This week's roundup:
- In Focus: Texas Releases STAR & CHIP Managed Care Services RFP

- California to Sanction 22 Medi-Cal Plans for Poor Quality Ratings

- California Governor Awards $480.5 Million in Grants for Youth Behavioral Health Infrastructure

- Connecticut Governor to Appoint Andrea Barton Reeves Commissioner of Social Services

- Massachusetts Medicaid Secretary To Step Down

- Minnesota Judge Blocks Managed Care Plan from Expanding Board of Directors

- Missouri, Mississippi, Montana, Wyoming Are Expected to Extend Medicaid Postpartum Eligibility in 2023

- Nevada Releases External Quality Review Organization RFP

- North Carolina Faces Lawsuit for Foster Children in Residential Psychiatric Treatment Facilities

- Wyoming Requests $22 Million to Increase Nursing Home Medicaid Reimbursement Rates in 2024

- CMS Rule Would Increase Availability of Standardized Exchange Plans

- MedPAC Draft Recommendations Call for Medicare Payment Increases for Hospitals, Physicians in 2024

- Exchange Enrollment Rises 18 Percent in First Five Weeks of Open Enrollment

- SCAN Group, CareOregon to Merge as HealthRight Group

- Centene Names New President, Chief Operating Officer, Other Leadership Changes

In Focus
Texas Releases STAR & CHIP Managed Care Services RFP
This week, our In Focus section reviews the State of Texas Access Reform (STAR), Children’s Health Insurance Program (CHIP), and Healthy Texas Women (HTW) Medicaid managed care request for proposals (RFP) released by the Texas Health and Human Services Commission (HHSC) on December 7, 2022. Medicaid managed care organizations (MCOs) will serve over 4.6 million members. Prior STAR & CHIP program contracts were valued at roughly $9.7 billion annually, with new contracts to be worth more.
Background
Texas is currently in the process of rebidding all of its Medicaid managed care programs. A former STAR & CHIP RFP was cancelled in March 2020.
STAR is Texas’ traditional Medicaid program. Under the STAR program, MCOs will provide preventive, primary, acute care, behavioral health (including mental health and substance-use disorder counseling and treatment), Non-Emergency Medical Transportation (NEMT), and pharmacy services to eligible pregnant women, newborns, children, and parents with limited income.
CHIP is the state-federal jointly funded program covering children whose families who earn too much to qualify for Medicaid but cannot afford private insurance. In Texas, CHIP contracts also include the CHIP Perinatal Program covering pregnant women who are ineligible for Medicaid due to income or immigration status to receive prenatal care for their unborn children. Once born, newborns receive 12 months of continuous coverage.
The HTW program provides family planning services, family planning-related services, and other preconception women’s health services. The HTW program was originally a fee-for-service program until the Centers for Medicare & Medicaid Services (CMS) approved a Section 1115 waiver demonstration in January 2020. Texas is currently waiting on CMS approval for a waiver amendment to also add HTW Plus, an enhanced postpartum benefits package, into Medicaid managed care.
RFP
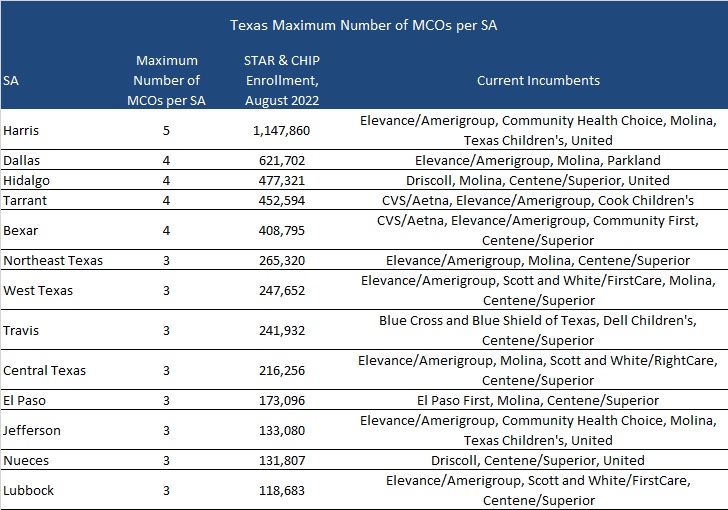
HHSC intends to award at least three contracts for each service area (SA). The maximum number of MCOs that will be awarded in the new procurement for each SA is shown below.
As of August 2022, STAR enrollment was 4.56 million and CHIP enrollment was over 97,000.
Timeline
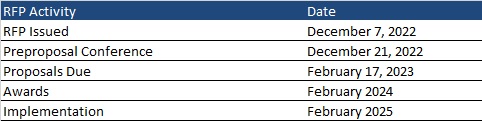
A preproposal conference will be held on December 21, 2022. While optional, the conference is recommended and will include training on the completion of the Historically Underutilized Business (HUB) Subcontracting Plan. Proposals will be due February 17, 2023, with awards anticipated in February 2024. Implementation is expected February 2025. Contracts will run for six years, with three two-year renewal options, not to exceed a total contract term of 12 years.
Evaluation
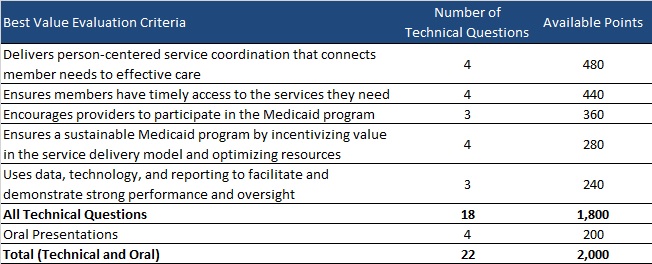
MCOs will be scored out of 2,000 points as shown below. HHSC will recommend contract awards in SAs based on MCOs’ final weighted scores and will take consideration of MCOs’ ranking of SAs by preference.
Each MCO can be awarded contracts in up to seven SAs. However, HHSC may choose to award more per MCO if the SA has not reached a maximum number of MCOs.
Link to RFP
HMA Roundup
Alabama
Alabama Uninsured Rate Individuals Could Rise 16 Percent After End of Public Health Emergency. AL.com reported on December 10, 2022, that approximately 61,000 Alabama Medicaid enrollees could lose health coverage when the federal public health emergency (PHE) expires, according to a report from Robert Wood Johnson Foundation and Urban Institute. The disenrollments could lead to a 16 percent increase in the state’s uninsured rate. Read More
California
California to Sanction 22 Medi-Cal Plans for Poor Quality Ratings. The California Department of Health Care Services (DHCS) announced on December 13, 2022, that it will sanction 22 Medi-Cal plans for nearly $2.3 million for falling below Minimum Performance Levels for immunization rates, well-infant and well-child visits, breast cancer screenings, and cervical cancer screenings for calendar year 2021. Plans must submit a revised comprehensive quality strategy and work with DHCS to address health disparities by January 31, 2023. Read More
California Healthcare Organizations Settle False Claims Act Lawsuits for $22.5 Million. Fierce Healthcare reported on December 9, 2022, that Dignity Health and two subsidiaries of Tenet Healthcare will pay a combined $22.5 million to California to settle federal and state False Claims Act lawsuits. The lawsuits claim that Tenet’s Twin Cities Community Hospital and Sierra Vista Regional Medical Center overbilled the Medicaid program between January 2014 through April 2016, while Dignity Health submitted claims for “enhanced services” from February 2015 through June 2016. Read More
California Governor Awards $480.5 Million in Grants for Youth Behavioral Health Infrastructure. California Governor Gavin Newsom announced on December 7, 2022, that California awarded grants totaling $480.5 million across 54 programs to improve the state’s behavioral health infrastructure for children and youth. The programs include construction and expansion of facilities for children’s mental health and substance use disorder treatment. The awards are round four of a six-part, $2.1 billion Behavioral Health Continuum Infrastructure Program. Read More
Colorado
Colorado, Florida, New Hampshire, New Mexico Seek Federal Approval to Import Pharmaceuticals from Canada. Kaiser Health News reported on December 14, 2022, that Colorado joined Florida, New Hampshire, and New Mexico in requesting federal approval to import prescriptions from Canada. The Biden Administration has previously expressed support for these proposals but has yet to approve any. Read More
Connecticut
Connecticut Governor to Appoint Andrea Barton Reeves Commissioner of Social Services. Connecticut Governor Ned Lamont announced on December 7, 2022, plans to appoint Andrea Barton Reeves commissioner of the state Department of Social Services (DSS) which oversees the state’s Medicaid and Children’s Health Insurance Program. Current commissioner Deidre Gifford, MD, will be appointed executive director of the Connecticut Office of Health Strategy. Barton Reeves is currently chief executive of the Connecticut Paid Leave Authority. Read More
Florida
Florida Stakeholders Want to See Governor’s Plan for Medicaid Redeterminations. The Tampa Bay Times reported on December 8, 2022, that a coalition of Florida-based stakeholders urged Governor Ron DeSantis to release the state’s plan for ensuring eligible individuals do not lose Medicaid coverage at the end of the public health emergency (PHE), according to a letter signed by 40 organizations. Officials from the Florida Department of Children and Families stated that they are working with the state Agency for Health Care Administration and other stakeholders to ensure the state is prepared for the PHE’s end. Read More
Massachusetts
Massachusetts Medicaid Secretary To Step Down. The Massachusetts Executive Office of Health and Human Services announced on December 13, 2022, that Amanda Cassel Kraft, assistant secretary for MassHealth, the state’s Medicaid program, will step down effective January 2, 2023. Mike Levine, the state’s deputy Medicaid director, will become acting assistant secretary. Read More
Minnesota
Minnesota Judge Blocks Managed Care Plan from Expanding Board of Directors. The Star Tribune reported on December 8, 2022, that Hennepin County Judge Laurie Miller temporarily blocked Minnesota Medicaid managed care plan UCare from expanding its board of directors. The University of Minnesota, which created the health plan and appoints eight of its 15 board members, asked for the injunction in a lawsuit arguing the move would marginalize its role in the plan and threaten its right to receive assets if the plan was ever shut down. Read More
Mississippi
Mississippi Contracts with Verato to Implement New Medicaid Data Management Platform. Verato announced on December 13, 2022, it will partner with the state of Mississippi’s Division of Medicaid and the Mississippi Department of Human Services to implement the state’s new healthcare master data management platform. The platform will establish a unique identifier for each Medicaid beneficiary with the goal of better organizing beneficiary data across the agency. Read More
Mississippi House Speaker Opposes Medicaid Postpartum Coverage Extension. The Daily Journal reported on December 8, 2022, that Mississippi House Speaker Phillip Gunn (R-Clinton) stated his opposition to extending postpartum Medicaid coverage to one year. The state currently offers coverage up to 60 days postpartum. Read More
Missouri
Missouri, Mississippi, Montana, Wyoming Are Expected to Extend Medicaid Postpartum Eligibility in 2023. Kaiser Health News reported on December 8, 2022, that legislators in Montana, Wyoming, Missouri, and Mississippi are considering proposals to extend Medicaid postpartum coverage to 12 months. Montana Governor Greg Gianforte included provisions to extend coverage in the proposed state budget, and a Wyoming legislative committee voted to introduce a coverage extension bill in the 2023 legislative session. Lawmakers in Missouri and Mississippi are expected to introduce similar legislation in 2023. Read More
Nevada
Nevada Releases External Quality Review Organization RFP. The Nevada Division of Health Care Finance and Policy released on December 7, 2022, a request for proposals (RFP) for an external quality review organization (EQRO) for the state’s Medicaid managed care organizations and prepaid ambulatory health plans. The state plans to award one contract for a period of four years, beginning on July 1, 2023, with two, one-year renewal options. The current EQRO contract is held by Health Services Advisory Group. Proposals are due by February 9, 2023. Read More
New Hampshire
New Hampshire Submits 1115 Medicaid Waiver Amendment Request to Cover Prosthodontics. The Centers for Medicare & Medicaid Services (CMS) announced on December 8, 2022, that New Hampshire submitted an amendment to its Substance Use Disorder, Serious Mental Illness, and Serious Emotional Disturbance Treatment Recovery and Access Section 1115 demonstration to cover removable prosthodontics for Medicaid enrollees age 21 and over in nursing facilities. Public comments will be accepted through January 6, 2023. Read More
New Mexico
New Mexico Medicaid Faces Provider Shortages, Low Reimbursement Rates, Report Finds. The Santa Fe New Mexican reported on December 13, 2022, that New Mexico’s Medicaid program faces a shortage of providers, low provider reimbursement rates, and outdated contact information for enrollees, according to a report from Legislative Finance Committee program evaluator Ryan Tolman. The report recommended that the state develop a comprehensive network adequacy assessment, appropriate funds for provider rate increases, and mandate managed care organizations update provider directories. Read More
New Mexico Could Disenroll Up To 100,000 Medicaid Enrollees After Public Health Emergency Ends. Source New Mexico reported on December 13, 2022, that 85,000 to 100,000 New Mexicans could lose Medicaid coverage at the end of the public health emergency, acting Department of Health Secretary David Scrase told the state Legislative Finance Committee. New Mexico has the highest proportion of Medicaid and Children’s Health Insurance Plan enrollees nationwide at 34 percent of the population. Read More
North Carolina
North Carolina Faces Lawsuit for Foster Children in Residential Psychiatric Treatment Facilities. North Carolina Health News reported on December 8, 2022, that Disability Rights North Carolina and the North Carolina State Conference of the NAACP have filed a joint federal lawsuit, claiming that the state is “warehousing” foster children of color with disabilities in “prison-like settings” in residential psychiatric treatment facilities. The lawsuit argues the children should have access to home and community-based settings. Read More
Ohio
Ohio May Be Spending Millions on Ineligible Medicaid Members, Audit Finds. The Ohio Auditor of State Keith Faber announced on December 13, 2022, that the Ohio Department of Medicaid did not address 59 percent of alerts from the Public Assistance Reporting Information System, which tracks if individuals are enrolled in Medicaid and other state benefits in multiple states, since July 2022. The state’s inaction on these alerts could be costing between $5.3 million and $24.5 million annually, according to the report. Read More
South Dakota
South Dakota Looks to Implement Medicaid Expansion As Required in July 2023. The Mitchell Daily Republic reported on December 9, 2022, that South Dakota Governor Kristi Noem and state lawmakers are looking to implement Medicaid expansion by July 1, 2023, as mandated by a recently passed constitutional amendment. The state must outline the program in an amended Medicaid state plan to the Centers for Medicare & Medicaid Services by March 1, 2023. A projected 52,000 individuals will be eligible. Read More
West Virginia
West Virginia Providers To Receive Funding from Aetna for Children with Serious Emotional Disorders. CVS/Aetna Better Health of West Virginia announced on December 8, 2022, that it would provide $6.1 million to 18 health care providers in the state to expand community-based waiver services for Children with Serious Emotional Disorders. The funding will assist children in residential treatment facilities transition to home and community-based settings. Aetna holds the single Specialized Managed Care for Children and Youth contract in West Virginia. Read More
Wisconsin
Wisconsin Recovers $106 Million Under Medicaid Birth Cost Recover Policy, Report Finds. The Wisconsin Examiner reported on December 14, 2022, that Wisconsin has won almost 76,000 legal judgements, totaling $106 million, to recover costs paid by Medicaid under the state’s birth cost recovery policy, according to a report by ABC for Health. The policy allows the state to clawback costs paid by Medicaid from unmarried parents in cases where the mother is enrolled in Medicaid while pregnant, but the child’s other parent has the resources to cover all or part of the costs. The report says the policy disproportionately affects Black families. Read More
Wyoming
Wyoming Requests $22 Million to Increase Nursing Home Medicaid Reimbursement Rates in 2024. The Casper Star Tribune reported on December 14, 2022, that the Wyoming Department of Health is seeking to boost Medicaid reimbursement rates for nursing homes through a $22 million budget request for fiscal 2024. The department is requesting a total of almost $118 million for the year. Read More
National
Congressional Democrats Express Concerns About ACO REACH Program Participants. CQ News reported on December 13, 2022, that 21 Democratic legislators have expressed concerned over nine participants selected by the Centers for Medicare and Medicaid Services (CMS) for the Accountable Care Organization Realizing Equity, Access, and Community Health (ACO REACH) program, according to a letter sent to CMS. The legislators say these participants have a history of Medicare, Medicaid, and Veterans Affairs fraud and should be prevented from joining the program. Read More
National Council on Disability Calls for Mandatory Medicaid HCBS Coverage. Disability Scoop reported on December 13, 2022, that the National Council on Disability (NCD) is calling for mandatory Medicaid coverage of home and community based services (HCBS), noting that more than 820,000 individuals are currently on HCBS waiting lists nationwide. According to an NCD report, 14 million Americans need community-based services, with individuals under age 30 accounting for the fastest growing group of nursing home residents. Read More
CMS Rule Would Increase Availability of Standardized Exchange Plans. Modern Healthcare reported on December 12, 2022, that the Centers for Medicare & Medicaid Services (CMS) proposed a rule that would increase the availability of standardized Exchange plans and limit the number of non-standardized plans. The rule would also require insurers to increase substance use disorder and mental health coverage, establish a special enrollment period for individuals who lose coverage at the end of the public health emergency, and decrease state and federal Exchange user fees. Read More
CMS Releases Resource for Transitioning Children Between Medicaid, CHIP. The Centers for Medicare & Medicaid Services (CMS) released on December 12, 2022, a slide deck outlining the requirements for transitioning children between Medicaid and the Children’s Health Insurance Program (CHIP). The information is designed to help states during the unwinding of the public health emergency. Read More
MedPAC Draft Recommendations Call for Medicare Payment Increases for Hospitals, Physicians in 2024. Axios reported on December 12, 2022, that the Medicare Payment Advisory Commission (MedPAC) has drafted recommendations calling for Congress to increase 2024 Medicare payment rates for hospitals by one percent more than required by law. MedPAC is also likely to recommended 2024 physician fee schedule increases for clinicians. However, the draft calls for a three percent cut to base payments for skilled nursing facilities and a seven percent cut for home health. Read More
More Than 2,000 Pharmacies To Rejoin TRICARE Network. The Navy Times reported on December 8, 2022, that more than 2,000 pharmacies will rejoin TRICARE’s pharmacy network, according to pharmacy benefit manager Cigna/Express Scripts. About 15,000 pharmacies had left the network citing low reimbursement rates. A letter from the National Community Pharmacists Association indicates that the pharmacies rejoining will receive rates that are virtually identical to those originally proposed by Cigna/Express Scripts. Read More
Exchange Enrollment Rises 18 Percent in First Five Weeks of Open Enrollment. Fierce Healthcare reported on December 7, 2022, that 5.5 million individuals have enrolled in Exchange plans in the first five weeks of open enrollment, an 18 percent increase from 2021, according to figures from the Centers for Medicare & Medicaid Services. Of the total, 1.2 million have enrolled in Exchange plans for the first time. Read More
Pharmacy Groups Urge TRICARE PBM to Reinstate Pharmacies Dropped From Network. Fierce Healthcare reported on December 7, 2022, that pharmacy groups urged pharmacy benefit manager Cigna/Express Scripts to reinstate nearly 15,000 pharmacies dropped from the TRICARE network in October. In a letter to Cigna/Express Scripts, pharmacy groups said the move has created confusion and is already impacting access to some 400,000 beneficiaries. Read More
Industry News
SCAN Group, CareOregon to Merge as HealthRight Group. Oregon-based CareOregon and California-based SCAN Group announced on December 14, 2022, a definitive agreement to merge under the name HealthRight Group. The combined not-for-profit organization will serve almost 800,000 members through Medicare and Medicaid managed care plans with a combined revenue of $6.8 billion. SCAN Group chief executive Sachin Jain, MD will become the chief executive of HealthRight. Chief executive and president of CareOregon Eric C. Hunter will serve as president of HealthRight’s Medicaid Division and will continue in his current role. The transaction is expected to close in 2023, pending regulatory approval. Read More
Centene Names New President, Chief Operating Officer, Other Leadership Changes. Centene Corporation announced on December 14, 2022, that Ken Fasola will serve as the new president of Centene. Fasola, who is currently the executive vice president (EVP) of Health Care Enterprises, will become responsible for Centene’s health plans, all lines of business, and core operations. EVP of markets Dave Thomas will be named the chief executive of Markets and Medicaid. Additionally, Jim Murray, EVP, chief transformation officer, will be appointed EVP, chief operating officer, and president, and chief operating officer Brent Layton will be transitioned to senior advisor to the chief executive. Read More
The Care Team Acquires 1st Care Home Health and Care Hospice. Private equity firm Revelstoke Capital Partners announced on December 14, 2022, that its portfolio company The Care Team has acquired 1st Care Home Health and Care Hospice, a home health and hospice provider based in Indiana. Members of the 1st Care leadership team will serve in management roles with The Care Team. Read More
Oscar Health Pauses New Enrollment in FL Exchange Plan. Modern Healthcare reported on December 12, 2022, that Oscar Health has paused new enrollment in its Florida Exchange plan to “ensure that our projected membership does not exceed the company’s targets for 2023,” a company spokesperson said. Existing enrollees are able to renew coverage through the end of the open enrollment period. Read More
MBF Healthcare Partners II Acquires Austin Connect to Wellness. MBF Healthcare Partners II announced on December 12, 2022, the acquisition of Austin Connect to Wellness/ABA Connect, a provider of applied behavior analysis therapy for children with Autism Spectrum Disorder in six facilities in Austin and Houston, TX. MBF Healthcare Partners II is a private equity fund based in Florida. Read More
Michigan Medicine to Acquire Sparrow Health. Modern Healthcare/Crain’s Detroit Business reported on December 8, 2022, that Michigan Medicine, the parent company of the University of Michigan (UM) Hospital, is expected to approve a plan to acquire Sparrow Health, a health system with 6 hospitals and 56 ambulatory facilities in the state. The UM Board of Regents must vote to approve the deal before the health systems can merge. Read More
Pinnacle Treatment Centers Acquires MBA Wellness Center. Pinnacle Treatment Centers announced on December 8, 2022, the acquisition of MBA Wellness Center, an outpatient opioid addiction treatment program in Georgia. MBA Wellness will operate under the HealthQwest brand, a subsidiary of Pinnacle. Read More
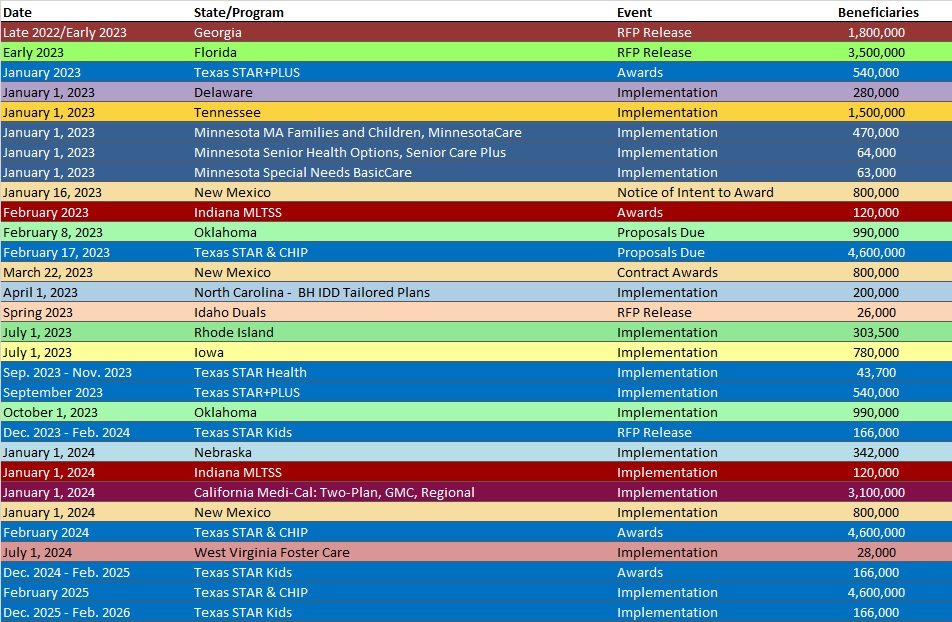
RFP Calendar
HMA News & Events
WAKELY, AN HMA COMPANY, WHITE PAPER
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Kentucky Medicaid Managed Care Enrollment is Up 5%, Oct-22 Data
- Illinois Medicaid Managed Care Enrollment is Up 3%, Oct-22 Data
- Illinois Dual Demo Enrollment is Down 3.4%, Oct-22 Data
- Indiana Medicaid Managed Care Enrollment Is Up 8.4%, Oct-22 Data
- Maryland Medicaid Managed Care Enrollment Is Up 4.6%, Oct-22 Data
- Mississippi Medicaid Managed Care Enrollment is Down 13.9%, Oct-22 Data
- Ohio Medicaid Managed Care Enrollment is Up 0.5%, Sep-22 Data
- Pennsylvania Medicaid Managed Care Enrollment is Up 4.9%, Sep-22 Data
- Texas Dual Demo Enrollment is 34,336, Aug-22 Data
- Washington Medicaid Managed Care Enrollment is Up 4.7%, Oct-22 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Illinois Dental FFS RFP (Canceled), 2022
- Oklahoma SoonerSelect Managed Care RFP, Dec-22
- Nevada External Quality Review Organization RFP, Dec-22
- Washington Medicaid Managed Care Model Contracts, 2022
Medicaid Program Reports, Data, and Updates:
- California Department of Managed Health Care Annual Reports, 2016-21
- California Enhancing Quality for Medi-Cal Members Report, Dec-22
- Michigan Behavioral Health Comparison Rate Development, SFY 2023
- Michigan Department of Health and Human Services Annual Report of Key Program Statistics, FY 2013-22
- Michigan Health Link Financial Alignment Initiative Evaluation Reports, 2019-22
- New Mexico Medicaid Program Evaluation Legislative Report, Dec-22
- Texas Medicaid Telemedicine, Telehealth, and Home Telemonitoring Services Report, 2016-22
- Texas VBP and Quality Improvement Committee Recommendations to Legislature, Dec-22
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.