This week's roundup:
- In Focus: Behavioral Health Crises Drive Bipartisan Action in Congress

- Kansas to Delay Reprocurement of Medicaid Contracts After Legislature Overrides Veto

- North Carolina Senate Republicans to Propose Medicaid Expansion

- Oklahoma Legislature Approves Move to Medicaid Managed Care

- Rhode Island Governor Proposes MMIS Modernization Project in Fiscal 2023 Budget

- Virginia Director of the Department of Medical Assistance Services Steps Down

- Washington Appoints Charissa Fotinos as Medicaid Director

- West Virginia Lawmakers Evaluate DHHR Ahead of Possible Reorganization

- U.S. Senators Introduce Bipartisan Legislation to Integrate Care for Dual Eligibles

- Enhanced Healthcare Partners Invests in Howard J. Chudler & Associates

In Focus
Behavioral Health Crises Drive Bipartisan Action in Congress
Agreement about the severity of the nation’s mental health and substance use disorder crises is rising above the partisan politics in Congress. In fact, these are among a handful of issues driving work on bipartisan legislation across all the key House and Senate committees with jurisdiction over behavioral health programs and policies this year.
On May 18, the U.S. House of Representatives Energy and Commerce Committee unanimously approved the “Restoring Hope for Mental Health and Well-Being Act of 2022” (H.R. 7666). This legislation incorporates a collection of bipartisan bills to update and reauthorize over 30 Substance Abuse and Mental Health Services Administration (SAMHSA) and Health Resources and Services Administration (HRSA) programs addressing the mental health and substance use disorder (SUD) crisis. The bill also advances initiatives to strengthen the 9-8-8 National Suicide Prevention Lifeline implementation efforts, invest in the crisis response continuum of care, and support strategic opioid crisis response plans among numerous other policies. Energy and Commerce is one of several House committees planning to advance behavioral health bills this year.
U.S. Senate committee leaders have been similarly engaged in developing bipartisan proposals to address mental health and substance use disorders. Senate Health, Education, Labor and Pensions (HELP) and Finance committee leaders are expected to reveal their proposals as soon as this summer. The Finance Committee’s proposal will focus on Medicare, Medicaid, and Children’s Health Insurance Program (CHIP) policies and could reflect findings from the committee’s report, “Mental Health Care in the United States: The Case for Federal Action.” Similarly, HELP members Sens. Chris Murphy (D-CT) and Bill Cassidy (R-LA) introduced the Mental Health Reform Reauthorization Act to extend several expiring mental health programs, which could be incorporated in that Committee’s comprehensive proposal. Across committees, there has been an interest in strengthening parity, supporting integration of primary and behavioral health care, increasing access to youth mental health screenings, scheduling fentanyl analogues, and easing requirements for prescribing Medication Assisted Treatment.
What To Expect
Congressional leaders have consistently expressed their desire to advance bipartisan legislation to address the urgent needs and gaps in the mental health and SUD care delivery systems, as well as support education and research. While these are key areas to watch, the diminishing number of legislative days on the congressional calendar and climate surrounding November’s mid-term elections create uncertainty for the timing and scope of Congress’ work. It remains to be seen whether a package of health care proposals, such as reauthorization of the U.S. Food and Drug Administration’s user fee programs, the Cures 2.0 legislation to advance biomedical research, mental health and substance use disorder legislation, and the PREVENT Act could be sent to President Biden’s desk before the end of September.
HMA companies are supporting clients impacted by the policy changes being discussed and the program funding addressed in these legislative proposals. Understanding the landscape for federal change allows state and local governments and stakeholders to plan for and shape these opportunities. For more information, please contact Andrea Maresca, Principal, Federal Policy, HMA; Matt Gallivan, Director, Leavitt Partners; and Laura Pence, Director, Leavitt Partners.
HMA Roundup
Florida
Florida Organization Seeks Full Federal Appeals Court Review of Motion to Dismiss False Claims Act Lawsuit. Health News Florida reported on May 18, 2022, that the Florida Birth-Related Neurological Injury Compensation Association (NICA) filed a motion requesting that the full 11th U.S. Circuit Court of Appeals consider whether NICA has immunity against a false claims act lawsuit alleging it shifted costs to Florida’s Medicaid program by considering itself payer of last resort. Previously, a panel of three federal Appeals Court judges rejected NICA’s motion to dismiss the lawsuit. Read More
Kansas
Kansas to Delay Reprocurement of Medicaid Contracts After Legislature Overrides Veto. The Kansas Reflector reported on May 23, 2022, that the Kansas legislature overrode Governor Laura Kelly’s veto of a bill that would delay the process of procuring new Medicaid managed care contracts until January 2023. This delay will ensure that the procurement takes place after the gubernatorial election in November. The contracts are worth approximately $3.9 billion. Read More
New York
New York Nursing Home Group Files Lawsuit to Block Staffing Minimums, Resident Spending Legislation. The Times Herald-Record reported on May 25, 2022, that nursing home trade group LeadingAge New York filed a lawsuit in state supreme court aimed at overturning a law governing nursing home staffing minimums and resident-care spending levels. The law requires that nursing homes provide 3.5 hours of care per resident per day by a certified nurse aide, licensed practical nurse, or registered nurse. It also requires that facilities spend 70 percent of revenues on direct resident care and 40 percent of revenue on resident-facing staffing. Read More
North Carolina
Senate Republicans to Propose Medicaid Expansion. Axios reported on May 23, 2022, that North Carolina Senate Republicans are expected to propose legislation to implement Medicaid expansion, which would reach about 600,000 adults. The legislation will also give registered nurses a wider scope of practice, change requirements for providers looking to open practices, establish rules to foster medical billing transparency, and define telehealth. Read More
Oklahoma
Legislature Approves Move to Medicaid Managed Care. Insurance News Net reported on May 24, 2022, that the Oklahoma legislature passed a bill (Senate Bill 1337), which would allow the state to implement elements of the Medicaid managed care proposal favored by Governor Kevin Stitt. The bill would allow the state to issue a request for proposals (RFP) to award capitated contracts to at least three entities, which may include Medicaid managed care plans and provider-led entities like accountable care organizations. Implementation would begin October 1, 2023. Provider-led entities would receive preferential treatment, with at least one targeted to receive a contract. Covered beneficiaries would include traditional Medicaid members and the state’s voter-approved expansion population, but not the aged, blind, and disabled population. The state would issue separate RFPs for a Medicaid dental plan and a Children’s Specialty Plan. The bill awaits signature by Governor Kevin Stitt. Read More
Pennsylvania
Pennsylvania Group Calls for Increase in Medicaid Rates for Long-Term Care Amid Staffing Crisis. Local 21 News reported on May 24, 2022, that the Pennsylvania Health Care Association and some state legislators are calling for a $294 million increase in funding for Medicaid reimbursement rates for long-term care facilities amid a workforce shortage. According to a report by Health Management Associates, more than 1.18 million individuals will require long-term care in Pennsylvania over the next 20 to 30 years. Read More
Rhode Island
Governor Proposes MMIS Modernization Project in Fiscal 2023 Budget. Rhode Island Governor Daniel McKee proposed allocating $28.8 million to transition the state’s current Medicaid management information system (MMIS) to a modular MMIS solution. McKee proposed funds for Medicaid Enterprise System upgrades, including $5.2 million to implement a claims and finance module and $14.3 million for a vendor to aid with the transition to a modular MMIS. An additional $2.4 million will go toward implementing a Medicaid Eligibility and Services Authorization Verification module, and $2.6 million will go toward a Third-Party Liability (TPL) module.
Virginia
Virginia Receives Federal Approval for Reinsurance Program through State Innovation Waiver.
Modern Healthcare reported on May 19, 2022, that Virginia received federal waiver approval for a reinsurance program that will reimburse individual health plans for claims between $40,000 and $155,000 with 70 percent coinsurance. Virginia projects that the Section 1332 State Innovation Waiver, which runs through 2027, will help reduce average individual plan premiums by 15.6 percent in 2023. Anthem, Cigna, and Kaiser are the state’s largest individual plans. Read More
Director of the Department of Medical Assistance Services Steps Down. The Richmond Times-Dispatch reported on May 16, 2022, that Karen Kimsey, director of the Virginia Department of Medical Assistance Services, has stepped down. Cheryl Roberts, deputy director of program and operations, will serve as interim director of the agency. Read More
Washington
Washington Appoints Charissa Fotinos as Medicaid Director. KPVI reported on May 18, 2022, that the Washington Health Care Authority appointed Charissa Fotinos, MD, as Medicaid director. Fotinos has been serving as interim Medicaid director for the past 10 months.
West Virginia
Lawmakers Evaluate Department of Health and Human Resources Ahead of Possible Reorganization. Metro News reported on May 23, 2022, that West Virginian lawmakers continue to evaluate the state’s Department of Health and Human Resources (DHHR) ahead of a possible reorganization. Governor Jim Justice vetoed a bill passed in the 2022 legislative session, which would have divided the agency into two departments. The state is still evaluating vendor applications for an in-depth review of DHHR. Read More
National
House Democrats Push for Extension of Enhanced Exchange Subsidies. Fierce Healthcare reported on May 24, 2022, that House Democrats are calling for an extension of enhanced Affordable Care Act (ACA) Exchange plan subsidies, which are currently set to expire at the end of 2022. Lawmakers also want to close the Medicaid coverage gap in non-expansion states. Read More
U.S. Senate Considers Bipartisan Legislation to Reform PBM Practices. Fierce Healthcare reported on May 24, 2022, that the U.S. Senate is considering bipartisan legislation that would reform pharmacy benefit manager (PBM) practices by eliminating spread pricing, banning PBMs from clawing back payments to pharmacies via direct remuneration fees, and preventing PBMs from unfairly charging pharmacies more to offset federal reimbursement changes. The legislation would also give the Federal Trade Commission and state attorneys general the authority to enforce the new rules. Read More
CMS Enhances Medicaid.gov to Assist Medicaid, CHIP Beneficiaries With Eligibility Redeterminations. The Centers for Medicare & Medicaid Services (CMS) announced on May 24, 2022, that it has added information to the Medicaid.gov website to assist beneficiaries of Medicaid and the Children’s Health Insurance Program (CHIP) with eligibility redeterminations after the public health emergency ends. Features include a Renew Your Medicaid and CHIP page and reminding beneficiaries to update contact information, check their mail, and complete a renewal form. Read More
‘No Surprises Act’ Protected Health Insurance Enrollees from 2 Million Surprise Medicaid Bills in 2 Months, Survey Finds. Modern Healthcare reported on May 24, 2022, that the No Surprises Act shielded commercial health insurance enrollees from an estimated two million surprise bills during the first two months of the year, according to a survey from America’s Health Insurance Plans and the Blue Cross Blue Shield Association. The report projects that the law could prevent more than 12 million surprise bills this year. Read More
U.S. Senators Introduce Bipartisan Legislation to Integrate Care for Dual Eligibles. U.S. Senator Bill Cassidy (R-Louisiana) announced on May 20, 2022, the introduction of the AIM Act, which would require states to develop strategies to integrate and coordinate care for dual eligibles. The legislation, which Cassidy introduced with Senators Tim Scott (R-SC) and Bob Casey (D-PA), would also require that state strategies are approved by the Department of Health and Human Services. Read More
HHS Cannot Mandate That Medicaid ‘Drug Best’ Price Calculations Include Copay Assistance, Judge Rules. Fierce Healthcare reported on May 19, 2022, that the U.S. Department of Health and Human Services (HHS) does not have the authority to mandate that copay assistance programs like coupons and cost-sharing be included in best price calculations for drugs in the Medicaid rebate programs, according to District Court Judge Carl Nichols. Nichols sided with the Pharmaceutical Research and Manufacturers of America (PhRMA), which brought the lawsuit against HHS, claiming the proposed 2020 rule contradicts the federal rebate law. Read More
U.S. House Committee to Consider Bill Requiring Medicaid Coverage of Doula Services. Milwaukee Neighborhood News Service reported on May 19, 2022, that the House Committee on Energy and Commerce will consider a bill that would require state Medicaid programs to cover doula and midwife services, including prenatal and postpartum care. The bill was first introduced by U.S. Representative Gwen Moore (D-WI) in 2019 and referred to the committee in April. Read More
Medicaid Expansion Is Associated with Increased Cancer Survival Rates, Study Finds. Salamanca Press/HealthDay News reported on May 18, 2022, that two-year cancer survival rates in Medicaid expansion states rose to 82.2 percent after expansion (2014-16), up from 80.6 percent before expansion (2010-12), a 160 basis point improvement, according to a study from the American Cancer Society. In non-expansion states, two-year cancer survival rates rose from 78.71 to 80.04 percent, a 133 basis point improvement. Improvement was most pronounced in non-Hispanic Black patients and patients living in rural areas, as well as patients diagnosed with colorectal cancer, lung cancer, non-Hodgkin lymphoma, pancreatic cancer, and liver cancer.
Disability Rights Advocate Julianne Beckett Dies at Age 72. The Gazette reported on May 18, 2022, the death of Julianne Beckett, 72, who helped establish the “Katie Beckett waiver,” which allows Medicaid to pay for the care of individuals with disabilities living at home or in the community. The waiver is named after her daughter Katie, who had contracted viral encephalitis. Read More
71 Percent of Medicaid Members Have Received Information on Medicaid Redeterminations, Survey Finds. Icario Health reported on May 17, 2022, that 71 percent of Medicaid members have received information about Medicaid redetermination or re-enrollment within the past year, according to a survey conducted with Harris Poll. Higher income individuals were more likely to say they had received information. The survey notes, however, that just over half indicated that the information provided was helpful. About 44 percent of those surveyed said email was their preferred form of communication, 40 percent preferred paper mail, and 19 percent preferred a phone call. Read More
Industry News
Enhanced Healthcare Partners Invests in Howard J. Chudler & Associates. Private equity firm Enhanced Healthcare Partners announced on May 24, 2022, an investment in Howard J. Chudler & Associates, a behavioral therapy services provider for individuals with autism and intellectual and developmental disabilities. Read More
VillageMD to Acquire Bandera Family Medical Group. VillageMD announced on May 19, 2022, that it is acquiring Bandera Family Medical Group, a San Antonio-based group of three primary care practices. Eight primary care clinicians and staff will join Village Medical, which provides primary care at free-standing practices and through Walgreens stores. Read More
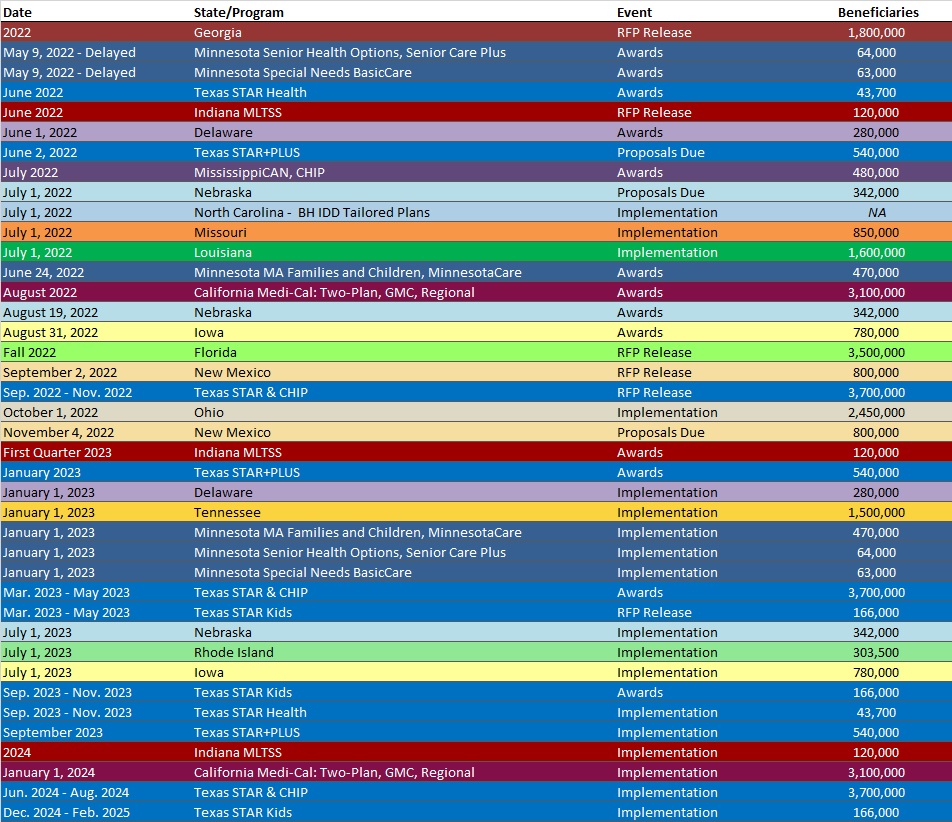
RFP Calendar
HMA News & Events
HMA Welcomes New Colleagues:
Deborah Witham, LMSW, JD
Principal
Washington, D.C.
Debbi Witham is a seasoned executive with experience delivering high quality, mission driven healthcare. During her career, she has focused on behavioral health, including mental health and substance use disorders (SUD), integration of primary and behavioral health services, services for people living with HIV/AIDS, and housing and social services.
She joins HMA after serving as managing director of public policy and opioid treatment programs with CARF International where she oversaw federal policy for all accreditation areas, tracked and monitored policy issues that impact service delivery for accredited services and provided education to policymakers on quality issues. In addition, she oversaw development of standards for opioid treatment programs and served as the liaison to the Substance Abuse Mental Health Services Administration (SAMHSA) Center for Substance Abuse Treatment (CSAT).
Skilled in program design and development, Debbi has worked to create and improve programs aimed at improving access and care in behavioral health and housing systems, including large scale projects aimed at delivery system reform, workforce development and preparing systems for value-based payment.
Debbi is also an experienced compliance, accreditation, and quality improvement expert, leading corporate compliance, and quality improvement programs to build structured strategic plans, implement internal audit procedures, prepare for – and succeed with – accreditations, and develop countermeasures to manage risk exposure, ensure compliance, and improve outcomes. Prior to moving to CARF in a full-time managing director role, Debbi served as a CARF surveyor for the opioid treatment program accreditation area.
She is a licensed social worker with experience delivering services across the lifespan and earned a Juris Doctor from New York Law School. She received her Master of Social Work and a bachelor’s degree, also in social work, from the University of Pittsburgh.
Dina Besirevic, RN, RAC-CT, RAC-CTA, CDONA
Senior Consultant
Chicago, IL
With an extensive background in managed care, Medicare, Medicaid Case Mix, and healthcare policy, and a focus on financial performance, Dina Besirevic is a seasoned healthcare and clinical reimbursement expert.
She joins HMA after serving Villa Healthcare in increasingly senior roles including divisional director of clinical reimbursement. In that role, she increased revenue and Medicare Patient Driven Payment Method (PDPM) use as well as Medicaid Case Mix rates in a number of states over multiple years. She provided leadership across facilities in three states and coordinated efforts around continuing improvement in PDPM. In addition, she provided continuing education to staff and streamlined processes which led to to improved quality measures and outcomes for resident.
During her career, Dina has worked to optimize reimbursement by performing consistent, focused data mining, and implementing change based on those findings. She is also adept at creating and maintaining relationships with healthcare executives and external business partners in order to enhance quality and performance.
Dina is a registered nurse and holds certifications in restorative nursing, resident assessment coordinator-certified advanced nursing, and director of nursing administration. Her clinical experience includes providing hands-on oversight to rehabilitation center operations and restorative nursing programs as well as serving as a charge nurse.
She earned an associate’s degree in science and nursing from Harry S. Truman College in Chicago.
Autumn Carparelli
Senior Consultant
Denver, CO
A skilled data expert, Autumn Carparelli has the know-how and experience to analyze big data in order to understand populations and programs and to improve efficiency, accessibility, and affordability of healthcare. Autumn has experience using datasets from a wide range of sources including Medicare, Medicaid, local and state health departments, and electronic medical records (EMR).
She joins HMA after a position as a population health data scientist with St. Peter’s Health where she led a team of subject matter experts in upgrades and improvements to a clinical decision support tool. In this role, she also mined EMR data to produce visualizations and reports analyzing program cost projections, value-based contract outcomes, and operational and clinical decision support. While there, she also provided useful data to providers so they could better understand the needs and outcomes of their patient population.
Earlier in her career, Autumn gained experience with claims data focused on member care management programs and tribal health with Montana Medicaid. She also has experience with Medicare claims data, using this dataset to glean insights about utilization and quality outcomes.
Autumn’s technical skills include building dashboards and queries to explore trends, developing maps and infographics, and replying to requests from member care management programs, hospitals and health systems, Medicaid agencies, CMS, and other stakeholders.
Autumn earned a Master of Public Health in epidemiology from the University of Nebraska Medical Center and a bachelor’s degree in pre-medicine and environmental studies from the University of Nebraska, Lincoln.
Ruth Danielzuk, MA, MBA, BS, CPHQ
Senior Consultant
Phoenix, AZ
Driven by collaboration across the healthcare landscape, Ruth Danielzuk is a seasoned quality and innovation expert with experience managing programs and projects while optimizing patient safety and improving healthcare quality outcomes.
Before joining HMA, she served as director of risk performance improvement with Acadia Health Care where she led infection control strategies and provided analysis to aide prevention and mitigation factors during the COVID-19 pandemic. She also oversaw, and successfully completed, The Joint Commission survey for preparedness management earning accreditation with a focus on Net Promoter Score goals and best practices in a behavioral health setting.
Ruth has driven performance and quality improvement efforts by developing and implementing hospital and health center innovations, leading to cost savings and cost avoidance while implementing and enforcing best practices to reduce harm to patients. She has led quality improvement teams and achieved Patient Center Medical Home certifications while enhancing patient outcomes and reducing costs through care coordination.
She earned a Master of Business Administration from Saint Thomas University, a Master of Arts in psychology from Bethel University, and a bachelor’s degree in public health, family social science and child psychology from the University of Minnesota.
Ruth is a Certified Professional in Healthcare Quality and a Lean Certified Green Belt. She also completed the Telluride Certificate of Achievement Patient Safety Academy for Emerging Leaders in Patient Safety.
Katie Sherman
Senior Consultant
Austin, TX
An experienced behavioral health professional, Katie Sherman has served in clinical and administrative roles with public, private, and governmental organizations within the behavioral health, substance use disorder (SUD), healthcare integration and operational management spaces.
She joins HMA after serving as vice president of international drug policy with The Levenson Foundation where she developed models of care to increase revenue streams and improve access to quality behavioral health and harm reduction services. She also identified and executed funding opportunities for services in addition to consulting and collaborating with partners on changes in international drug policy law and their impacts.
An expert in SUD and medication assisted treatment (MAT), Katie previously had statewide oversight of MAT services in the state of Texas. In this role, she developed policy, oversaw procurement and contracting services as well as capacity growth and quality management for providers and populations with opioid use disorders.
Katie has experience utilizing data and metrics to evaluate and improve programs and assess service delivery, target audience outcomes and financial operations. She has provided project oversight, cross agency coordination, strategic development, and process improvement to agencies and organizations while securing grant funding, meeting federal CMS and state agency regulations, and improving care and workflows to partners and stakeholders.
In her spare time, Katie harnesses her passion for MAT advocacy by co-facilitating trainings to empower peer support services in Medication Assisted Recovery.
New This Week On HMA Information Services (HMAIS):
Medicaid Data
- Mississippi Medicaid Managed Care Enrollment is Down 8.3%, Apr-22 Data
- Missouri SNP Membership at 73,076, Mar-22 Data
- Nebraska Medicaid Managed Care Enrollment Is Up 1.5%, Jan-22 Data
- South Carolina Dual Demo Enrollment is Down 5.4%, Nov-21 Data
- South Carolina Medicaid Managed Care Enrollment is Up 9.4%, Nov-21 Data
- Texas Dual Demo Enrollment is 35,525, Feb-22 Data
- Texas Medicaid Managed Care Enrollment is Up 2%, Feb-22 Data
- Utah Medicaid Managed Care Enrollment is Up 14.8%, Nov-21 Data
- Virginia Medicaid Managed Care Enrollment is Up 11.5%, Oct-21 Data
- Virginia Medicaid MLTSS Enrollment is Up 6.1%, Oct-21 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Colorado Healthcare Billing, Data Collection, Reporting, and Analysis RFP, May-22
- Minnesota Medicaid Managed Care Plan Financials, 2017-21
- Minnesota Medicaid Managed Care Model Contracts, 2022
- Minnesota Medicaid Managed Care Organization (MCO) Contracts, 2022
- Tennessee Dual Eligibles LTSS Program Planning Assistance RFI, May-22
Medicaid Program Reports, Data and Updates:
- California Medi-Cal Managed Care External Quality Review Reports, 2013-21
- Illinois Medicaid Annual Reports, 2013-21
- Illinois Medical Programs External Quality Review Annual Reports, FY 2012-21
- Iowa Medical Assistance Advisory Council Meeting Materials, 2016-22
- Louisiana Medicaid Quality Committee Meeting Materials, May-22
- Michigan Dental Health Plans External Quality Review Technical Reports, 2020-21
- Michigan Medicaid Health Plan External Quality Review Reports, FY 2014-21
- Minnesota DHS EQR Annual Technical Reports, 2016-20
- New Jersey Medical Assistance Advisory Council Meeting Materials, Apr-22
- Texas Coordinated Statewide Behavioral Health Expenditure Proposals, FY 2020-22
- Texas Housing Choice Plan Report, May-22
- Texas Quarterly Reports from the HHS Ombudsman Managed Care Assistance Team, FY 2019-22
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
