicare and Medicaid dually eligible population and rural communities.
- New risk adjustment methods.
- Potential improvements to the MA quality program.
- Strategies for improving the beneficiary enrollment process.
- The value and opportunity of using technology and telehealth and how these impact the design of provider networks.
- Framing the factors and dynamics around MA plan and provider value-based contracting.
What’s Next
CMS is accepting comments on this RFI until August 31, 2022. The agency could use input it receives to develop proposals for at least the next two regular rulemaking cycles for the Medicare Advantage program, issue policy proposals outside of the normal rulemaking, or both.
HMA experts are available to provide strategic assistance with framing and developing responses as well as analysis to reinforce points and recommendations to the agency for this expedited RFI response timeline.
For questions please contact Amy Bassano, Managing Director, Medicare; Julie Faulhaber, Managing Director, Medicare and Dual Eligibles; Zach Gaumer, Principal; Andrea Maresca, Principal.
HMA Roundup
Alabama
Alabama Releases SMI Independent Evaluator RFP. The Alabama Medicaid Agency released on August 2, 2022, a request for proposals for an independent evaluator of the state’s serious mental illness (SMI) 1115 waiver demonstration programs. The SMI waiver was approved in May 2022 and is effective through May 19, 2027. Proposals are due August 26, 2022, and the contract will be effective October 1, 2022. Read More
Arkansas
Arkansas Withdraws Previously Released PBM RFP To ‘Start from Scratch’. Health Payer Specialist reported on July 27, 2022, that Arkansas is withdrawing a request for proposals (RFP) for a pharmacy benefit manager (PBM) released in May and will start again from scratch. The decision comes after consulting firm The Segal Group, which was hired to help the state write the RFP, expressed concern that it was left out of the process. Read More
Georgia
Georgia Receives Approval for 2 Percent Rate Increase for HCBS Waivers. The Georgia Department of Community Health announced on August 2, 2022, that the Centers for Medicare & Medicaid Services approved the state’s Appendix K emergency preparedness request to implement two percent rate increases for certain community waiver services for providers who have struggled during COVID-19. The rate increases, which will be effective July 1, 2022, until six months after the end of the public health emergency, apply to two 1915(c) Home and Community-Based Services (HCBS) waivers: Comprehensive Supports Waiver Program and the New Options Waiver. The state will also raise the individual service maximum annual allowances by two percent to align with the rate increases. Read More
Indiana
Senate Passes Spending Bill That Would Allocate $45 Million to Health Services for Pregnant, Postpartum Women. WHAS 11 reported on July 30, 2022, that the Indiana Senate passed a spending bill that would allocate $45 million to state agencies that provide healthcare services to pregnant and postpartum women and infants under four years old. The bill also allocates $5 million to increase adoption tax credits. A similar House bill differs on support of direct payments to taxpayers. Read More
Michigan
Michigan Seeks Another Year to Implement State Plan Amendment for Community Support Services. The Michigan Department of Health and Human Services announced on August 2, 2022, that it has asked federal regulators for another year until October 1, 2023, to implement the State Plan Amendment to transition needs-based eligibility determinations for community support services from pre-paid inpatient health plans (PIHPs) to the state of Michigan. The extension cites significant resource demands to comply with eligibility determination requirements. The federal public comment period is open until September 1. Read More
Michigan Seeks Public Input on Strengthening Medicaid Coverage Before Next Procurement. The Michigan Department of Health and Human Services announced on July 29, 2022, the launch of MIHealthyLife, an initiative to strengthen Medicaid coverage by seeking public input ahead of the next Medicaid health plan procurement. The state is seeking feedback on a variety of priorities, including providing a healthy start for children, reducing racial and ethnic health disparities, and using data to drive outcomes. Medicaid and the Healthy Michigan Plan cover approximately 2.2 million beneficiaries. Survey responses are due on August 26. Read More
Mississippi
Mississippi Delays Medicaid Managed Care Awards to August. The Mississippi Division of Medicaid announced on July 29, 2022, it has delayed announcing awards for its Medicaid managed care procurement until August. According to the request for qualifications, the state is looking for two to three managed care plans to serve its traditional Mississippi Coordinated Access Network (MississippiCAN) Medicaid program and the state Children’s Health Insurance Program (CHIP). This is the first time the state is seeking plans, which it refers to as “coordinated care organizations,” to jointly administer MississippiCAN and CHIP. Incumbents are Centene/Magnolia Health Plan, Molina Healthcare, and UnitedHealthcare.
Missouri
Missouri Submits Substance Use Disorder 1115 Waiver Application. The Missouri Department of Social Services submitted on July 15, 2022, a Section 1115 waiver application seeking federal authority to reimburse for substance use disorder (SUD) treatment provided at an institution for mental diseases with more than 16 beds. Medicaid enrollees ages 12-64 who receive full Medicaid benefits and require a residential level of care for SUD treatment will be eligible under the waiver. The state is requesting a five-year term, beginning on October 1. The federal comment period is open until September 1. Read More
Nevada
Nevada Receives $1.6 Million Grant to Address Shortage of Medicaid Oral Health Providers. KTNV reported on July 27, 2022, that the U.S. Department of Health and Human Services has awarded Nevada nearly $1.6 million over four years to help address the state’s shortage of Medicaid oral health providers. The funds will go toward development of five programs aimed at expanding the state’s provider delivery infrastructure. More than 70 percent of Nevadans live in a federally designated Health Provider Shortage Area. Implementation is anticipated to begin on September 1. Read More
New Hampshire
New Hampshire Files Lawsuit Against Pharmacy Chains for Over-Dispensing Opioids. WMUR 9 reported on July 26, 2022, that the New Hampshire Attorney General has filed a lawsuit against several pharmacy chains for over-dispensing prescription opioids and failing to alert authorities of suspicious amounts of opioid prescriptions. The lawsuit names CVS, Neighbor Care, Rite Aid, Maxi Drug North, and Walgreens. Read More
New York
Attorney General Files Antitrust Lawsuit Against CVS Over 340B Program. Crain’s New York Business reported on July 29, 2022, that the New York Attorney General filed a lawsuit claiming CVS violated antitrust laws by allegedly refusing to contract with hospitals that did not use the company’s 340B third-party administrator Wellpartner. The lawsuit is seeking monetary relief and a requirement that CVS tell hospitals they can contract with CVS even if they do not use Wellpartner. Read More
New York Proposes $325 Million Investment in HERO Program to Address Health Equity. Healthcare Innovation reported on July 27, 2022, that New York State proposed a $325 million investment in nine Health Equity Regional Organizations (HEROs) to serve as coordinating entities for partnerships between managed care organizations, hospitals, community-based providers, and other stakeholders in the state Section 1115 Medicaid waiver amendment request. The HERO program is part of a $13.5 billion request to transform the state’s Medicaid program. Read More
Ohio
Ohio Releases Medicaid IV&V Services RFP. The Ohio Department of Administrative Services released on August 1, 2022, a request for proposals (RFP) for Medicaid Independent Verification and Validation (IV&V) services. The procurement is part of Ohio’s Medicaid Enterprise System program, which will replace the state’s Medicaid management information system contract currently held by Gainwell Technologies. The IV&V contract will run through June 30, 2023, with five two-year renewal options. Proposals are due by September 9, 2022. Read More
Oregon
Oregon Seeks Medicaid Coverage for Individuals Up to 200 Percent of Poverty After PHE Ends. The Oregon Health Authority announced on August 1, 2022, it is seeking federal approval to extend Medicaid coverage to individuals up to 200 percent of poverty for 14 months after the end of the public health emergency (PHE) until the state can implement a Basic Health Plan. The request was made to the Centers for Medicare & Medicaid Services through an amendment to the Oregon Health Plan substance use disorder (SUD) 1115 waiver. Public comments on the waiver will be accepted through September 7, 2022. Read More
South Carolina
South Carolina to Convene Working Group on Emergency Mental Health. The Post and Courier reported on July 31, 2022, that the South Carolina Department of Health and Human Services will convene a working group to address the state’s lack of emergency mental health treatment and access to coverage. The effort, which is backed by $64 million from the state legislature, includes state agencies, hospitals, and others. Read More
Texas
Texas Receives Approval for State Directed Payment Programs for Fiscal 2023. The Texas Health and Human Services Commission announced on August 2, 2022, that the Centers for Medicare & Medicaid Services (CMS) approved the continuation of the state’s directed payment programs for fiscal 2023. The five approved programs are the Comprehensive Hospital Increase Reimbursement Program, Quality Incentive Payment Program, Texas Incentives for Physicians and Professional Services, Directed Payment Program for Behavioral Health Services, and Rural Access to Primary and Preventative Services Program. The programs constitute more than $7.3 billion in Medicaid payments for hospitals, nursing facilities, physician groups, behavioral health, and primary care. Read More
Utah
Utah Health, Human Services Departments Officially Merge. KSL-TV reported on July 31, 2022, that the Utah Department of Health and the Department of Human Services officially merged to create the Utah Department of Health and Human Services (DHHS). Services have moved to the new department with the exception of Medicaid eligibility policy, Medicaid Eligibility and Quality Control, and eligibility adjudications, which are now under the Department of Workforce Services. The Utah DHHS is the largest agency in the state, with a total annual budget of $1.32 billion. Tracy Gruber, who was named executive director of the Utah Department of Human Services in January 2021, serves as executive director of the combined agency. Read More
National
National Uninsured Rate Hits a Record Low of 8 Percent. Fierce Healthcare reported on August 2, 2022, that the U.S. uninsured rate hit a record low eight percent in the first quarter of 2022, according to the U.S. Department of Health and Human Services. About 5.2 million individuals have gained coverage since 2020, with individuals making below 100 percent of the federal poverty level (FPL) and between 200 and 400 percent FPL seeing the biggest increase in coverage. The report cites enhanced Exchange subsidies and continuous enrollment during the public health emergency as contributors to the low rate. Read More
Biden Administration May Allow Medicaid Waivers to Cover Out-of-State Abortions. The Hill reported on August 3, 2022, that President Biden ordered federal regulators to consider allowing Medicaid waivers that cover expenses for women who cross state lines for an abortion. Under the executive order, states where abortion is legal would apply for a section 1115 waiver to cover reproductive healthcare services for out-of-state residents. Read More
NCQA Adds Race, Gender-Relevant Care to 2023 HEDIS Measures. Health Payer Intelligence reported on August 1, 2022, that the National Committee for Quality Assurance (NCQA) added race and ethnicity data, social determinants of health screening measures, and gender-relevant care measures to its 2023 healthcare quality rankings. The 2023 Healthcare Effectiveness Data and Information Set (HEDIS) will also add measures of pediatric dental services, diabetes care, and prescription of benzodiazepines for seniors. Read More
HHS Announces New Medicaid Health Home Benefit for Children With Medically Complex Conditions. The U.S. Department of Health and Human Services (HHS) announced on August 1, 2022, an optional Medicaid health home benefit for children with medically complex conditions, including person-centered care management, care coordination, and support. States with approved Medicaid state plan amendments (SPAs) to cover the new benefit will receive a 15 percentage point increase in federal matching for their expenditures on health home services during the first two fiscal year quarters that the SPA is in effect. States will have the option to offer the health home benefit beginning on October 1. Read More
CMS to Release Medicare Advantage RFI. The Centers for Medicare & Medicaid Services (CMS) announced on July 28, 2022, it will release a request for information (RFI) on the Medicare Advantage (MA) program, regarding health equity, beneficiary access to health services, innovation in payment and care delivery, and competition. The RFI will be open for public comment on August 1. Read More
Biden Administration Announces Funding Opportunities to Address Teenage Mental Health Crisis. The Biden Administration announced on July 29, 2022, that it will award $300 million to expand mental health services in schools, including $140 million to increase the number of mental health professionals on staff. Read More
Medicaid, CHIP Enrollment Tops 88 Million, Medicare Tops 64 Million as of April 2022. The Centers for Medicare & Medicaid Services (CMS) released on July 28, 2022, that Medicaid and Children’s Health Insurance Program (CHIP) enrollment was nearly 88.3 million as of April 2022, up 88,000 from March 2022. Medicare enrollment was 64.4 million, with 29.6 million in a Medicare Advantage plan. More than 12 million were dually eligible and counted in the enrollment totals for both programs. Read More
CMS Releases Final Medicare Inpatient, Long Term Care Prospective Payment System Rule. The Centers for Medicare & Medicaid Services released on August 1, 2022, the final Medicare prospective payment system rule for inpatient and long-term care hospitals. The rule includes a 4.3 percent increase in Medicare inpatient payment rates for hospitals that participate in the inpatient quality reporting (IQR) program and utilize electronic health records and an increase of approximately 2.4 percent for long term care payments. The final rule also adds three health equity measures to the IQR program and introduces a birthing-friendly designation for hospitals committed to reducing maternal morbidity and mortality. Read More
CMS Increases Medicare Payments to Nursing Homes by 2.7 Percent in Fiscal 2023. Modern Healthcare reported on July 29, 2022, that nursing homes will receive a net 2.7 percent or $904 million increase in Medicare payments during fiscal 2023 under a final rule issued by the Centers for Medicare & Medicaid Services (CMS). In April, CMS proposed cutting Medicare Part A payments to nursing homes, but the agency changed course because providers are still struggling with the impact of COVID-19. The final rule also caps annual wage index adjustments for nursing homes so payments will not decrease more than five percent year to year. Read More
CMS Failed to Recoup $226 Million in Medicare Overpayments, Audit Finds. Modern Healthcare reported on July 28, 2022, that the Centers for Medicare & Medicaid Services (CMS) failed to recoup $226 million out of $498 million in Medicare overpayments, according to an audit from the Office of Inspector General. The audit also found that CMS failed to complete prior recommendations intended to limit overpayments and improve claims tracking. The audit looked at 148 Medicare audit reports issued from October 1, 2014, through December 31, 2016. Read More
House Passes Bill to Extend Medicare Reimbursement Flexibilities for Telehealth Through 2024. Modern Healthcare reported on June 27, 2022, that the U.S. House passed legislation to extend Medicare reimbursement flexibilities for telehealth through 2024. Read More
Industry News
Medical Transportation Management Finalizes Acquisition of Veyo. Medical Transportation Management (MTM) announced on August 2, 2022, that it had completed the acquisition of Veyo, a non-emergency medical transportation provider. MTM and Veyo will serve a combined 15.4 million members in 31 states and generate roughly $1 billion in revenues. Read More
Stepping Stones Group Acquires Center for Behavioral, Educational, and Social Therapies. Stepping Stones Group announced on July 28, 2022, the acquisition of the Center for Behavioral, Educational, and Social Therapies (CBEST), a Los Angeles-based provider of applied behavior analysis services. CBEST founder Shah Bahador will assume the role of Stepping Stones clinical director. Read More
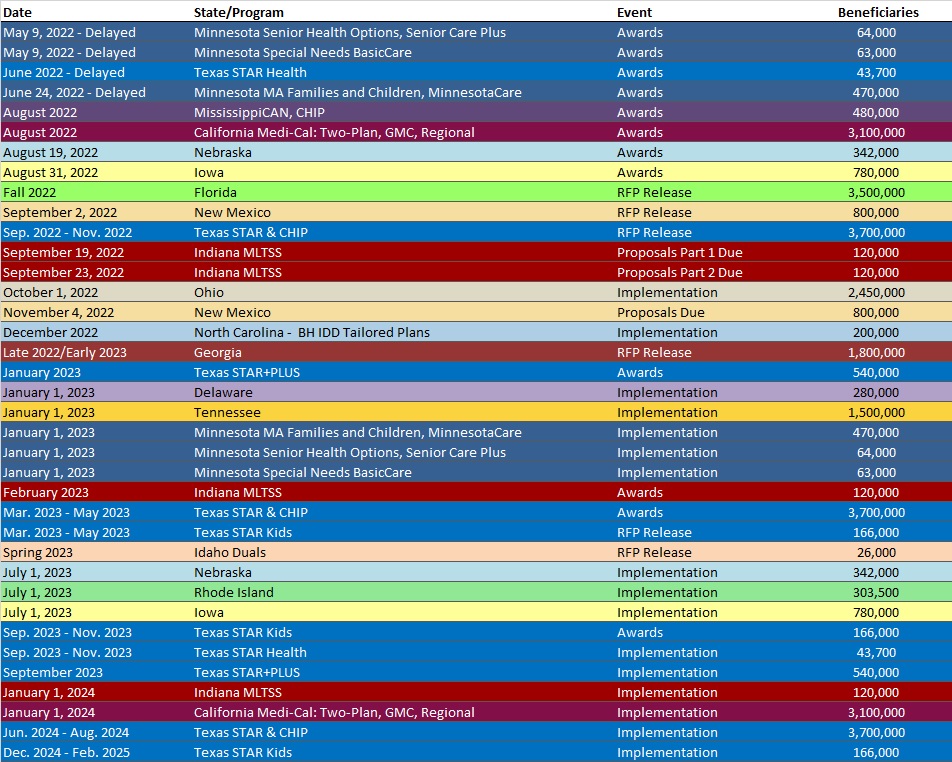
RFP Calendar
HMA News & Events
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Maryland Medicaid Managed Care Enrollment Is Up 2.1%, Apr-22 Data
- Pennsylvania Medicaid Managed Care Enrollment is Up 2.6%, Apr-22 Data
Medicaid Financials and Utilization Data:
- MLRs Average 84.2% at Florida MMA MCOs, 2021 Data
- MLRs Average 81.8% at Georgia Medicaid MCOs, 2021 Data
- MLRs Average 88.3% at Hawaii Medicaid MCOs, 2021 Data
- MLRs at Indiana Medicaid MCOs Average 91.2%, 2021 Data
- MLRs at Iowa Medicaid MCOs Average 85.4%, 2021 Data
- MLRs at Kansas Medicaid MCOs Average 83.7%, 2021 Data
- MLRs at Kentucky Medicaid MCOs Average 88%, 2021 Data
- MLRs at Louisiana Medicaid MCOs Average 87.9%, 2021 Data
- MLRs Average 87% at Maryland Medicaid MCOs, 2021 Data
- MLRs Average 81.8% at Michigan Medicaid MCOs, 2021 Data
- MLRs Average 89.1% at Minnesota Medicaid MCOs, 2021 Data
- MLRs Average 78.8% at Missouri Medicaid MCOs, 2021 Data
- MLRs Average 86.2% at Nebraska Medicaid MCOs, 2021 Data
- MLRs Average 86.4% at New Hampshire Medicaid MCOs, 2021 Data
- MLRs Average 84.3% at New Jersey Medicaid MCOs, 2021 Data
- MLRs Average 84.3% at Ohio Medicaid MCOs, 2021 Data
- MLRs Average 92.1% at Puerto Rico Medicaid MCOs, 2021 Data
- MLRs Average 88.7% at Rhode Island Medicaid MCOs, 2021 Data
- MLRs Average 79.5% at Tennessee Medicaid MCOs, 2021 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Alabama SMI Program Independent Evaluator RFP, Aug-22
- Georgia Medicaid Redeterminations Solution RFQ, Aug-22
- Mississippi MississippiCAN and CHIP RFQ and Amendments, 2021-22
- Ohio Medicaid Independent Verification and Validation Services RFP, Aug-22
Medicaid Program Reports, Data and Updates:
- Missouri Section 1115 Substance Use Disorder Waiver Application, Jul-22
- Ohio Medicaid Budget Variance Report, 2017-21
- Oregon Health Plan Substance Use Disorder 1115 Waiver Documents, 2021-22
- South Dakota Medicaid Advisory Committee Meeting Materials, May-22
- Washington 1115 Medicaid Transformation Waiver Documents, 2015-22
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.